Lung Carcinoma/ Lung cancer is among the most deadly cancers for both men and women (rx). Its death rate exceeds that of the three most common cancers (colon, breast, and pancreatic) combined (rx). Over half of patients diagnosed with lung cancer die within one year of diagnosis and the 5-year survival is around 17.8% (rx). There are two main subtypes of lung cancer, small-cell lung carcinoma and non-small-cell lung carcinoma (NSCLC), accounting for 15% and 85% of all lung cancer, respectively (rx). NSCLC is further classified into three types: squamous-cell carcinoma, adenocarcinoma, and large-cell carcinoma.
General Information About Non-Small Cell Lung Cancer (NSCLC)
NSCLC is any type of epithelial lung cancer other than small cell lung cancer (SCLC). The most common types of NSCLC are squamous cell carcinoma, large cell carcinoma, and adenocarcinoma, but there are several other types that occur less frequently, and all types can occur in unusual histologic variants. Although NSCLCs are associated with cigarette smoke, adenocarcinomas may be found in patients who have never smoked. As a class, NSCLCs are relatively insensitive to chemotherapy and radiation therapy compared with SCLC. Patients with resectable disease may be cured by surgery or surgery followed by chemotherapy. Local control can be achieved with radiation therapy in a large number of patients with unresectable disease, but cure is seen only in a small number of patients. Patients with locally advanced unresectable disease may achieve long-term survival with radiation therapy combined with chemotherapy. Patients with advanced metastatic disease may achieve improved survival and palliation of symptoms with chemotherapy, targeted agents, and other supportive measures.
Incidence and Mortality
Estimated new cases and deaths from lung cancer (NSCLC and SCLC combined) in the United States in 2018:[1]
-
New cases: 234,030.
-
Deaths: 154,050.
Lung cancer is the leading cause of cancer-related mortality in the United States.[1] The 5-year relative survival rate from 1995 to 2001 for patients with lung cancer was 15.7%. The 5-year relative survival rate for patients with local-stage (49%), regional-stage (16%), and distant-stage (2%) disease varies markedly, depending on the stage at diagnosis.[2]
Anatomy
NSCLC arises from the epithelial cells of the lung of the central bronchi to terminal alveoli. The histological type of NSCLC correlates with site of origin, reflecting the variation in respiratory tract epithelium of the bronchi to alveoli. Squamous cell carcinoma usually starts near a central bronchus. Adenocarcinoma and bronchioloalveolar carcinoma usually originate in peripheral lung tissue.
Pathogenesis
Smoking-related lung carcinogenesis is a multistep process. Squamous cell carcinoma and adenocarcinoma have defined premalignant precursor lesions. Before becoming invasive, lung epithelium may undergo morphological changes that include the following:
-
Hyperplasia.
-
Metaplasia.
-
Dysplasia.
-
Carcinoma in situ.
Dysplasia and carcinoma in situ are considered the principal premalignant lesions because they are more likely to progress to invasive cancer and less likely to spontaneously regress.
In addition, after resection of a lung cancer, there is a 1% to 2% risk per patient per year that a second lung cancer will occur.[3]
Pathology
NSCLC is a heterogeneous aggregate of histologies. The most common histologies include the following:
-
Epidermoid or squamous cell carcinoma.
-
Adenocarcinoma.
-
Large cell carcinoma.
These histologies are often classified together because approaches to diagnosis, staging, prognosis, and treatment are similar.
Risk Factors
Increasing age is the most important risk factor for most cancers. Other risk factors for lung cancer include the following:
-
History of or current tobacco use: cigarettes, pipes, and cigars.[4]
-
Occupational exposure to asbestos, arsenic, chromium, beryllium, nickel, and other agents.[7]
- Radiation exposure from any of the following:
- Radiation therapy to the breast or chest.[8
- Radon exposure in the home or workplace.[9]
- Medical imaging tests, such as computed tomography (CT) scans.[10]
- Atomic bomb radiation.[11]
-
Family history of lung cancer.[15]
- Human immunodeficiency virus infection.[16]
- Beta carotene supplements in heavy smokers.[17,18]
The single most important risk factor for the development of lung cancer is smoking. For smokers, the risk for lung cancer is on average tenfold higher than in lifetime nonsmokers (defined as a person who has smoked <100 cigarettes in his or her lifetime). The risk increases with the quantity of cigarettes, duration of smoking, and starting age.
Smoking cessation results in a decrease in precancerous lesions and a reduction in the risk of developing lung cancer. Former smokers continue to have an elevated risk of lung cancer for years after quitting. Asbestos exposure may exert a synergistic effect of cigarette smoking on the lung cancer risk.[19]
Prevention
A significant number of patients cured of their smoking-related lung cancer may develop a second malignancy. In the Lung Cancer Study Group trial of 907 patients with stage T1, N0 resected tumors, the rate was 1.8% per year for nonpulmonary second cancers and 1.6% per year for new lung cancers.[20] Other studies have reported even higher risks of second tumors in long-term survivors, including rates of 10% for second lung cancers and 20% for all second cancers.[21]
Because of the persistent risk of developing second lung cancers in former smokers, various chemoprevention strategies have been evaluated in randomized control trials. None of the phase III trials using the agents beta carotene, retinol, 13-cis-retinoic acid, [alpha]-tocopherol, N-acetylcysteine, or acetylsalicylic acid has demonstrated beneficial, reproducible results.[18,22–25][Level of evidence: 1iiA] Chemoprevention of second primary cancers of the upper aerodigestive tract is undergoing clinical evaluation in patients with early-stage lung cancer.
(Refer to the PDQ summary on Lung Cancer Prevention for more information.)
