Structure and Functions of the Autonomic Nervous System/The autonomic nervous system (ANS), formerly the vegetative nervous system, is a division of the peripheral nervous system that supplies smooth muscle and glands, and thus influences the function of internal organs.[rx] The autonomic nervous system is a control system that acts largely unconsciously and regulates bodily functions, such as the heart rate, digestion, respiratory rate, pupillary response, urination, and sexual arousal.[rx] This system is the primary mechanism in control of the fight-or-flight response.
Preganglionic Neurons
In the autonomic nervous system (ANS), nerve fibers that connect the central nervous system to ganglia are known as preganglionic fibers.
Key Points
All preganglionic fibers of the ANS are cholinergic —meaning they have acetylcholine as their neurotransmitter and are myelinated for faster transmission.
Differences between sympathetic and parasympathetic preganglionic fibers include that sympathetic preganglionic fiber tend to be shorter than parasympathetic fibers and sympathetic fibers tend to form more synapses than parasympathetic fibers.
The parasympathetic division (craniosacral outflow) consists of cell bodies from one of two locations: the brainstem (cranial nerves III, VII, IX, X) or the sacral spinal cord (S2, S3, S4).
The sympathetic division (thoracolumbar outflow) consists of cell bodies in the lateral horn of the spinal cord (intermediolateral cell columns) from T1 to L2. These cell bodies are GVE (general visceral efferent ) neurons and are the preganglionic neurons.
Key Terms
cholinergic: Pertaining to, activated by, producing, or having the same function as acetylcholine.
postsynaptic neuron: The nerve cell that bears receptors for neurotransmitters released into the synaptic cleft by the presynaptic neuron.
preganglionic fiber: In the autonomic nervous system, fibers from the CNS to the ganglion are known as preganglionic fibers.
ganglion: A cluster of interconnecting nerve cells outside the brain.
preganglionic neuron: The nerve fibers that supply a ganglion.
Preganglionic Neuron Properties
In the autonomic nervous system (ANS), fibers from the central nervous system to the ganglion are known as preganglionic fibers. All preganglionic fibers, whether they are in the sympathetic nervous system (SNS) or in the parasympathetic nervous system (PSNS), are cholinergic—that is, these fibers use acetylcholine as their neurotransmitter—and are myelinated.
The ANS is unique in that it requires a sequential two-neuron efferent pathway; the preganglionic neuron must first cross a synapse onto a postganglionic neuron before innervating the target organ. The preganglionic, or first neuron will begin at the outflow and will cross a synapse at the postganglionic, or second neuron’s cell body. The postganglionic neuron will then cross a synapse at the target organ.
Sympathetic preganglionic fibers tend to be shorter than parasympathetic preganglionic fibers because sympathetic ganglia are often closer to the spinal cord while parasympathetic preganglionic fibers tend to project to and synapse with the postganglionic fiber close to the target organ.
Outflow Sites
Properties of the SNS and PSNS preganglionic neurons also differ with respect to the spinal cord exit points. The sympathetic division has thoracolumbar outflow, meaning that the neurons begin at the thoracic and lumbar (T1–L2) portions of the spinal cord. The parasympathetic division has craniosacral outflow, meaning that the neurons begin at the cranial nerves (CN3, CN7, CN9, CN10) and sacral (S2–S4) spinal cord.
The sympathetic division (thoracolumbar outflow) consists of cell bodies in the lateral horn of the spinal cord (intermediolateral cell columns) from T1 to L2. These cell bodies are GVE (general visceral efferent) neurons and are the preganglionic neurons. There are several locations where preganglionic neurons create synapses with their postganglionic neurons:
- The paravertebral ganglia of the sympathetic chain (these run on either side of the vertebral bodies), cervical ganglia, thoracic ganglia, rostral lumbar ganglia, caudal lumbar ganglia, and pelvic ganglia.
- The prevertebral ganglia celiac ganglion, aorticorenal ganglion, superior mesenteric ganglion, inferior mesenteric ganglion.
- The chromaffin cells of the adrenal medulla. This is the one exception to the two-neuron pathway rule: they create a synapse directly onto the target cell bodies.
The parasympathetic division (craniosacral outflow) consists of cell bodies from one of two locations: the brainstem (cranial nerves III, VII, IX, X) or the sacral spinal cord (S2, S3, S4).
These are the preganglionic neurons that synapse with the postganglionic neurons in these locations:

Parasympathetic ganglia of the head: The parasympathetic division has craniosacral outflow, meaning that the neurons begin at the cranial nerves (CN3, CN7, CN9, CN10) and the sacral (S2–S4) spinal cord. Pre- and post-ganglionic fibers and targets are depicted.
- Parasympathetic ganglia of the head (ciliary (CN III)).
