Rectum Cancer are the third most commonly diagnosed cancer in the United States and the second deadliest. Rectal cancer has distinct environmental associations and genetic risk factors different from colon cancer. The transformation of the normal rectal epithelium to a dysplastic lesion and eventually an invasive carcinoma requires a combination of genetic mutations either somatic (acquired) or germline (inherited) over an approximately 10 to 15 year period. Response to pre-operative therapy and pathological staging are the most important prognostic indicators of rectal cancer.
Types of Rectum Cancer
Other, much less common types of tumors can start in the colon and rectum, too. These include:
- Carcinoid tumors – These start from special hormone-making cells in the intestine. They’re covered in Gastrointestinal Carcinoid Tumors.
- Gastrointestinal stromal tumors (GISTs) – start from special cells in the wall of the colon called the interstitial cells of Cajal. Some are not cancer (benign). These tumors can be found anywhere in the digestive tract, but are not common in the colon. They’re discussed in Gastrointestinal Stromal Tumor (GIST).
- Lymphomas – are cancers of immune system cells. They mostly start in lymph nodes, but they can also start in the colon, rectum, or other organs. Information on lymphomas of the digestive system can be found in Non-Hodgkin Lymphoma.
- Sarcomas – can start in blood vessels, muscle layers, or other connective tissues in the wall of the colon and rectum. Sarcomas of the colon or rectum are rare. They’re discussed in Soft Tissue Sarcoma.
There are three ways that cancer spreads in the body.
Cancer can spread through tissue, the lymph system, and the blood:
-
Tissue – Cancer spreads from where it began by growing into nearby areas.
-
Lymph system -Cancer spreads from where it began by getting into the lymph system. Cancer travels through the lymph vessels to other parts of the body.
-
Blood – Cancer spreads from where it began by getting into the blood. Cancer travels through the blood vessels to other parts of the body.
Cancer may spread from where it began to other parts of the body.
When cancer spreads to another part of the body, it is called metastasis. Cancer cells break away from where they began (the primary tumor) and travel through the lymph system or blood.
-
Lymph system – cancer gets into the lymph system, travels through the lymph vessels, and forms a tumor (metastatic tumor) in another part of the body.
-
Blood – Cancer gets into the blood, travels through the blood vessels, and forms a tumor (metastatic tumor) in another part of the body.
The metastatic tumor is the same type of cancer as the primary tumor. For example, if rectal cancer spreads to the lung, the cancer cells in the lung are actually rectal cancer cells. The disease is metastatic rectal cancer, not lung cancer.
Metastasis: how cancer spreads
- Many cancer deaths are caused when cancer moves from the original tumor and spreads to other tissues and organs. This is called metastatic cancer. This animation shows how cancer cells travel from the place in the body where they first formed to other parts of the body.
Causes of Rectum Cancer
Rectal cancer occurs when healthy cells in the rectum develop errors in their DNA. In most cases, the cause of these errors is unknown.
- Healthy cells grow and divide in an orderly way to keep your body functioning normally. But when a cell’s DNA is damaged and becomes cancerous, cells continue to divide — even when new cells aren’t needed. As the cells accumulate, they form a tumor.
- With time, the cancer cells can grow to invade and destroy normal tissue nearby. And cancerous cells can travel to other parts of the body.
Inherited gene mutations that increase the risk of colon and rectal cancer
In some families, gene mutations passed from parents to children increase the risk of colorectal cancer. These mutations are involved in only a small percentage of rectal cancers. Some genes linked to rectal cancer increase an individual’s risk of developing the disease, but they don’t make it inevitable.
Two well-defined genetic colorectal cancer syndromes are
- Hereditary nonpolyposis colorectal cancer (HNPCC) – HNPCC, also called Lynch syndrome, increases the risk of colon cancer and other cancers. People with HNPCC tend to develop colon cancer before age 50.
- Familial adenomatous polyposis (FAP) – FAP is a rare disorder that causes you to develop thousands of polyps in the lining of your colon and rectum. People with untreated FAP have a greatly increased risk of developing colon or rectal cancer before age 40.
FAP, HNPCC and other, rarer inherited colorectal cancer syndromes can be detected through genetic testing. If you’re concerned about your family’s history of colon cancer, talk to your doctor about whether your family history suggests you have a risk of these conditions.