Screening
In patients considered at high risk for developing lung cancer, the only screening modality for early detection that has been shown to alter mortality is low-dose helical CT scanning.[26] Studies of lung cancer screening with chest radiography and sputum cytology have failed to demonstrate that screening lowers lung cancer mortality rates.
(Refer to the Screening by low-dose helical computed tomography subsection in the PDQ summary on Lung Cancer Screening for more information.)
Clinical Features
Lung cancer may present with symptoms or be found incidentally on chest imaging. Symptoms and signs may result from the location of the primary local invasion or compression of adjacent thoracic structures, distant metastases, or paraneoplastic phenomena. The most common symptoms at presentation are worsening cough or chest pain. Other presenting symptoms include the following:
-
Hemoptysis.
-
Malaise.
-
Weight loss.
-
Dyspnea.
-
Hoarseness.
Symptoms may result from local invasion or compression of adjacent thoracic structures such as compression involving the esophagus causing dysphagia, compression involving the laryngeal nerves causing hoarseness, or compression involving the superior vena cava causing facial edema and distension of the superficial veins of the head and neck. Symptoms from distant metastases may also be present and include neurological defect or personality change from brain metastases or pain from bone metastases. Infrequently, patients may present with symptoms and signs of paraneoplastic diseases such as hypertrophic osteoarthropathy with digital clubbing or hypercalcemia from parathyroid hormone-related protein. Physical examination may identify enlarged supraclavicular lymphadenopathy, pleural effusion or lobar collapse, unresolved pneumonia, or signs of associated disease such as chronic obstructive pulmonary disease or pulmonary fibrosis.
Diagnosis
Investigations of patients with suspected NSCLC focus on confirming the diagnosis and determining the extent of the disease. Treatment options for patients are determined by histology, stage, and general health and comorbidities of the patient.
The procedures used to determine the presence of cancer include the following:
-
History.
-
Physical examination.
-
Routine laboratory evaluations.
-
Chest x-ray.
-
Chest CT scan with infusion of contrast material.
-
Biopsy.
Before a patient begins lung cancer treatment, an experienced lung cancer pathologist must review the pathologic material. This is critical because SCLC, which responds well to chemotherapy and is generally not treated surgically, can be confused on microscopic examination with NSCLC.[27] Immunohistochemistry and electron microscopy are invaluable techniques for diagnosis and subclassification, but most lung tumors can be classified by light microscopic criteria.
(Refer to the Staging Evaluation section of this summary for more information on tests and procedures used for staging.)
Molecular Features
The identification of mutations in lung cancer has led to the development of molecularly targeted therapy to improve the survival of subsets of patients with metastatic disease.[28] In particular, subsets of adenocarcinoma now can be defined by specific mutations in genes encoding components of the epidermal growth factor receptor (EGFR) and downstream mitogen-activated protein kinases (MAPK) and phosphatidylinositol 3-kinases (PI3K) signaling pathways. These mutations may define mechanisms of drug sensitivity and primary or acquired resistance to kinase inhibitors.
Other genetic abnormalities of potential relevance to treatment decisions include translocations involving the anaplastic lymphoma kinase (ALK)-tyrosine kinase receptor, which are sensitive to ALK inhibitors, and amplification of MET (mesenchymal epithelial transition factor), which encodes the hepatocyte growth factor receptor. METamplification has been associated with secondary resistance to EGFR tyrosine kinase inhibitors.
Prognostic Factors
Multiple studies have attempted to identify the prognostic importance of a variety of clinicopathologic factors.[21,29–32] Factors that have correlated with adverse prognosis include the following:
-
Presence of pulmonary symptoms.
-
Large tumor size (>3 cm).
-
Nonsquamous histology.
-
Metastases to multiple lymph nodes within a TNM-defined nodal station.[33–43] (Refer to the Evaluation of Mediastinal Lymph Node Metastasis section of this summary for more information.)
For patients with inoperable disease, prognosis is adversely affected by poor performance status and weight loss of more than 10%. These patients have been excluded from clinical trials evaluating aggressive multimodality interventions.
In multiple retrospective analyses of clinical trial data, advanced age alone has not been shown to influence response or survival with therapy.[47]
(Refer to the separate treatment sections for each stage of NSCLC in this summary for more information about prognosis.)
Because treatment is not satisfactory for almost all patients with NSCLC, eligible patients should be considered for clinical trials. Information about ongoing clinical trials is available from the NCI website.
Related Summaries
Other PDQ summaries containing information related to lung cancer include the following:
Cellular Classification of NSCLC
Malignant non-small cell epithelial tumors of the lung are classified by the World Health Organization (WHO)/International Association for the Study of Lung Cancer (IASLC). There are three main subtypes of non-small cell lung cancer (NSCLC), including the following:
-
Squamous cell carcinoma (25% of lung cancers).
-
Adenocarcinoma (40% of lung cancers).
-
Large cell carcinoma (10% of lung cancers).
There are numerous additional subtypes of decreasing frequency.[1]
WHO/IASLC Histologic Classification of NSCLC
-
Squamous cell carcinoma.
-
Papillary.
-
Clear cell.
-
Small cell.
-
Basaloid.
-
-
Adenocarcinoma.
-
Acinar.
-
Papillary.
-
Bronchioloalveolar carcinoma.
-
Nonmucinous.
-
Mucinous.
-
Mixed mucinous and nonmucinous or indeterminate cell type.
-
-
Solid adenocarcinoma with mucin.
-
Adenocarcinoma with mixed subtypes.
-
Variants.
-
Well-differentiated fetal adenocarcinoma.
-
Mucinous (colloid) adenocarcinoma.
-
Mucinous cystadenocarcinoma.
-
Signet ring adenocarcinoma.
-
Clear cell adenocarcinoma.
-
-
-
Large cell carcinoma.
-
Variants.
-
Large cell neuroendocrine carcinoma (LCNEC).