- Submandibular (CN VII).
- Pterygopalatine (CN VII).
- Otic (CN IX)).
- In or near the wall of an organ innervated by the vagus (CN X) or sacral nerves (S2, S3, S4).
Divergence
Another major difference between the two ANS systems is divergence or the number of postsynaptic fibers a single preganglionic fiber creates a synapse with. Whereas in the parasympathetic division there is a divergence factor of roughly 1:4, in the sympathetic division there can be a divergence of up to 1:20.
The site of synapse formation and this divergence for both the sympathetic and parasympathetic preganglionic neurons do, however, occur within ganglia situated within the peripheral nervous system.
Autonomic Ganglia
Autonomic ganglia are clusters of neuron cell bodies that transmit sensory signals from the periphery to the integration centers in the CNS.
Key Points
Autonomic ganglia can be classified as either sympathetic ganglia and parasympathetic ganglia.
A dorsal root ganglion (or spinal ganglion) is a nodule on a dorsal root of the spine that contains the cell bodies of nerve cells ( neurons ) that carry signals from sensory organs to the appropriate integration center.
Sympathetic ganglia deliver information to the body about stress and impending danger, and are responsible for the familiar fight-or-flight response. They contain approximately 20,000–30,000 nerve cell bodies and are located close to and on either side of the spinal cord in long chains.
The axons of dorsal root ganglion neurons are known as afferents. In the peripheral nervous system, afferents refer to the axons that relay sensory information into the central nervous system (i.e., the brain and the spinal cord).
Key Terms
sympathetic ganglion: The ganglia of the sympathetic nervous system. They deliver information to the body about stress and impending danger, and are responsible for the familiar fight-or-flight response.
dorsal root ganglia: A dorsal root ganglion (or spinal ganglion) is a nodule on a dorsal root of the spine that contains the cell bodies of nerve cells (neurons) that carry signals from sensory organs toward the appropriate integration center.
parasympathetic ganglion: The autonomic ganglia of the parasympathetic nervous system. Most are small terminal ganglia or intramural ganglia, so named because they lie near or within (respectively) the organs they innervate.
Autonomic ganglia are clusters of neuronal cell bodies and their dendrites. They are essentially a junction between autonomic nerves originating from the central nervous system and autonomic nerves innervating their target organs in the periphery.
The dorsal root ganglia lie along the vertebral column by the spine and develop in the embryo from neural crest cells, not neural tube. Therefore, the spinal ganglia can be regarded as a gray matter of the spinal cord that became translocated to the periphery.
The two main categories are sympathetic ganglia and parasympathetic ganglia. An example of a parasympathetic ganglion is the ciliary ganglion, involved in pupil constriction and accommodation. A depiction of all the parasympathetic ganglia in the head and neck is shown in the following illustration.

Ciliary ganglion: The pathways of the ciliary ganglion include sympathetic neurons (red), parasympathetic neurons (green), and sensory neurons (blue).
Parasympathetic ganglia of the head: Parasympathetic ganglia of the head (shown as red circles) help supply all parasympathetic innervation to the head and neck.

Anatomy of an autonomic ganglion: The sympathetic connections of the ciliary and superior cervical ganglia are shown in this diagram. The postganglionic fibers travel from the ganglion to the effector organ.
Dorsal Root Ganglia
A dorsal root ganglion (or spinal ganglion) is a nodule on a dorsal root of the spine that contains the cell bodies of nerve cells (neurons) that carry signals from the sensory organs towards the appropriate integration center.
Nerves that carry signals towards the brain are known as afferent nerves. The axons of dorsal root ganglion neurons are known as afferents. In the peripheral nervous system, afferents refer to the axons that relay sensory information into the central nervous system (i.e., the brain and the spinal cord).
These neurons are of the pseudo-unipolar type, meaning they have an axon with two branches that act as a single axon, often referred to as a distal process and a proximal process.
Unlike the majority of neurons found in the central nervous system, an action potential in a dorsal root ganglion neuron may initiate in the distal process in the periphery, bypass the cell body, and continue to propagate along the proximal process until reaching the synaptic terminal in the dorsal horn of the spinal cord.
The distal section of the axon may either be a bare nerve ending or encapsulated by a structure that helps relay specific information to a nerve. The nerve endings of dorsal root ganglion neurons have a variety of sensory receptors that are activated by mechanical, thermal, chemical, and noxious stimuli.
In these sensory neurons, a group of ion channels thought to be responsible for somatosensory transduction have been identified. For example, a Meissner’s corpuscle or Pacinian corpuscle may encapsulate the nerve ending, rendering the distal process sensitive to mechanical stimulation, such as stroking or vibration, respectively.