Risk factors
The characteristics and lifestyle factors that increase your risk of rectal cancer are the same as those that increase your risk of colon cancer. They include:
- Older age – The great majority of people diagnosed with colon and rectal cancer are older than 50. Colorectal cancer can occur in younger people, but it occurs much less frequently.
- African-American descent – People of African ancestry born in the United States have a greater risk of colorectal cancer than do people of European ancestry.
- A personal history of colorectal cancer or polyps – If you’ve already had rectal cancer, colon cancer or adenomatous polyps, you have a greater risk of colorectal cancer in the future.
- Inflammatory bowel disease – Chronic inflammatory diseases of the colon and rectum, such as ulcerative colitis and Crohn’s disease, increase your risk of colorectal cancer.
- Inherited syndromes that increase colorectal cancer risk – Genetic syndromes passed through generations of your family can increase your risk of colorectal cancer. These syndromes include FAP and HNPCC.
- Family history of colorectal cancer – You’re more likely to develop colorectal cancer if you have a parent, sibling or child with the disease. If more than one family member has colon cancer or rectal cancer, your risk is even greater.
- Dietary factors – Colorectal cancer may be associated with a diet low in vegetables and high in red meat, particularly when the meat is charred or well-done.
- A sedentary lifestyle – If you’re inactive, you’re more likely to develop colorectal cancer. Getting regular physical activity may reduce your risk of colon cancer.
- Diabetes – People with poorly controlled type 2 diabetes and insulin resistance may have an increased risk of colorectal cancer.
- Obesity – People who are obese have an increased risk of colorectal cancer and an increased risk of dying of colon or rectal cancer when compared with people considered normal weight.
- Smoking – People who smoke may have an increased risk of colon cancer.
- Alcohol – Regularly drinking more than three alcoholic beverages a week may increase your risk of colorectal cancer.
- Radiation therapy for previous cancer – Radiation therapy directed at the abdomen to treat previous cancers may increase the risk of colorectal cancer.
Symptoms of Rectum Cancer
Common symptoms include:
-
Blood (either bright red or very dark) in the stool.
- A change in bowel habits.
- Diarrhea.
- Constipation.
- Feeling that the bowel does not empty completely.
- Stools that are narrower or have a different shape than usual.
-
General abdominal discomfort (frequent gas pains, bloating, fullness, or cramps).
-
Change in appetite.
-
Weight loss for no known reason.
-
Feeling very tired.
- A change in your bowel habits, such as diarrhea, constipation or more frequent bowel movements
- Dark or red blood in the stool
- Mucus in stool
- Narrow stool
- Abdominal pain
- Painful bowel movements
- Iron deficiency anemia
- A feeling that your bowel doesn’t empty completely
- Unexplained weight loss
- Weakness or fatigue
- Blood in the stool
- Diarrhea and/or constipation
- Bloating
- A feeling that you are unable to empty your bowels
If cancer metastasizes or spreads to other parts of the body, symptoms may vary depending on where in the body the cancer is located. Symptoms of metastatic rectal cancer may include:
- Persistent cough
- Fatigue
- Bone pain
- Shortness of breath
- Loss of appetite
- Jaundice
- Swelling in the hands and feet
- Changes in vision or speech
Diagnosis of Rectum Cancer
Anything that increases your chance of getting a disease is called a risk factor. Having a risk factor does not mean that you will get cancer; not having risk factors doesn’t mean that you will not get cancer. Talk to your doctor if you think you may be at risk for colorectal cancer.
-
Having a family history of colon or rectal cancer in a first-degree relative (parent, sibling, or child).
-
Having a personal history of cancer of the colon, rectum, or ovary.
-
Having a personal history of high-risk adenomas (colorectal polyps that are 1 centimeter or larger in size or that have cells that look abnormal under a microscope).
-
Having inherited changes in certain genes that increase the risk of familial adenomatous polyposis (FAP) or Lynch syndrome (hereditary nonpolyposis colorectal cancer).
-
Having a personal history of chronic ulcerative colitis or Crohn disease for 8 years or more.
-
Having three or more alcoholic drinks per day.
-
Smoking cigarettes.
-
Being black.
-
Being obese.
Older age is a main risk factor for most cancers. The chance of getting cancer increases as you get older.

Created for the National Cancer Institute, http://www.cancer.gov
Tests that examine the rectum and colon are used to detect (find) and diagnose rectal cancer.
Tests used to diagnose rectal cancer include the following:
-
Physical exam and history – An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patient’s health habits and past illnesses and treatments will also be taken.