-
Combined LCNEC.
-
Basaloid carcinoma.
-
Lymphoepithelioma-like carcinoma.
-
Clear cell carcinoma.
-
Large cell carcinoma with rhabdoid phenotype.
-
-
-
Adenosquamous carcinoma.
-
Carcinomas with pleomorphic, sarcomatoid, or sarcomatous elements.
-
Carcinomas with spindle and/or giant cells.
-
Spindle cell carcinoma.
-
Giant cell carcinoma.
-
Carcinosarcoma.
-
Pulmonary blastoma.
-
-
Carcinoid tumor.
-
Typical carcinoid.
-
Atypical carcinoid.
-
-
Carcinomas of salivary gland type.
-
Mucoepidermoid carcinoma.
-
Adenoid cystic carcinoma.
-
Others.
-
-
Unclassified carcinoma.
Squamous cell carcinoma
Most squamous cell carcinomas of the lung are located centrally, in the larger bronchi of the lung. Squamous cell carcinomas are linked more strongly with smoking than other forms of NSCLC. The incidence of squamous cell carcinoma of the lung has been decreasing in recent years.
Adenocarcinoma
Adenocarcinoma is now the most common histologic subtype in many countries, and subclassification of adenocarcinoma is important. One of the biggest problems with lung adenocarcinomas is the frequent histologic heterogeneity. In fact, mixtures of adenocarcinoma histologic subtypes are more common than tumors consisting purely of a single pattern of acinar, papillary, bronchioloalveolar, and solid adenocarcinoma with mucin formation.
Criteria for the diagnosis of bronchioloalveolar carcinoma have varied widely in the past. The current WHO/IASLC definition is much more restrictive than that previously used by many pathologists because it is limited to only noninvasive tumors.
If stromal, vascular, or pleural invasion are identified in an adenocarcinoma that has an extensive bronchioloalveolar carcinoma component, the classification would be an adenocarcinoma of mixed subtype with predominant bronchioloalveolar pattern and a focal acinar, solid, or papillary pattern, depending on which pattern is seen in the invasive component. However, the future of bronchioloalveolar carcinoma as a distinct clinical entity is unclear; a multidisciplinary expert panel representing the IASLC, the American Thoracic Society, and the European Respiratory Society proposed a major revision of the classification of adenocarcinomas in 2011 that entails a reclassification of what was called bronchioloalveolar carcinoma into newly defined histologic subgroups.
The following variants of adenocarcinoma are recognized in the WHO/IASLC classification:
-
Well-differentiated fetal adenocarcinoma.
-
Mucinous (colloid) adenocarcinoma.
-
Mucinous cystadenocarcinoma.
-
Signet ring adenocarcinoma.
-
Clear cell adenocarcinoma.
Large cell carcinoma
In addition to the general category of large cell carcinoma, several uncommon variants are recognized in the WHO/IASLC classification, including the following:
-
LCNEC.
-
Basaloid carcinoma.
-
Lymphoepithelioma-like carcinoma.
-
Clear cell carcinoma.
-
Large cell carcinoma with rhabdoid phenotype.
Basaloid carcinoma is also recognized as a variant of squamous cell carcinoma, and rarely, adenocarcinomas may have a basaloid pattern; however, in tumors without either of these features, they are regarded as a variant of large cell carcinoma.
Neuroendocrine tumors
LCNEC is recognized as a histologically high-grade non-small cell carcinoma. It has a very poor prognosis similar to that of small cell lung cancer (SCLC). Atypical carcinoid is recognized as an intermediate-grade neuroendocrine tumor with a prognosis that falls between typical carcinoid and high-grade SCLC and LCNEC.
Neuroendocrine differentiation can be demonstrated by immunohistochemistry or electron microscopy in 10% to 20% of common NSCLCs that do not have any neuroendocrine morphology. These tumors are not formally recognized within the WHO/IASLC classification scheme because the clinical and therapeutic significance of neuroendocrine differentiation in NSCLC is not firmly established. These tumors are referred to collectively as NSCLC with neuroendocrine differentiation.
Carcinomas with pleomorphic, sarcomatoid, or sarcomatous elements
This is a group of rare tumors. Spindle cell carcinomas and giant cell carcinomas comprise only 0.4% of all lung malignancies, and carcinosarcomas comprise only 0.1% of all lung malignancies. In addition, this group of tumors reflects a continuum in histologic heterogeneity as well as epithelial and mesenchymal differentiation. On the basis of clinical and molecular data, biphasic pulmonary blastoma is regarded as part of the spectrum of carcinomas with pleomorphic, sarcomatoid, or sarcomatous elements.
Molecular features
The identification of mutations in lung cancer has led to the development of molecularly targeted therapy to improve the survival of subsets of patients with metastatic disease.[2] In particular, subsets of adenocarcinoma now can be defined by specific mutations in genes encoding components of the epidermal growth factor receptor (EGFR) and downstream mitogen-activated protein kinases (MAPK) and phosphatidylinositol 3-kinases (PI3K) signaling pathways. These mutations may define mechanisms of drug sensitivity and primary or acquired resistance to kinase inhibitors. Other mutations of potential relevance to treatment decisions include:
-
Kirsten rat sarcoma viral oncogene (KRAS).
-
Anaplastic lymphoma kinase receptor (ALK).
-
Human epidermal growth factor receptor 2 (HER2).
-
V-raf murine sarcoma viral oncogene homolog B1 (BRAF).
-
PI3K catalytic protein alpha (PI3KCA).
-
AKT1.
-
MAPK kinase 1 (MAP2K1 or MEK1).
-
MET, which encodes the hepatocyte growth factor receptor (HGFR).