Sympathetic Ganglia
Sympathetic ganglia are the ganglia of the sympathetic nervous system. They deliver information to the body about stress and impending danger and are responsible for the familiar fight-or-flight response. They contain approximately 20,000–30,000 nerve cell bodies and are located close to and on either side of the spinal cord in long chains.
Sympathetic ganglia are the tissue from which neuroblastoma tumors arise. The bilaterally symmetric sympathetic chain ganglia —also called the paravertebral ganglia —are located just ventral and lateral to the spinal cord. The chain extends from the upper neck down to the coccyx, forming the unpaired coccygeal ganglion.
Preganglionic nerves from the spinal cord create a synapse end at one of the chain ganglia, and the postganglionic fiber extends to an effector, typically a visceral organ in the thoracic cavity. There are usually 21 or 23 pairs of these ganglia: three in the cervical region, 12 in the thoracic region, four in the lumbar region, four in the sacral region, and a single, unpaired ganglion lying in front of the coccyx called the ganglion impair.
Neurons of the collateral ganglia also called the prevertebral ganglia, receive input from the splanchnic nerves and innervate organs of the abdominal and pelvic region. These include the celiac ganglia, superior mesenteric ganglia, and inferior mesenteric ganglia.
Parasympathetic Ganglia
Parasympathetic ganglia are the autonomic ganglia of the parasympathetic nervous system. Most are small terminal ganglia or intramural ganglia, so named because they lie near or within (respectively) the organs they innervate. The exceptions are the four paired parasympathetic ganglia of the head and neck.
Efferent parasympathetic nerve signals are carried from the central nervous system to their targets by a system of two neurons. The first neuron in this pathway is referred to as the preganglionic or presynaptic neuron. Its cell body sits in the central nervous system and its axon usually extends to a ganglion somewhere else in the body, where it synapses with the dendrites of the second neuron in the chain.
This second neuron is referred to as the postganglionic or postsynaptic neuron. The axons of presynaptic parasympathetic neurons are usually long. They extend from the CNS into a ganglion that is either very close to or embedded in their target organ. As a result, the postsynaptic parasympathetic nerve fibers are very short.
Postganglionic Neurons
In the autonomic nervous system, fibers from the ganglion to the effector organ are called postganglionic fibers.
Key Points
Postganglionic fibers in the sympathetic division are adrenergic and use norepinephrine (also called noradrenaline) as a neurotransmitter. By contrast, postganglionic fibers in the parasympathetic division are cholinergic and use acetylcholine as a neurotransmitter.
In the sympathetic nervous system, the postganglionic neurons of sweat glands release acetylcholine for the activation of muscarinic receptors.
Chromaffin cells of the adrenal medulla are analogous to post-ganglionic neurons; the adrenal medulla develops in tandem with the sympathetic nervous system and acts as a modified sympathetic ganglion.
In the sympathetic nervous system, presynaptic nerves ‘ axons terminate in either the paravertebral ganglia or prevertebral ganglia. In all cases, the axon enters the paravertebral ganglion at the level of its originating spinal nerve.
Key Terms
postganglionic fiber: In the autonomic nervous system, these are the fibers that run from the ganglion to the effector organ.
cholinergic: Pertaining to, activated by, producing, or having the same function as acetylcholine.
adrenergic: Containing or releasing adrenaline.
postganglionic neuron: A nerve cell that is located distal or posterior to a ganglion.
In the autonomic nervous system, fibers from the ganglion to the effector organ are called postganglionic fibers. The post-ganglionic neurons are directly responsible for changes in the activity of the target organ via biochemical modulation and neurotransmitter release.
The neurotransmitters used by postganglionic fibers differ. In the parasympathetic division, they are cholinergic and use acetylcholine as their neurotransmitter. In the sympathetic division, most are adrenergic, meaning they use norepinephrine as their neurotransmitter.

Postganglionic nerve fibers: In the autonomic nervous system, preganglionic fibers (shown in light blue) carry information from the CNS to the ganglion.
The Sympathetic Fibers
At the synapses within the ganglia, the preganglionic neurons release acetylcholine, a neurotransmitter that activates nicotinic acetylcholine receptors on postganglionic neurons. In response to this stimulus, postganglionic neurons—with two important exceptions—release norepinephrine, which activates adrenergic receptors on the peripheral target tissues. The activation of target tissue receptors causes the effects associated with the sympathetic system.
The two exceptions mentioned above are the postganglionic neurons of sweat glands and the chromaffin cells of the adrenal medulla. The postganglionic neurons of sweat glands release acetylcholine for the activation of muscarinic receptors. The chromaffin cells of the adrenal medulla are analogous to post-ganglionic neurons—the adrenal medulla develops in tandem with the sympathetic nervous system and acts as a modified sympathetic ganglion. Within this endocrine gland, the pre-ganglionic neurons create synapses with chromaffin cells and stimulate the chromaffin cells to release norepinephrine and epinephrine directly into the blood.