-
Digital rectal exam (DRE) – An exam of the rectum. The doctor or nurse inserts a lubricated, gloved finger into the lower part of the rectum to feel for lumps or anything else that seems unusual. In women, the vagina may also be examined.
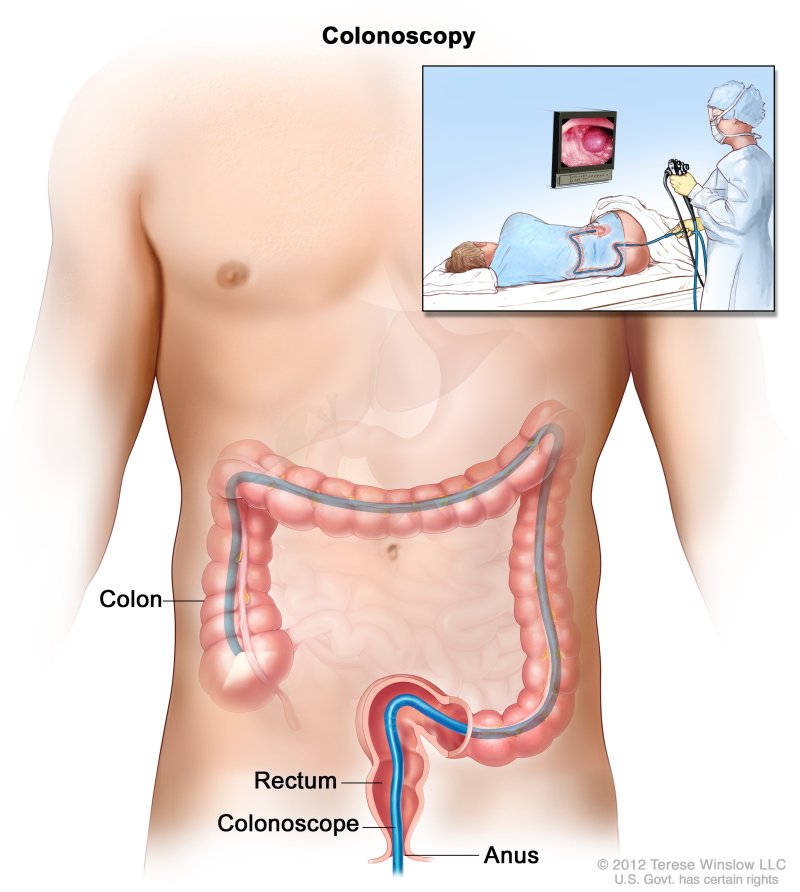
- Colonoscopy – A procedure to look inside the rectum and colon for polyps (small pieces of bulging tissue), abnormal areas, or cancer. A colonoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove polyps or tissue samples, which are checked under a microscope for signs of cancer.
- Biopsy – The removal of cells or tissues so they can be viewed under a microscope to check for signs of cancer. Tumor tissue that is removed during the biopsy may be checked to see if the patient is likely to have the gene mutation that causes HNPCC. This may help to plan treatment. The following tests may be used:
- Reverse transcription-polymerase chain reaction (RT–PCR) test – A laboratory test in which the amount of a genetic substance called mRNA made by a specific gene is measured. An enzyme called reverse transcriptase is used to convert a specific piece of RNA into a matching piece of DNA, which can be amplified (made in large numbers) by another enzyme called DNA polymerase. The amplified DNA copies help tell whether a specific mRNA is being made by a gene. RT–PCR can be used to check the activation of certain genes that may indicate the presence of cancer cells. This test may be used to look for certain changes in a gene or chromosome, which may help diagnose cancer.
- Immunohistochemistry – A laboratory test that uses antibodies to check for certain antigens (markers) in a sample of a patient’s tissue. The antibodies are usually linked to an enzyme or a fluorescent dye. After the antibodies bind to a specific antigen in the tissue sample, the enzyme or dye is activated, and the antigen can then be seen under a microscope. This type of test is used to help diagnose cancer and to help tell one type of cancer from another type of cancer.
- Carcinoembryonic antigen (CEA) assay – A test that measures the level of CEA in the blood. CEA is released into the bloodstream from both cancer cells and normal cells. When found in higher than normal amounts, it can be a sign of rectal cancer or other conditions.