These mutations are mutually exclusive, except for those involving PI3KCA and BRAF mutations, EGFR mutations, or ALK translocations.[3,4]
EGFR and ALK mutations predominate in adenocarcinomas that develop in nonsmokers, and KRAS and BRAFmutations are more common in smokers or former smokers. EGFR mutations strongly predict the improved response rate and progression-free survival of EGFR inhibitors. In a set of 2,142 lung adenocarcinoma specimens from patients treated at Memorial Sloan Kettering Cancer Center, EGFR exon 19 deletions and L858R were found in 15% of tumors from former smokers (181 of 1,218; 95% confidence interval [CI], 13–17), 6% from current smokers (20 of 344; 95% CI, 4–9), and 52% from never-smokers (302 of 580; 95% CI, 48–56; P < .001 for ever- vs. never-smokers).[5]
Fusions of ALK with EML4 genes form translocation products that occur in ranges from 3% to 7% in unselected NSCLC and are responsive to pharmacological inhibition of ALK by agents such as crizotinib. Sensitizing fusions of ALK with other genes have also been reported. Other mutations that occur in less than 5% of NSCLC tumors include:
-
HER2, present in 2% of tumors.
-
PI3KCA, present in 2% of tumors.
-
AKT1, present in 1% of tumors.
-
BRAF mutations, present in 1% to 3% of tumors.
BRAF mutations are mutually exclusive of EGFR and KRAS mutations. Somatic mutations in MAP2K1 (also known as MEK) have been identified in 1% of NSCLC. MET oncogene encodes hepatocyte growth factor receptor. Amplification of this gene has been associated with secondary resistance to EGFR tyrosine kinase inhibitors.
References
-
Travis WD, Colby TV, Corrin B, et al.: Histological typing of lung and pleural tumours. 3rd ed. Berlin: Springer-Verlag, 1999.
-
Pao W, Girard N: New driver mutations in non-small-cell lung cancer. Lancet Oncol 12 (2): 175-80, 2011. [PubMed]
-
Tiseo M, Gelsomino F, Boggiani D, et al.: EGFR and EML4-ALK gene mutations in NSCLC: a case report of erlotinib-resistant patient with both concomitant mutations. Lung Cancer 71 (2): 241-3, 2011. [PubMed]
-
Villaruz LC, Socinski MA, Abberbock S, et al.: Clinicopathologic features and outcomes of patients with lung adenocarcinomas harboring BRAF mutations in the Lung Cancer Mutation Consortium. Cancer 121 (3): 448-56, 2015. [PMC free article] [PubMed]
-
D’Angelo SP, Pietanza MC, Johnson ML, et al.: Incidence of EGFR exon 19 deletions and L858R in tumor specimens from men and cigarette smokers with lung adenocarcinomas. J Clin Oncol 29 (15): 2066-70, 2011. [PMC free article] [PubMed]
Stage Information for NSCLC
Background
In non-small cell lung cancer (NSCLC), the determination of stage has important therapeutic and prognostic implications. Careful initial diagnostic evaluation to define the location and to determine the extent of primary and metastatic tumor involvement is critical for the appropriate care of patients.
In general, symptoms, physical signs, laboratory findings, or perceived risk of distant metastasis lead to an evaluation for distant metastatic disease. Additional tests such as bone scans and computed tomography (CT)/magnetic resonance imaging (MRI) of the brain may be performed if initial assessments suggest metastases or if patients with stage III disease are under consideration for aggressive local and combined modality treatments.
Stage has a critical role in the selection of therapy. The stage of disease is based on a combination of clinical factors and pathological factors.[1] The distinction between clinical stage and pathological stage should be considered when evaluating reports of survival outcome.
Procedures used to determine staging include the following:
-
History.
-
Physical examination.
-
Routine laboratory evaluations.
-
Chest x-ray.
-
Chest CT scan with infusion of contrast material.
-
Fluorine F 18-fludeoxyglucose positron emission tomography (18F-FDG PET) scanning.
Procedures used to obtain tissue samples include bronchoscopy, mediastinoscopy, or anterior mediastinotomy. Pathological staging of NSCLC requires the following:
-
Examination of the tumor.
-
Resection margins.
-
Lymph nodes.
Prognostic and treatment decisions are based on some of the following factors:
-
Knowledge of histologic type.
-
Tumor size and location.
-
Involvement of pleura.
-
Surgical margins.
-
Status and location of lymph nodes by station.
-
Tumor grade.
-
Lymphovascular invasion.
At diagnosis, patients with NSCLC can be divided into the following three groups that reflect both the extent of the disease and the treatment approach:
-
Surgically resectable disease (generally stage I, stage II, and selected stage III tumors).
-
Has the best prognosis, which depends on a variety of tumor and host factors.
-
Patients with resectable disease who have medical contraindications to surgery are candidates for curative radiation therapy.
-
Postoperative cisplatin-based combination chemotherapy may provide a survival advantage for patients with resected stage II or stage IIIA NSCLC.
-
-
Locally (T3–T4) and/or regionally (N2–N3) advanced disease.
-
Has a diverse natural history.
-
Selected patients with locally advanced tumors may benefit from combined modality treatments.
-
Patients with unresectable or N2–N3 disease are treated with radiation therapy in combination with chemotherapy.
-
Selected patients with T3 or N2 disease can be treated effectively with surgical resection and either preoperative or postoperative chemotherapy or chemoradiation therapy.
-
-
Distant metastatic disease (includes distant metastases [M1] that were found at the time of diagnosis).
-
May be treated with radiation therapy or chemotherapy for palliation of symptoms of the primary tumor.
-
Patients with good performance status, women, and patients with distant metastases confined to a single site live longer than others.[2]
-
Platinum-based chemotherapy has been associated with short-term palliation of symptoms and with a survival advantage.