Presynaptic nerves’ axons terminate in either the paravertebral ganglia or prevertebral ganglia. In all cases, the axon enters the paravertebral ganglion at the level of its originating spinal nerve.
After this, it can then either create a synapse in this ganglion, ascend to a more superior ganglion, or descend to a more inferior paravertebral ganglion and make a synapse there, or it can descend to a prevertebral ganglion and create a synapse there with the postsynaptic cell. The postsynaptic cell then goes on to innervate the targeted end effector (i.e., gland, smooth muscle, etc.).
Because paravertebral and prevertebral ganglia are relatively close to the spinal cord, presynaptic neurons are generally much shorter than their postsynaptic counterparts, which must extend throughout the body to reach their destinations.
The Parasympathetic Fibers
The axons of presynaptic parasympathetic neurons are usually long. They extend from the CNS into a ganglion that is either very close to or embedded in their target organ. As a result, the postsynaptic parasympathetic nerve fibers are very short.
In the cranium, preganglionic fibers (cranial nerves III, VII, and IX) usually arise from specific nuclei in the central nervous system (CNS) and create a synapse at one of four parasympathetic ganglia: ciliary, pterygopalatine, otic, or submandibular.
From these four ganglia the postsynaptic fibers complete their journey to target tissues via cranial nerve V (the trigeminal ganglion with its ophthalmic, maxillary, and mandibular branches).
The vagus nerve does not participate in these cranial ganglia, as most of its fibers are destined for a broad array of ganglia on or near the thoracic viscera (esophagus, trachea, heart, lungs) and the abdominal viscera (stomach, pancreas, liver, kidneys). It travels all the way down to the midgut/hindgut junction, which occurs just before the splenic flexure of the transverse colon.
The pelvic splanchnic efferent preganglionic nerve cell bodies reside in the lateral gray horn of the spinal cord at the S2–S4 spinal levels. Their axons continue away from the CNS to synapse at an autonomic ganglion close to the organ of innervation. This differs from the sympathetic nervous system, where synapses between pre- and post-ganglionic efferent nerves in general occur at ganglia that are farther away from the target organ.
The parasympathetic nervous system uses acetylcholine (ACh) as its chief neurotransmitter, although peptides (such as cholecystokinin) may act on the PSNS as a neurotransmitter. The ACh acts on two types of receptors, the muscarinic and nicotinic cholinergic receptors.
Most transmissions occur in two stages: When stimulated, the preganglionic nerve releases ACh at the ganglion, which acts on the nicotinic receptors of the postganglionic neurons. The postganglionic nerve then releases ACh to stimulate the muscarinic receptors of the target organ.
Autonomic Plexuses
Autonomic plexuses are formed from sympathetic and parasympathetic fibers that innervate and regulate the overall activity of visceral organs.
Key Points
The autonomic plexuses include the cardiac plexus, the pulmonary plexus, the esophageal plexus, the abdominal aortic plexus, and the superior and inferior hypogastric plexuses.
Autonomic plexuses are formed from sympathetic postganglionic axons, parasympathetic preganglionic axons, and some visceral sensory axons.
Plexuses provide a complex innervation pattern to the target organs since most organs are innervated by both divisions of the autonomic nervous system.
Key Terms
autonomic plexus: Any of the extensive networks of nerve fibers and cell bodies associated with the autonomic nervous system that are found in the thorax, abdomen, and pelvis, and that contain sympathetic, parasympathetic, and visceral afferent fibers.
abdominal aortic plexus: This is formed by branches derived, on either side, from the celiac plexus and ganglia, and receives filaments from some of the lumbar ganglia. It is situated upon the sides and front of the aorta, between the origins of the superior and inferior mesenteric arteries.
pulmonary plexus: An autonomic plexus formed from the pulmonary branches of the vagus nerve and the sympathetic trunk. It supplies the bronchial tree and the visceral pleura.
Autonomic plexuses are formed from sympathetic postganglionic axons, parasympathetic preganglionic axons, and some visceral sensory axons. The nerves in each plexus are close to each other, as in the plexuses of the somatic nervous system, but typically do not interact or synpase together.

Sympathetic trunk: This section of the sympathetic trunk shows both the celiac and the hypogastric plexus.
Instead, they provide a complex innervation pattern to the target organs, since most organs are innervated by both divisions of the autonomic nervous system. The autonomic plexuses include the cardiac plexus, the pulmonary plexus, the esophageal plexus, and the abdominal aortic plexus, and the superior and inferior hypogastric plexuses.