- Anorectal manometry – measures and assesses the anal sphincter (internal and external) and rectal pressure and its function. This method is used to evaluate patients with fecal incontinence and constipation. It can directly measure the luminal pressure, including the high-pressure zone, resting pressure, squeezing pressure, rectal sensation/compliance, and the anorectal inhibitory reflex.[rx]
- Defecating proctography/Defecography – A study using X-ray imaging to evaluate anatomic defects of the anorectal region and function of the puborectalis muscle. A contrast filled paste gets initially introduced to the rectum, and the patient is instructed to defecate in a series of stages (relaxation, contraction, tensing of the abdomen, and evacuation).[rx]
- Balloon capacity and compliance test – Evaluates the function of the rectum using a device (plastic catheter with a latex balloon attached), which is inserted into the rectum and gradually filled with warm water. During this process, the volume and pressure are measured.[rx]
- Balloon evacuation study – This test is similar to the balloon capacity and compliance test in which a catheter with a small balloon gets inserted into the rectum and filled with water. Different volumes of water get loaded inside the balloon, and the patient is instructed to evacuate the balloon. This procedure is done to evaluate the opening of the anal canal and to assess the relaxation of the pelvic floor.[rx]
- Pudendal nerve terminal motor latency – A probe designed to stimulate and record nerve activity is placed on the physician’s gloved finger, which is then inserted into the rectum to measure pudendal nerve activity (latency to contraction of the anal sphincter muscle). The pudendal nerve innervates the anal sphincter muscles; therefore, this test can be used to assess any injury to that nerve.
- Electromyography – A test to measure the ability of the puborectalis muscle and sphincter muscles to relax properly. An electrode is placed inside the rectum, and the activity of these muscles gets evaluated throughout a series of stages (relaxation, contraction, and evacuation).[rx]
- Endoanal Ultrasonography – The use of ultrasound imaging to examine rectal lesions, defects, or injuries to the surrounding tissues.[rx]
- Suction rectal biopsy – Gold standard for the diagnosis of Hirschsprung disease. A biopsy is taken two cm above the dentate line, and the absence of ganglion cells on histology confirms the diagnosis. Hypertrophic nerve fibers may be present in addition to this finding.[rx]
- Contrast enema – Used as one of the diagnostic methods for Hirschsprung disease. Useful for localization of the aganglionic segment by looking for a narrowed rectum. Diagnostic confirmation is via a rectal biopsy.[rx]
Certain factors affect prognosis (chance of recovery) and treatment options.
The prognosis (chance of recovery) and treatment options depend on the following:
-
The stage of the cancer (whether it affects the inner lining of the rectum only, involves the whole rectum, or has spread to lymph nodes, nearby organs, or other places in the body).
-
Whether the tumor has spread into or through the bowel wall.
-
Where the cancer is found in the rectum.
-
Whether the bowel is blocked or has a hole in it.
-
Whether all of the tumor can be removed by surgery.
-
The patient’s general health.
-
Whether the cancer has just been diagnosed or has recurred (come back).
Stages of Rectum Cancer
After rectal cancer has been diagnosed, tests are done to find out if cancer cells have spread within the rectum or to other parts of the body.
The process used to find out whether cancer has spread within the rectum or to other parts of the body is called staging. The information gathered from the staging process determines the stage of the disease. It is important to know the stage in order to plan treatment.
The following tests and procedures may be used in the staging process:
- Chest x-ray – An x-ray of the organs and bones inside the chest. An x-ray is a type of energy beam that can go through the body and onto film, making a picture of areas inside the body.
- Colonoscopy – A procedure to look inside the rectum and colon for polyps (small pieces of bulging tissue). abnormal areas, or cancer. A colonoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove polyps or tissue samples, which are checked under a microscope for signs of cancer.

-
CT scan (CAT scan) – A procedure that makes a series of detailed pictures of areas inside the body, such as the abdomen, pelvis, or chest, taken from different angles. The pictures are made by a computer linked to an x-ray machine. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
-
MRI (magnetic resonance imaging) – A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging (NMRI).
-
PET scan (positron emission tomography scan) – A procedure to find malignant tumor cells in the body. A small amount of radioactive glucose (sugar) is injected into a vein. The PET scanner rotates around the body and makes a picture of where glucose is being used in the body. Malignant tumor cells show up brighter in the picture because they are more active and take up more glucose than normal cells do.