-
Currently, no single chemotherapy regimen can be recommended for routine use.
-
Patients previously treated with platinum combination chemotherapy may derive symptom control and survival benefit from docetaxel, pemetrexed, or epidermal growth factor receptor inhibitors.
-
Staging Evaluation
Evaluation of mediastinal lymph node metastasis
Surgical evaluation
Surgical staging of the mediastinum is considered standard if accurate evaluation of the nodal status is needed to determine therapy.
Accurate staging of the mediastinal lymph nodes provides important prognostic information.
Evidence (nodal status):
-
The association between survival and the number of examined lymph nodes during surgery for patients with stage I NSCLC treated with definitive surgical resection was assessed from the population-based Surveillance, Epidemiology, and End Results (SEER) database for the period from 1990 to 2000.[3] A total of 16,800 patients were included in the study.
-
The overall survival analysis for patients without radiation therapy demonstrated that in comparison with the reference group (one to four lymph nodes), patients with five to eight lymph nodes examined during surgery had a modest but statistically significant increase in survival, with a proportionate hazard ratio (HR) of 0.90 (95% confidence interval [CI], 0.84–0.97). For patients with 9 to 12 examined lymph nodes, the HR was 0.86 (95% CI, 0.79–0.95), and for patients with 13 to 16 examined lymph nodes, the HR was 0.78 (95% CI, 0.68–0.90). There appeared to be no incremental improvement after evaluating more than 16 lymph nodes. The corresponding results for lung cancer–specific mortality and for patients receiving radiation therapy were not substantially different.
-
These results indicate that patient survival following resection for NSCLC is associated with the number of lymph nodes evaluated during surgery. Because this is most likely the result of a reduction-of-staging error, namely, a decreased likelihood of missing positive lymph nodes with an increasing number of lymph nodes sampled, it suggests that an evaluation of nodal status should include 11 to 16 lymph nodes.
-
CT imaging
CT scanning is primarily used for determining the size of the tumor. The CT scan should extend inferiorly to include the liver and adrenal glands. MRI scans of the thorax and upper abdomen do not appear to yield advantages over CT scans.[4]
Evidence (CT scan):
-
A systematic review of the medical literature relating to the accuracy of CT scanning for noninvasive staging of the mediastinum in patients with lung cancer has been conducted. In the 35 studies published between 1991 and June 2006, 5,111 evaluable patients were identified. Almost all studies specified that CT scanning was performed following the administration of intravenous contrast material and that a positive test result was defined as the presence of one or more lymph nodes that measured larger than 1 cm on the short-axis diameter.[5]
-
The median prevalence of mediastinal metastasis was 28% (range, 18%–56%).
-
The pooled sensitivity and specificity of CT scanning for identifying mediastinal lymph node metastasis were 51% (95% CI, 47%–54%) for sensitivity and 86% (95% CI, 84%–88%) for specificity. Corresponding positive (3.4%) and negative (0.6%) likelihood ratios were provided.
-
-
The results from the systematic review are similar to those of a large meta-analysis that reported the median sensitivity and specificity of CT scanning for identifying malignant mediastinal nodes as 61% for sensitivity and 79% for specificity.[6]
-
An earlier meta-analysis reported an average sensitivity rate of 64% and specificity rate of 74%.[7]
18F-FDG PET scanning
The wider availability and use of 18F-FDG PET scanning for staging has modified the approach to staging mediastinal lymph nodes and distant metastases.
Randomized trials evaluating the utility of 18F-FDG PET scanning in potentially resectable NSCLC report conflicting results in terms of the relative reduction in the number of noncurative thoracotomies.
Although the current evidence is conflicting, 18F-FDG PET scanning may improve results of early-stage lung cancer by identifying patients who have evidence of metastatic disease that is beyond the scope of surgical resection and that is not evident by standard preoperative staging procedures.
Evidence (18F-FDG PET scan):
-
A systematic review, an expansion of a health technology assessment conducted in 2001 by the Institute for Clinical and Evaluative Sciences, evaluated the accuracy and utility of 18F-FDG PET scanning in the diagnosis and staging of lung cancer.[8] Through a systematic search of the literature, 12 evidence summary reports and 15 prospective studies of the diagnostic accuracy of 18F-FDG PET scanning were identified. 18F-FDG PET scanning appears to be superior to CT imaging for mediastinal staging in NSCLC. 18F-FDG PET scanning also appears to have high sensitivity and reasonable specificity for differentiating benign from malignant lesions as small as 1 cm.
-
A systematic review of the medical literature relating to the accuracy of 18F-FDG PET scanning for noninvasive staging of the mediastinum in patients with lung cancer identified 44 studies published between 1994 and 2006 with 2,865 evaluable patients.[5] The median prevalence of mediastinal metastases was 29% (range, 5%–64%). Pooled estimates of sensitivity and specificity for identifying mediastinal metastasis were 74% (95% CI, 69%–79%) for sensitivity and 85% (95% CI, 82%–88%) for specificity. Corresponding positive (4.9%) and negative (0.3%) likelihood ratios were provided for mediastinal staging with 18F-FDG PET scanning. These findings demonstrated that 18F-FDG PET scanning is more accurate than CT scanning for staging of the mediastinum in patients with lung cancer.