Plexuses
Cardiac
The cardiac plexus is a plexus of nerves situated at the base of the heart that innervates the heart. The superficial part of the cardiac plexus lies beneath the arch of the aorta, in front of the right pulmonary artery. It is formed by the superior cardiac branch of the left sympathetic trunk and the lower superior cervical cardiac branch of the left vagus nerve. A small ganglion, the cardiac ganglion of Wrisberg, is occasionally found connected with these nerves at their point of junction.
Pulmonary
The pulmonary plexus is an autonomic plexus formed from pulmonary branches of vagus nerve and the sympathetic trunk. It supplies the bronchial tree and the visceral pleura.
Esophageal
The esophageal plexus is formed by nerve fibers from two sources: the branches of the vagus nerve and the visceral branches of the sympathetic trunk. The esophageal plexus and the cardiac plexus contain the same types of fibers and are both considered thoracic autonomic plexus(es).
Abdominal
The abdominal aortic plexus is formed by branches derived, on either side, from the celiac plexus and ganglia, and receives filaments from some of the lumbar ganglia. It is situated on the sides and front of the aorta, between the origins of the superior and inferior mesenteric arteries.
From this plexus arise parts of the spermatic, the inferior mesenteric, and the hypogastric plexuses; it also distributes filaments to the inferior vena cava.
Superior Hypogastric Plexus
The superior hypogastric plexus (in older texts, hypogastric plexus or presacral nerve) is a plexus of nerves situated on the vertebral bodies below the bifurcation of the abdominal aorta.
Inferior Hypogastric Plexus
The inferior hypogastric plexus (pelvic plexus in some texts) is a plexus of nerves that supplies the viscera of the pelvic cavity. The inferior hypogastric plexus is a paired structure, with each situated on the side of the rectum in the male, and at the sides of the rectum and vagina in the female.
Parasympathetic (Craniosacral) Division
Parasympathetic ganglia are the autonomic ganglia of the parasympathetic nervous system that lie near or within the organs they innervate.
Key Points
Each PSNS ganglion has three roots: a motor root, a sympathetic root, and a sensory root, as well as a number of existing branches.
Most are small terminal ganglia or intramural ganglia, so named because they lie near or within the organs they innervate.
The parasympathetic system is referred to as having craniosacral outflow because of the location of PSNS fiber origins.
Key Terms
lacrimal gland: One of a pair of almond-shaped glands, one for each eye, that secrete the aqueous layer of the tear film.
sympathetic root: This carries postsynaptic sympathetic fibers that traverse the ganglion without crossing a synapse.
motor root: This carries presynaptic parasympathetic nerve fibers that terminate in the ganglion and create synapses for the postsynaptic fibers to travel to their target organs.
sensory root: The proximal end of a dorsal afferent nerve that is attached to the spinal cord.
parasympathetic: Relating to the part of the autonomic nervous system that inhibits or opposes the effects of the sympathetic nervous system.
EXAMPLES
Nerves that supply parasympathetic fibers to the parasympathetic ganglia of the head include the oculomotor nerve (ciliary ganglion); the facial nerve (pterygopalatine ganglion, submandibular ganglion); the glossopharyngeal nerve (otic ganglion); the vagus nerve (no named ganglion); and the pelvic splanchnic nerves (no named ganglion).
Parasympathetic ganglia are the autonomic ganglia of the parasympathetic nervous system, blue fibers). Most are small terminal ganglia or intramural ganglia, so named because they lie near or within (respectively) the organs they innervate.
The exceptions are the four paired parasympathetic ganglia of the head and neck. These paired ganglia supply all parasympathetic innervation to the head and neck: ciliary ganglion (spincter pupillae, ciliary muscle), pterygopalatine ganglion (lacrimal gland, glands of nasal cavity), submandibular ganglion (submandibular and sublingual glands), and otic ganglion (parotid gland).

Nerve innervation of the autonomic nervous system: The parasympathetic nervous system, shown in blue, is a division of the autonomic nervous system.
Each has three roots entering the ganglion (motor, sympathetic, and sensory roots) and a variable number of exiting branches.
- The motor root carries presynaptic parasympathetic nerve fibers (general visceral efferent fibers) that terminate in the ganglion by creating a synapse for the postsynaptic fibers traveling to target organs.
- The sympathetic root carries postsynaptic sympathetic fibers (general visceral efferent fibers) that traverse the ganglion without creating a synapse.
- The sensory root carries general sensory fibers (general somatic afferent fibers) that also do not create a synapse in the ganglion.
Some ganglia also carry special sensory fibers (special visceral afferent) for taste sensation.
The nerves that supply parasympathetic fibers to the parasympathetic ganglia of the head include the oculomotor nerve (ciliary ganglion), the facial nerve (pterygopalatine ganglion, submandibular ganglion), the glossopharyngeal nerve (otic ganglion), the vagus nerve, and the pelvic splanchnic nerves.