-
Endorectal ultrasound – A procedure used to examine the rectum and nearby organs. An ultrasound transducer (probe) is inserted into the rectum and used to bounce high-energy sound waves (ultrasound) off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram. The doctor can identify tumors by looking at the sonogram. This procedure is also called transrectal ultrasound.
The following stages are used for rectal cancer:
Stage 0 (Carcinoma in Situ)
Stage 0 (rectal carcinoma in situ). Abnormal cells are shown in the mucosa of the rectum wall.
In stage 0 rectal cancer, abnormal cells are found in the mucosa (innermost layer) of the rectum wall. These abnormal cells may become cancer and spread into nearby normal tissue. Stage 0 is also called carcinoma in situ.
Stage I
Stage I rectal cancer. Cancer has spread from the mucosa of the rectum wall to the submucosa or to the muscle layer.
In stage, I rectal cancer, cancer has formed in the mucosa (innermost layer) of the rectum wall and has spread to the submucosa (layer of tissue next to the mucosa) or to the muscle layer of the rectum wall.
Stage II
Stage II rectal cancer. In stage IIA, cancer has spread through the muscle layer of the rectum wall to the serosa. In stage IIB, cancer has spread through the serosa but has not spread to nearby organs. In stage IIC, cancer has spread through the serosa to nearby organs.
Stage II rectal cancer is divided into stages IIA, IIB, and IIC.
-
Stage IIA: Cancer has spread through the muscle layer of the rectum wall to the serosa (outermost layer) of the rectum wall.
-
Stage IIB: Cancer has spread through the serosa (outermost layer) of the rectum wall to the tissue that lines the organs in the abdomen (visceral peritoneum).
-
Stage IIC: Cancer has spread through the serosa (outermost layer) of the rectum wall to nearby organs.
Stage III
Stage III rectal cancer is divided into stages IIIA, IIIB, and IIIC.
Stage IIIA rectal cancer. Cancer has spread through the mucosa of the rectum wall to the submucosa and may have spread to the muscle layer, and has spread to one to three nearby lymph nodes or tissues near the lymph nodes. OR, cancer has spread through the mucosa to the submucosa and four to six nearby lymph nodes.
In stage IIIA, cancer has spread:
-
through the mucosa (innermost layer) of the rectum wall to the submucosa (layer of tissue next to the mucosa) or to the muscle layer of the rectum wall. Cancer has spread to one to three nearby lymph nodes or cancer cells have formed in tissue near the lymph nodes; or
-
through the mucosa (innermost layer) of the rectum wall to the submucosa (layer of tissue next to the mucosa). Cancer has spread to four to six nearby lymph nodes.
In stage IIIB, cancer has spread:
-
through the muscle layer of the rectum wall to the serosa (outermost layer) of the rectum wall or has spread through the serosa to the tissue that lines the organs in the abdomen (visceral peritoneum). Cancer has spread to one to three nearby lymph nodes or cancer cells have formed in tissue near the lymph nodes; or
-
to the muscle layer or to the serosa (outermost layer) of the rectum wall. Cancer has spread to four to six nearby lymph nodes; or
-
through the mucosa (innermost layer) of the rectum wall to the submucosa (layer of tissue next to the mucosa) or to the muscle layer of the rectum wall. Cancer has spread to seven or more nearby lymph nodes.
In stage IIIC, cancer has spread:
-
through the serosa (outermost layer) of the rectum wall to the tissue that lines the organs in the abdomen (visceral peritoneum). Cancer has spread to four to six nearby lymph nodes; or
-
through the muscle layer of the rectum wall to the serosa (outermost layer) of the rectum wall or has spread through the serosa to the tissue that lines the organs in the abdomen (visceral peritoneum). Cancer has spread to seven or more nearby lymph nodes; or
-
through the serosa (outermost layer) of the rectum wall to nearby organs. Cancer has spread to one or more nearby lymph nodes or cancer cells have formed in tissue near the lymph nodes.
Stage IV
Stage IV rectal cancer is divided into stages IVA, IVB, and IVC.
-
Stage IVA – Cancer has spread to one area or organ that is not near the rectum, such as the liver, lung, ovary, or a distant lymph node.
-
Stage IVB – cancer has spread to more than one area or organ that is not near the rectum, such as the liver, lung, ovary, or a distant lymph node.
-
Stage IVC – Cancer has spread to the tissue that lines the wall of the abdomen and may have spread to other areas or organs.