Cost effectiveness of 18F-FDG PET scanning
Decision analyses demonstrate that 18F-FDG PET scanning may reduce the overall costs of medical care by identifying patients with falsely negative CT scans in the mediastinum or otherwise undetected sites of metastases.[9–11] Studies concluded that the money saved by forgoing mediastinoscopy in 18F-FDG PET-positive mediastinal lesions was not justified because of the unacceptably high number of false-positive results.[9–11] A randomized study found that the addition of 18F-FDG PET scanning to conventional staging was associated with significantly fewer thoracotomies.[12] A second randomized trial evaluating the impact of 18F-FDG PET scanning on clinical management found that 18F-FDG PET scanning provided additional information regarding appropriate stage but did not lead to significantly fewer thoracotomies.[13]
Combination of CT imaging and 18F-FDG PET scanning
The combination of CT imaging and 18F-FDG PET scanning has greater sensitivity and specificity than CT imaging alone.[14]
Evidence (CT/18F-FDG PET scan):
-
If there is no evidence of distant metastatic disease on CT scan, 18F-FDG PET scanning complements CT scan staging of the mediastinum. Numerous nonrandomized studies of 18F-FDG PET scanning have evaluated mediastinal lymph nodes using surgery (i.e., mediastinoscopy and/or thoracotomy with mediastinal lymph node dissection) as the gold standard of comparison.
-
In a meta-analysis evaluating the conditional test performance of 18F-FDG PET scanning and CT scanning, the median sensitivity and specificity of 18F-FDG PET scans were reported as 100% for sensitivity and 78% for specificity in patients with enlarged lymph nodes.[6] 18F-FDG PET scanning is considered very accurate in identifying malignant nodal involvement when lymph nodes are enlarged. However, 18F-FDG PET scanning will falsely identify a malignancy in approximately one-fourth of patients with lymph nodes that are enlarged for other reasons, usually as a result of inflammation or infection.[15,16]
-
The median sensitivity and specificity of 18F-FDG PET scanning in patients with normal-sized mediastinal lymph nodes were 82% for sensitivity and 93% for specificity.[6] These data indicate that nearly 20% of patients with normal-sized lymph nodes but with malignant involvement had falsely negative 18F-FDG PET scan findings.
For patients with clinically operable NSCLC, the recommendation is for a biopsy of mediastinal lymph nodes that were found to be larger than 1 cm in shortest transverse axis on chest CT scan or were found to be positive on 18F-FDG PET scan. Negative 18F-FDG PET scanning does not preclude biopsy of radiographically enlarged mediastinal lymph nodes. Mediastinoscopy is necessary for the detection of cancer in mediastinal lymph nodes when the results of the CT scan and 18F-FDG PET scan do not corroborate each other.
Evaluation of brain metastasis
Patients at risk for brain metastases may be staged with CT or MRI scans. One study randomly assigned 332 patients with potentially operable NSCLC and no neurological symptoms to brain CT or MRI imaging to detect occult brain metastasis before lung surgery. MRI showed a trend towards a higher preoperative detection rate than CT scan (P = .069), with an overall detection rate of approximately 7% from pretreatment to 12 months after surgery.[17] Patients with stage I or stage II disease had a detection rate of 4% (i.e., eight detections out of 200 patients); however, individuals with stage III disease had a detection rate of 11.4% (i.e., 15 detections out of 132 patients). The mean maximal diameter of the brain metastases was significantly smaller in the MRI group. Whether the improved detection rate of MRI translates into improved outcome remains unknown. Not all patients are able to tolerate MRI, and for these patients contrast-enhanced CT scan is a reasonable substitute.
Evaluation of distant metastasis other than the brain
Numerous nonrandomized, prospective, and retrospective studies have demonstrated that 18F-FDG PET scanning seems to offer diagnostic advantages over conventional imaging in staging distant metastatic disease; however, standard 18F-FDG PET scans have limitations. 18F-FDG PET scans may not extend below the pelvis and may not detect bone metastases in the long bones of the lower extremities. Because the metabolic tracer used in 18F-FDG PET scanning accumulates in the brain and urinary tract, 18F-FDG PET scanning is not reliable for detection of metastases in these sites.[17]
The Revised International System for Staging Lung Cancer
The Revised International System for Staging Lung Cancer, based on information from a clinical database of more than 5,000 patients, was adopted in 2010 by the American Joint Committee on Cancer (AJCC) and the Union Internationale Contre le Cancer.[18,19] These revisions provide greater prognostic specificity for patient groups; however, the correlation between stage and prognosis predates the widespread availability of PET imaging.
AJCC Stage Groupings and TNM Definitions
The AJCC has designated staging by TNM (tumor, node, metastasis) classification to define NSCLC.[19]
Table 1. Definitions of TNM Occult Carcinomaa
| Stage | TNM | Description |
|---|---|---|
| Occult carcinoma | TX, N0, M0 | TX = Primary tumor cannot be assessed, or tumor proven by the presence of malignant cells in sputum or bronchial washings but not visualized by imaging or bronchoscopy. |
| N0 = No regional lymph node metastasis. | ||
| M0 = No distant metastasis. | ||
| T = primary tumor; N = regional lymph node; M = distant metastasis. | ||
-
aReprinted with permission from AJCC: Lung. In: Amin MB, Edge SB, Greene FL, et al., eds.: AJCC Cancer Staging Manual. 8th ed. New York, NY: Springer, 2017, pp 431–56.
Table 2. Definitions TNM Stage 0a
| Stage | TNM | Description | |
|---|---|---|---|
| 0 | Tis, N0, M0 | Tis = Carcinoma in situ; SCIS =Squamous cell carcinoma in situ; AIS: Adenocarcinoma in situ; Adenocarcinoma with pure lepidic pattern, ≤3 cm in greatest dimension. | |
| N0 = No regional lymph node metastasis. | |||
| M0 = No distant metastasis. | |||
-
T = primary tumor; N = regional lymph node; M = distant metastasis.
-
aReprinted with permission from AJCC: Lung. In: Amin MB, Edge SB, Greene FL, et al., eds.: AJCC Cancer Staging Manual. 8th ed. New York, NY: Springer, 2017, pp 431–56.