Because of its location, the parasympathetic system is commonly referred to as having craniosacral outflow, in contrast to the sympathetic nervous system, which is said to have thoracolumbar outflow.

Parasympathetic ganglia of the head: The parasympathetic division has craniosacral outflow, meaning that the neurons begin at the cranial nerves (CN3, CN7, CN9, CN10) and the sacral spinal cord (S2–S4). Pre- and post-ganglionic fibers and targets are depicted.
Sympathetic Nervous System
Sympathetic ganglia are the ganglia of the sympathetic nervous system that initiate fight-or-flight, stress-mediated responses.
Key Points
The bilaterally symmetric sympathetic chain ganglia, also called the paravertebral ganglia, extend from the upper neck down to the coccyx, lateral and slightly ventral to the vertebral column.
Most sympathetic ganglia are bilaterally symmetric, but an example of an unpaired ganglion, called the ganglion impar is present in front of the coccyx.
The sympathetic nervous system is said to have thoracolumbar outflow based on the proximity of the ganglia to the corresponding thoracic and lumbar vertebrae.
Key Terms
paravertebral ganglia: Located along the length of the sympathetic trunk, these ganglia are designated as cervical, thoracic, lumbar, and sacral and, except in the neck, closely correspond in number to the vertebrae.
fight or flight: All the coordinated physiological responses that the sympathetic nervous system initiates in response to stress or other emergency situations.
sympathetic chain ganglia: Also called the paravertebral ganglia, these are located just ventral and lateral to the spinal cord. The chain extends from the upper neck down to the coccyx, forming the unpaired coccygeal ganglion.

Nerve innervation of the autonomic nervous system: The parasympathetic nervous system, shown in blue, is a division of the autonomic nervous system.
The sympathetic ganglia are the ganglia of the sympathetic nervous system (the red lines in the diagram below). They deliver information to the body about stress and impending danger and are responsible for the familiar fight-or-flight response.
This response is also known as the sympathetic-adrenal response because the pre-ganglionic sympathetic fibers that end in the adrenal medulla—like all sympathetic fibers—secrete acetylcholine. This secretion activates the secretion of adrenaline (epinephrine) and to a lesser extent noradrenaline (norepinephrine) from the adrenal medulla.
Therefore, this response is mediated directly via impulses transmitted through the sympathetic nervous system, and indirectly via catecholamines secreted from the adrenal medulla, and acts primarily on the cardiovascular system.
An example of a sympathetic ganglion in a thoracic nerve is shown in. ganglia contain approximately 20000–30000 nerve cell bodies and are located close to and on either side of the spinal cord in long chains. Sympathetic ganglia are the tissue from which neuroblastoma tumors arise.
The bilaterally symmetric sympathetic chain ganglia, also called the paravertebral ganglia, are located just ventral and lateral to the spinal cord. The chain extends from the upper neck down to the coccyx, forming the unpaired coccygeal ganglion.
Preganglionic nerves from the spinal cord create a synapse at one end of the chain ganglia and the postganglionic fiber extends to an effector, typically a visceral organ, in the thoracic cavity. There are usually 21 or 23 pairs of these ganglia: 3 in the cervical region, 12 in the thoracic region, 4 in the lumbar region, 4 in the sacral region, and a single, unpaired ganglion lying in front of the coccyx called the ganglion impair.

Sympathetic ganglion: This intercostal nerve shows the sympathetic ganglion at the top left.
Neurons of the collateral ganglia also called the prevertebral ganglia, receive input from the splanchnic nerves and innervate organs of the abdominal and pelvic region. These include the celiac ganglia, the superior mesenteric ganglia, and the inferior mesenteric ganglia.
The sympathetic nervous system is said to have thoracolumbar outflow based on its location.
Autonomic Reflexes
Autonomic reflexes are unconscious motor reflexes relayed from the organs and glands to the CNS through visceral afferent signaling.
Key Points
While the unconscious reflex arcs are normally undetectable, in certain instances they may trigger pain, typically masked as referred pain.
The sympathetic nervous system is a quick-response, mobilizing system while the parasympathetic system is a more slowly activated, dampening system—but there are exceptions, such as in sexual arousal and orgasm where both systems play a role.
Within the brain, the ANS is located in the medulla oblongata in the lower brainstem. The medulla’s major ANS functions include respiration, cardiac regulation, vasomotor activity, and certain reflex actions (such as coughing, sneezing, vomiting, and swallowing).
Key Terms
reflex arc: A neural pathway that controls an action reflex. There are two types of reflex arcs: the autonomic reflex arc that affects the inner organs, and the somatic reflex arc that affects muscles.
referred pain: Pain perceived at a location other than the site of the painful stimulus.
somatic: Part of, or relating to, the body of an organism.