Treatment of Rectum Cancer
Six types of standard treatment are used
Surgery
Surgery is the most common treatment for all stages of rectal cancer. The cancer is removed using one of the following types of surgery:
-
Polypectomy – If the cancer is found in a polyp (a small piece of bulging tissue), the polyp is often removed during a colonoscopy.
-
Local excision – If the cancer is found on the inside surface of the rectum and has not spread into the wall of the rectum, cancer and a small amount of surrounding healthy tissue is removed.
-
Resection – If cancer has spread into the wall of the rectum, the section of the rectum with cancer and nearby healthy tissue is removed. Sometimes the tissue between the rectum and the abdominal wall is also removed. The lymph nodes near the rectum are removed and checked under a microscope for signs of cancer.
-
Radiofrequency ablation – The use of a special probe with tiny electrodes that kill cancer cells. Sometimes the probe is inserted directly through the skin and only local anesthesia is needed. In other cases, the probe is inserted through an incision in the abdomen. This is done in the hospital with general anesthesia.
-
Cryosurgery – A treatment that uses an instrument to freeze and destroy abnormal tissue. This type of treatment is also called cryotherapy.
-
Pelvic exenteration – If cancer has spread to other organs near the rectum, the lower colon, rectum, and bladder are removed. In women, the cervix, vagina, ovaries, and nearby lymph nodes may be removed. In men, the prostate may be removed. Artificial openings (stoma) are made for urine and stool to flow from the body to a collection bag.
After the cancer is removed, the surgeon will either
- do an anastomosis (sew the healthy parts of the rectum together, sew the remaining rectum to the colon, or sew the colon to the anus);
Resection of the rectum with anastomosis. The rectum and part of the colon are removed, and then the colon and anus are joined.
or
-
make a stoma (an opening) from the rectum to the outside of the body for waste to pass through. This procedure is done if the cancer is too close to the anus and is called a colostomy. A bag is placed around the stoma to collect the waste. Sometimes the colostomy is needed only until the rectum has healed, and then it can be reversed. If the entire rectum is removed, however, the colostomy may be permanent.
-
Radiation therapy and/or chemotherapy may be given before surgery to shrink the tumor, make it easier to remove cancer, and help with bowel control after surgery. Treatment is given before surgery is called neoadjuvant therapy. After all, cancer that can be seen at the time of the surgery is removed, some patients may be given radiation therapy and/or chemotherapy after surgery to kill any cancer cells that are left. Treatment given after the surgery, to lower the risk that cancer will come back, is called adjuvant therapy.
Radiation therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. There are two types of radiation therapy:
-
External radiation therapy uses a machine outside the body to send radiation toward the cancer.
-
Internal radiation therapy uses a radioactive substance sealed in needles, seeds, wires, or catheters that are placed directly into or near the cancer.
The way radiation therapy is given depends on the type and stage of the cancer being treated. External radiation therapy is used to treat rectal cancer.
Short-course preoperative radiation therapy is used in some types of rectal cancer. This treatment uses fewer and lower doses of radiation than the standard treatment, followed by surgery several days after the last dose.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping the cells from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). When chemotherapy is placed directly in the cerebrospinal fluid, an organ, or a body cavity such as the abdomen, the drugs mainly affect cancer cells in those areas (regional chemotherapy).
Chemoembolization of the hepatic artery is a type of regional chemotherapy that may be used to treat cancer that has spread to the liver. This is done by blocking the hepatic artery (the main artery that supplies blood to the liver) and injecting anticancer drugs between the blockage and the liver. The liver’s arteries then carry the drugs into the liver. Only a small amount of the drug reaches other parts of the body. The blockage may be temporary or permanent, depending on what is used to block the artery. The liver continues to receive some blood from the hepatic portal vein, which carries blood from the stomach and intestine.
The way the chemotherapy is given depends on the type and stage of the cancer being treated.
Active surveillance
Active surveillance is closely following a patient’s condition without giving any treatment unless there are changes in test results. It is used to find early signs that the condition is getting worse. Inactive surveillance, patients are given certain exams and tests to check if the cancer is growing. When cancer begins to grow, treatment is given to cure cancer. Tests include the following:
-
Digital rectal exam.
-
MRI.
-
Endoscopy.
-
Sigmoidoscopy.
-
CT scan.
-
Carcinoembryonic antigen (CEA) assay.
Targeted therapy
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells without harming normal cells.