Table 3. Definitions of TNM Stages IA1, IA2, IA3, and IBa
| Stage | TNM | Description | ||
|---|---|---|---|---|
| IA1 | T1mi, N0, M0 | T1 = Tumor ≤3 cm in greatest dimension, surrounded by lung or visceral pleura, without bronchoscopic evidence of invasion more proximal than the lobar bronchus (i.e., not in the main bronchus). | ||
| –T1mi = Minimally invasive adenocarcinoma: Adenocarcinoma (≤3 cm in greatest dimension) with a predominantly lepidic pattern and ≤5 mm invasion in greatest dimension. | ||||
| N0 = No regional lymph node metastasis. | ||||
| M0 = No distant metastasis. | ||||
| T1a, N0, M0 | T1 = Tumor ≤3 cm in greatest dimension, surrounded by lung or visceral pleura, without bronchoscopic evidence of invasion more proximal than the lobar bronchus (i.e., not in the main bronchus). | |||
| –T1mi = Minimally invasive adenocarcinoma: adenocarcinoma (≤3 cm in greatest dimension) with a predominantly lepidic pattern and ≤5 mm invasion in greatest dimension. | ||||
| –T1a = Tumor ≤1 cm in greatest dimension. A superficial, spreading tumor of any size whose invasive component is limited to the bronchial wall and may extend proximal to the main bronchus also is classified as T1a, but these tumors are uncommon. | ||||
| N0 = No regional lymph node metastasis. | ||||
| M0 = No distant metastasis. | ||||
| IA2 | T1b, N0, M0 | T1 = Tumor ≤3 cm in greatest dimension, surrounded by lung or visceral pleura, without bronchoscopic evidence of invasion more proximal than the lobar bronchus (i.e., not in the main bronchus). | ||
| –T1mi = Minimally invasive adenocarcinoma: adenocarcinoma (≤3 cm in greatest dimension) with a predominantly lepidic pattern and ≤5 mm invasion in greatest dimension. | ||||
| –T1a = Tumor ≤1 cm in greatest dimension. A superficial, spreading tumor of any size whose invasive component is limited to the bronchial wall and may extend proximal to the main bronchus also is classified as T1a, but these tumors are uncommon. | ||||
| –T1b = Tumor >1 cm but ≤2 cm in greatest dimension. | ||||
| N0 = No regional lymph node metastasis. | ||||
| M0 = No distant metastasis. | ||||
| IA3 | T1c, N0, M0 | T1 = Tumor ≤3 cm in greatest dimension, surrounded by lung or visceral pleura, without bronchoscopic evidence of invasion more proximal than the lobar bronchus (i.e., not in the main bronchus). | ||
| –T1mi = Minimally invasive adenocarcinoma: adenocarcinoma (≤3 cm in greatest dimension) with a predominantly lepidic pattern and ≤5 mm invasion in greatest dimension. | ||||
| –T1a = Tumor ≤1 cm in greatest dimension. A superficial, spreading tumor of any size whose invasive component is limited to the bronchial wall and may extend proximal to the main bronchus also is classified as T1a, but these tumors are uncommon. | ||||
| –T1b = Tumor >1 cm but ≤2 cm in greatest dimension. | ||||
| –T1c = Tumor >2 cm but ≤3 cm in greatest dimension. | ||||
| N0 = No regional lymph node metastasis. | ||||
| M0 = No distant metastasis. | ||||
| IB | T2a, N0, M0 | T2 = Tumor >3 cm but ≤5 cm or having any of the following features: involves the main bronchus regardless of distance to the carina, but without involvement of the carina; invades visceral pleura (PL1 or PL2); associated with atelectasis or obstructive pneumonitis that extends to the hilar region, involving part of rall of the lung. T2 tumors with these features are classified as T2a if ≤4 cm or if the size cannot be determined and T2b if >4 cm but ≤5 cm. | ||
| –T2a = Tumor >3 cm but ≤4 cm in greatest dimension. | ||||
| N0 = No regional lymph node metastasis. | ||||
| M0 = No distant metastasis. | ||||
-
T = primary tumor; N = regional lymph node; M = distant metastasis.
-
aReprinted with permission from AJCC: Lung. In: Amin MB, Edge SB, Greene FL, et al., eds.: AJCC Cancer Staging Manual. 8th ed. New York, NY: Springer, 2017, pp 431–56.