EXAMPLES
An example of referred pain from an autonomic reflex arc occurs when the bowel is suddenly distended. In these cases, the body will interpret the afferent pain stimulus as somatic.
The Autonomic Nervous System
The autonomic nervous system (ANS, visceral nervous system, or involuntary nervous system) is the part of the peripheral nervous system that acts as a control system. It functions largely below the level of consciousness and controls visceral functions.
The ANS affects heart rate, digestion, respiratory rate, salivation, perspiration, pupillary dilation, micturition (urination), and sexual arousal. Most autonomic functions are involuntary but a number of ANS actions can work alongside some degree of conscious control. Everyday examples include breathing, swallowing, and sexual arousal, and in some cases functions such as heart rate.
Functions
Within the brain, the ANS is located in the medulla oblongata in the lower brainstem. The medulla’s major ANS functions include respiration (the respiratory control center, or RCC), cardiac regulation (the cardiac control center, or CCC), vasomotor activity (the vasomotor center or VMC), and certain reflex actions (such as coughing, sneezing, vomiting, and swallowing).
These then subdivide into other areas and are also linked to ANS subsystems and nervous systems external to the brain. The hypothalamus, just above the brain stem, acts as an integrator for autonomic functions, receiving ANS regulatory input from the limbic system to do so.
Classifications
The ANS is classically divided into two subsystems: the parasympathetic nervous system (PSNS) and sympathetic nervous system (SNS) that operate independently in some functions and interact co-operatively in others. In many cases, the two have opposite actions. When one activates a physiological response, the other inhibits it.
An older simplification of the sympathetic and parasympathetic nervous systems as excitatory and inhibitory was overturned due to the many exceptions found. A more modern characterization is that the sympathetic nervous system is a quick-response, mobilizing system and the parasympathetic is a more slowly activated, dampening system—but there are exceptions, such as in sexual arousal and orgasm where both play a role.
The enteric nervous system is also sometimes considered part of the autonomic nervous system, and sometimes considered an independent system.
The ANS is unique in that it requires a sequential two-neuron efferent pathway; the preganglionic neuron must first create a synapse to a postganglionic neuron before innervating the target organ. The preganglionic, or first neuron will begin at the outflow and will cross a synapse at the postganglionic, or second neuron’s cell body. The postganglionic neuron will then create a synapse at the target organ.
General visceral afferent sensations are mostly unconscious, visceral motor reflex sensations from hollow organs and glands that are transmitted to the CNS (see the following illustration for a depiction of a typical nerve fiber, including general visceral afferent fibers).
While the unconscious reflex arcs are normally undetectable, in certain instances they may send pain sensations to the CNS, masked as referred pain. If the peritoneal cavity becomes inflamed or if the bowel is suddenly distended, the body will interpret the afferent pain stimulus as somatic in origin. This pain is usually non-localized. The pain is usually referred to as dermatomes that are at the same spinal nerve level as the visceral afferent synapse.
Innervation
Autonomic nerves travel to organs throughout the body. Most organs receive parasympathetic supply by the vagus nerve and sympathetic supply by splanchnic nerves. The sensory part of the latter reaches the spinal column at certain spinal segments. Pain in any internal organ is perceived as referred pain, more specifically as pain from the dermatome corresponding to the spinal segment.[rx]
| Organ | Nerves[rx] | Spinal column origin[rx] |
|---|---|---|
| stomach |
|
T5, T6, T7, T8, T9, sometimes T10 |
| duodenum |
|
T5, T6, T7, T8, T9, sometimes T10 |
| jejunum and ileum |
|
T5, T6, T7, T8, T9 |
| spleen |
|
T6, T7, T8 |
| gallbladder and liver |
|
T6, T7, T8, T9 |
| colon |
|
|
| pancreatic head |
|
T8, T9 |
| appendix |
|
T10 |
| kidneys and ureters |
|
T11, T12 |
Function
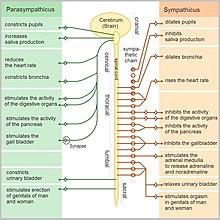
Function of the autonomic nervous system [rx]
Sympathetic and parasympathetic divisions typically function in opposition to each other. But this opposition is better termed complementary in nature rather than antagonistic. For an analogy, one may think of the sympathetic division as the accelerator and the parasympathetic division as the brake. The sympathetic division typically functions in actions requiring quick responses. The parasympathetic division functions with actions that do not require immediate reaction. The sympathetic system is often considered the “fight or flight” system, while the parasympathetic system is often considered the “rest and digest” or “feed and breed” system.