Types of targeted therapies used in the treatment of rectal cancer include the following
-
Monoclonal antibodies – Monoclonal antibody therapy is a type of targeted therapy being used for the treatment of rectal cancer. Monoclonal antibody therapy uses antibodies made in the laboratory from a single type of immune system cell. These antibodies can identify substances on cancer cells or normal substances that may help cancer cells grow. The antibodies attach to the substances and kill the cancer cells, block their growth, or keep them from spreading. Monoclonal antibodies are given by infusion. They may be used alone or to carry drugs, toxins, or radioactive material directly to cancer cells.
There are different types of monoclonal antibody therapy
- Vascular endothelial growth factor (VEGF) inhibitor therapy – Cancer cells make a substance called VEGF, which causes new blood vessels to form (angiogenesis) and helps the cancer grow. VEGF inhibitors block VEGF and stop new blood vessels from forming. This may kill cancer cells because they need new blood vessels to grow. Bevacizumab and ramucirumab are VEGF inhibitors and angiogenesis inhibitors.
-
Epidermal growth factor receptor (EGFR) inhibitor therapy – EGFRs are proteins found on the surface of certain cells, including cancer cells. Epidermal growth factor attaches to the EGFR on the surface of the cell and causes the cells to grow and divide. EGFR inhibitors block the receptor and stop the epidermal growth factor from attaching to the cancer cell. This stops the cancer cell from growing and dividing. Cetuximab and panitumumab are EGFR inhibitors.
-
Angiogenesis inhibitors – Angiogenesis inhibitors stop the growth of new blood vessels that tumors need to grow
-
Ziv-aflibercept – is a vascular endothelial growth factor trap that blocks an enzyme needed for the growth of new blood vessels in tumors.
-
Regorafenib – is used to treat colorectal cancer that has spread to other parts of the body and has not gotten better with other treatment. It blocks the action of certain proteins, including vascular endothelial growth factor. This may help keep cancer cells from growing and may kill them. It may also prevent the growth of new blood vessels that tumors need to grow.
Immunotherapy
Immunotherapy is a treatment that uses the patient’s immune system to fight cancer. Substances made by the body or made in a laboratory are used to boost, direct, or restore the body’s natural defenses against cancer. This type of cancer treatment is also called biotherapy or biologic therapy.
Immune checkpoint inhibitor therapy is a type of immunotherapy:
-
Immune checkpoint inhibitor therapy: PD-1 is a protein on the surface of T cells that helps keep the body’s immune responses in check. When PD-1 attaches to another protein called PDL-1 on a cancer cell, it stops the T cell from killing the cancer cell. PD-1 inhibitors attach to PDL-1 and allow the T cells to kill cancer cells. Pembrolizumab is a type of immune checkpoint inhibitor.
Treatment Options by Stage
For information about the treatments listed below, see the Treatment Option Overview section.
Stage 0 (Carcinoma in Situ)
Treatment of stage 0 may include the following:
-
Simple polypectomy.
-
Local excision.
-
Resection (when the tumor is too large to remove by local excision).
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Stage I Rectal Cancer
Treatment of stage I rectal cancer may include the following:
-
Local excision.
-
Resection.
-
Resection with radiation therapy and chemotherapy after surgery.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Stages II and III Rectal Cancer
Treatment of stage II and stage III rectal cancer may include the following:
-
Surgery.
-
Chemotherapy combined with radiation therapy, followed by surgery.
-
Short-course radiation therapy followed by surgery and chemotherapy.
-
Resection followed by chemotherapy combined with radiation therapy.
-
Chemotherapy combined with radiation therapy, followed by active surveillance. Surgery may be done if the cancer recurs (comes back).
-
A clinical trial of a new treatment.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Stage IV and Recurrent Rectal Cancer
Treatment of stage IV and recurrent rectal cancer may include the following:
-
Surgery with or without chemotherapy or radiation therapy.
-
Systemic chemotherapy with or without targeted therapy (angiogenesis inhibitor).
-
Systemic chemotherapy with or without immunotherapy (immune checkpoint inhibitor therapy).
-
Chemotherapy to control the growth of the tumor.
-
Radiation therapy, chemotherapy, or a combination of both, as palliative therapy to relieve symptoms and improve the quality of life.
-
Placement of a stent to help keep the rectum open if it is partly blocked by the tumor, as palliative therapy to relieve symptoms and improve the quality of life.
-
Immunotherapy.
-
Clinical trials of chemotherapy and/or targeted therapy.
Treatment of rectal cancer that has spread to other organs depends on where the cancer has spread.
- Treatment for areas of cancer that have spread to the liver includes the following:
- Surgery to remove the tumor. Chemotherapy may be given before surgery, to shrink the tumor.
- Cryosurgery or radiofrequency ablation.
- Chemoembolization and/or systemic chemotherapy.
- A clinical trial of chemoembolization combined with radiation therapy to the tumors in the liver.
Drugs Approved for Colon and Rectum Cancer
- Avastin (Bevacizumab)
- Bevacizumab
- Camptosar (Irinotecan Hydrochloride)
- Capecitabine
- Cetuximab
- Cyramza (Ramucirumab)
- Eloxatin (Oxaliplatin)
- Erbitux (Cetuximab)
- 5-FU (Fluorouracil Injection)
- Fluorouracil Injection
- Ipilimumab
- Irinotecan Hydrochloride
- Keytruda (Pembrolizumab)
- Leucovorin Calcium
- Lonsurf (Trifluridine and Tipiracil Hydrochloride)
- Mvasi (Bevacizumab)
- Nivolumab
- Opdivo (Nivolumab)
- Oxaliplatin
- Panitumumab
- Pembrolizumab
- Ramucirumab
- Regorafenib
- Stivarga (Regorafenib)
- Trifluridine and Tipiracil Hydrochloride
- Vectibix (Panitumumab)
- Xeloda (Capecitabine)
- Yervoy (Ipilimumab)
- Zaltrap (Ziv-Aflibercept)
- Ziv-Aflibercept
Drug Combinations Used in Colon Cancer
- CAPOX
- FOLFIRI
- FOLFIRI-BEVACIZUMAB
- FOLFIRI-CETUXIMAB
- FOLFOX
- FU-LV
- XELIRI
- XELOX
Drugs Approved for Rectal Cancer
- Avastin (Bevacizumab)
- Bevacizumab
- Camptosar (Irinotecan Hydrochloride)
- Capecitabine
- Cetuximab
- Cyramza (Ramucirumab)
- Eloxatin (Oxaliplatin)
- Erbitux (Cetuximab)
- 5-FU (Fluorouracil Injection)
- Fluorouracil Injection
- Ipilimumab
- Irinotecan Hydrochloride
- Keytruda (Pembrolizumab)
- Leucovorin Calcium
- Lonsurf (Trifluridine and Tipiracil Hydrochloride)
- Mvasi (Bevacizumab)
- Nivolumab
- Opdivo (Nivolumab)
- Oxaliplatin
- Panitumumab
- Pembrolizumab
- Ramucirumab
- Regorafenib
- Stivarga (Regorafenib)
- Trifluridine and Tipiracil Hydrochloride
- Vectibix (Panitumumab)
- Xeloda (Capecitabine)
- Yervoy (Ipilimumab)
- Zaltrap (Ziv-Aflibercept)
- Ziv-Aflibercept
Drug Combinations Used in Rectal Cancer
- CAPOX
- FOLFIRI
- FOLFIRI-BEVACIZUMAB
- FOLFIRI-CETUXIMAB
- FOLFOX
- FU-LV
- XELIRI
- XELOX
Drugs Approved for Gastroenteropancreatic Neuroendocrine Tumors
- Afinitor (Everolimus)
- Everolimus
- Lanreotide Acetate
- Somatuline Depot (Lanreotide Acetate)
To Learn More About Rectal Cancer
For more information from the National Cancer Institute about rectal cancer, see the following:
-
Colorectal Cancer Home Page
-
Colorectal Cancer Prevention
-
Colorectal Cancer Screening
-
Tests to Detect Colorectal Cancer and Polyps
-
Childhood Colorectal Cancer Treatment
-
Cryosurgery in Cancer Treatment
-
Drugs Approved for Colon and Rectal Cancer
-
Targeted Cancer Therapies
-
Genetic Testing for Inherited Cancer Susceptibility Syndromes
For general cancer information and other resources from the National Cancer Institute, see the following:
-
About Cancer
-
Staging
-
Chemotherapy and You: Support for People With Cancer
-
Radiation Therapy and You: Support for People With Cancer
-
Coping with Cancer
-
Questions to Ask Your Doctor about Cancer
-
For Survivors and Caregivers
References
![]()














About the author