However, many instances of sympathetic and parasympathetic activity cannot be ascribed to “fight” or “rest” situations. For example, standing up from a reclining or sitting position would entail an unsustainable drop in blood pressure if not for a compensatory increase in the arterial sympathetic tonus. Another example is the constant, second-to-second, modulation of heart rate by sympathetic and parasympathetic influences, as a function of the respiratory cycles. In general, these two systems should be seen as permanently modulating vital functions, in usually antagonistic fashion, to achieve homeostasis. Higher organisms maintain their integrity via homeostasis which relies on negative feedback regulation which, in turn, typically depends on the autonomic nervous system.[rx] Some typical actions of the sympathetic and parasympathetic nervous systems are listed below.[15]
| Target organ/system | Parasympathetic | Sympathetic |
|---|---|---|
| Digestive system | Increase peristalsis and amount of secretion by digestive glands | Decrease activity of digestive system |
| Liver | No effect | Causes glucose to be released to blood |
| Lungs | Constricts bronchioles | Dilates bronchioles |
| Urinary bladder/ Urethra | Relaxes sphincter | Constricts sphincter |
| Kidneys | No effects | Decrease urine output |
| Heart | Decreases rate | Increase rate |
| Blood vessels | No effect on most blood vessels | Constricts blood vessels in viscera; increase BP |
| Salivary and Lacrimal glands | Stimulates; increases production of saliva and tears | Inhibits; result in dry mouth and dry eyes |
| Eye (iris) | Stimulates constrictor muscles; constrict pupils | Stimulate dilator muscle; dilates pupils |
| Eye (ciliary muscles) | Stimulates to increase bulging of lens for close vision | Inhibits; decrease bulging of lens; prepares for distant vision |
| Adrenal Medulla | No effect | Stimulate medulla cells to secrete epinephrine and norepinephrine |
| Sweat gland of skin | No effect | Stimulate to produce perspiration |
Sympathetic nervous system
Promotes a fight-or-flight response, corresponds with arousal and energy generation, and inhibits digestion
- Diverts blood flow away from the gastrointestinal (GI) tract and skin via vasoconstriction
- Blood flow to skeletal muscles and the lungs is enhanced (by as much as 1200% in the case of skeletal muscles)
- Dilates bronchioles of the lung through circulating epinephrine, which allows for greater alveolar oxygen exchange
- Increases heart rate and the contractility of cardiac cells (myocytes), thereby providing a mechanism for enhanced blood flow to skeletal muscles
- Dilates pupils and relaxes the ciliary muscle to the lens, allowing more light to enter the eye and enhances far vision
- Provides vasodilation for the coronary vessels of the heart
- Constricts all the intestinal sphincters and the urinary sphincter
- Inhibits peristalsis
- Stimulates orgasm
Parasympathetic nervous system
The parasympathetic nervous system has been said to promote a “rest and digest” response, promote calming of the nerves return to regular function, and enhancing digestion. Functions of nerves within the parasympathetic nervous system include
- Dilating blood vessels leading to the GI tract, increasing the blood flow.
- Constricting the bronchiolar diameter when the need for oxygen has diminished
- Dedicated cardiac branches of the vagus and thoracic spinal accessory nerves impart parasympathetic control of the heart (myocardium)
- Constriction of the pupil and contraction of the ciliary muscles, facilitating accommodation and allowing for closer vision
- Stimulating salivary gland secretion, and accelerates peristalsis, mediating digestion of food and, indirectly, the absorption of nutrients
- Sexual. Nerves of the peripheral nervous system are involved in the erection of genital tissues via the pelvic splanchnic nerves 2–4. They are also responsible for stimulating sexual arousal.
Enteric nervous system
The enteric nervous system is the intrinsic nervous system of the gastrointestinal system. It has been described as “the Second Brain of the Human Body”.[rx] Its functions include:
- Sensing chemical and mechanical changes in the gut
- Regulating secretions in the gut
- Controlling peristalsis and some other movements
Neurotransmitters
At the effector organs, sympathetic ganglionic neurons release noradrenaline (norepinephrine), along with other transmitters such as ATP, to act on adrenergic receptors, with the exception of the sweat glands and the adrenal medulla:
- Acetylcholine is the preganglionic neurotransmitter for both divisions of the ANS, as well as the postganglionic neurotransmitter of parasympathetic neurons. Nerves that release acetylcholine are said to be cholinergic. In the parasympathetic system, ganglionic neurons use acetylcholine as a neurotransmitter to stimulate muscarinic receptors.
- At the adrenal medulla, there is no postsynaptic neuron. Instead, the presynaptic neuron releases acetylcholine to act on nicotinic receptors. Stimulation of the adrenal medulla releases adrenaline (epinephrine) into the bloodstream, which acts on adrenoceptors, thereby indirectly mediating or mimicking sympathetic activity.
References
![]()



About the author