Table 4. Definitions of TNM Stages IIA and IIBa
| Stage | TNM | Description |
|---|---|---|
| IIA | T2b, N0, M0 | T2 = Tumor >3 cm but ≤5 cm or having any of the following features: involves the main bronchus regardless of distance to the carina, but without involvement of the carina; invades visceral pleura (PL1 or PL2); associated with atelectasis or obstructive pneumonitis that extends to the hilar region, involving part of rall of the lung. T2 tumors with these features are classified as T2a if ≤4 cm or if the size cannot be determined and T2b if >4 cm but ≤5 cm. |
| –T2a = Tumor >3 cm but ≤4 cm in greatest dimension. | ||
| –T2b = Tumor >4 cm but ≤5 cm in greatest dimension. | ||
| N0 = No regional lymph node metastasis. | ||
| M0 = No distant metastasis. | ||
| IIB | T1a, N1, M0 | T1 = Tumor ≤3 cm in greatest dimension, surrounded by lung or visceral pleura, without bronchoscopic evidence of invasion more proximal than the lobar bronchus (i.e., not in the main bronchus). |
| –T1a = Tumor ≤1 cm in greatest dimension. A superficial, spreading tumor of any size whose invasive component is limited to the bronchial wall and may extend proximal to the main bronchus also is classified as T1a, but these tumors are uncommon. | ||
| N1 = Metastasis in ipsilateral peribronchial and/or ipsilateral hilar lymph nodes and intrapulmonary nodes, including involvement by direct extension. | ||
| M0 = No distant metastasis. | ||
| T1b, N1, M0 | T1 = Tumor ≤3 cm in greatest dimension, surrounded by lung or visceral pleura, without bronchoscopic evidence of invasion more proximal than the lobar bronchus (i.e., not in the main bronchus). | |
| –T1a = Tumor ≤1 cm in greatest dimension. A superficial, spreading tumor of any size whose invasive component is limited to the bronchial wall and may extend proximal to the main bronchus also is classified as T1a, but these tumors are uncommon. | ||
| –T1b = Tumor >1 cm but ≤2 cm in greatest dimension. | ||
| N1 = Metastasis in ipsilateral peribronchial and/or ipsilateral hilar lymph nodes and intrapulmonary nodes, including involvement by direct extension. | ||
| M0 = No distant metastasis. | ||
| T1c, N1, M0 | T1 = Tumor ≤3 cm in greatest dimension, surrounded by lung or visceral pleura, without bronchoscopic evidence of invasion more proximal than the lobar bronchus (i.e., not in the main bronchus). | |
| –T1a = Tumor ≤1 cm in greatest dimension. A superficial, spreading tumor of any size whose invasive component is limited to the bronchial wall and may extend proximal to the main bronchus also is classified as T1a, but these tumors are uncommon. | ||
| –T1b = Tumor >1 cm but ≤2 cm in greatest dimension. | ||
| –T1c = Tumor >2 cm but ≤3 cm in greatest dimension. | ||
| N1 = Metastasis in ipsilateral peribronchial and/or ipsilateral hilar lymph nodes and intrapulmonary nodes, including involvement by direct extension. | ||
| M0 = No distant metastasis. | ||
| T2a, N1, M0 | T2 = Tumor >3 cm but ≤5 cm or having any of the following features: involves the main bronchus regardless of distance to the carina, but without involvement of the carina; invades visceral pleura (PL1 or PL2); associated with atelectasis or obstructive pneumonitis that extends to the hilar region, involving part of rall of the lung. T2 tumors with these features are classified as T2a if ≤4 cm or if the size cannot be determined and T2b if >4 cm but ≤5 cm. | |
| –T2a = Tumor >3 cm but ≤4 cm in greatest dimension. | ||
| N1 = Metastasis in ipsilateral peribronchial and/or ipsilateral hilar lymph nodes and intrapulmonary nodes, including involvement by direct extension. | ||
| M0 = No distant metastasis. | ||
| T2b, N1, M0 | T2 = Tumor >3 cm but ≤5 cm or having any of the following features: involves the main bronchus regardless of distance to the carina, but without involvement of the carina; invades visceral pleura (PL1 or PL2); associated with atelectasis or obstructive pneumonitis that extends to the hilar region, involving part of rall of the lung. T2 tumors with these features are classified as T2a if ≤4 cm or if the size cannot be determined and T2b if >4 cm but ≤5 cm. | |
| –T2a = Tumor >3 cm but ≤4 cm in greatest dimension. | ||
| –T2b = Tumor >4 cm but ≤5 cm in greatest dimension. | ||
| N1 = Metastasis in ipsilateral peribronchial and/or ipsilateral hilar lymph nodes and intrapulmonary nodes, including involvement by direct extension. | ||
| M0 = No distant metastasis. | ||
| T3, N0, M0 | T3 = Tumor >5 cm but ≤7 cm in greatest dimension or directly invading any of the following: parietal pleura (PL3), chest wall (Including superior sulcus tumors), phrenic nerve, parietal pericardium; or separate tumor nodule(s) in the same lobe as the primary. | |
| N0 = No regional lymph node metastasis. | ||
| M0 = No distant metastasis. |
-
T = primary tumor; N = regional lymph node; M = distant metastasis.
-
aReprinted with permission from AJCC: Lung. In: Amin MB, Edge SB, Greene FL, et al., eds.: AJCC Cancer Staging Manual. 8th ed. New York, NY: Springer, 2017, pp 431–56.
Table 5. Definitions of TNM Stages IIIA, IIIB, and IIICa
| Stage | TNM | Description |
|---|---|---|
| IIIA | T1a, N2, M0 | T1 = Tumor ≤3 cm in greatest dimension, surrounded by lung or visceral pleura, without bronchoscopic evidence of invasion more proximal than the lobar bronchus (i.e., not in the main bronchus). |
| –T1a = Tumor ≤1 cm in greatest dimension. A superficial, spreading tumor of any size whose invasive component is limited to the bronchial wall and may extend proximal to the main bronchus also is classified as T1a, but these tumors are uncommon. | ||
| N2 = Metastasis in ipsilateral mediastinal and/or subcarinal lymph node(s). | ||
| M0 = No distant metastasis. | ||
| T1b, N2, M0 | T1 = Tumor ≤3 cm in greatest dimension, surrounded by lung or visceral pleura, without bronchoscopic evidence of invasion more proximal than the lobar bronchus (i.e., not in the main bronchus). | |
| –T1a = Tumor ≤1 cm in greatest dimension. A superficial, spreading tumor of any size whose invasive component is limited to the bronchial wall and may extend proximal to the main bronchus also is classified as T1a, but these tumors are uncommon. | ||
| –T1b = Tumor >1 cm but ≤2 cm in greatest dimension. | ||
| N2 = Metastasis in ipsilateral mediastinal and/or subcarinal lymph node(s). | ||
| M0 = No distant metastasis. | ||
| T1c, N2, M0 | T1 = Tumor ≤3 cm in greatest dimension, surrounded by lung or visceral pleura, without bronchoscopic evidence of invasion more proximal than the lobar bronchus (i.e., not in the main bronchus). | |
| –T1a = Tumor ≤1 cm in greatest dimension. A superficial, spreading tumor of any size whose invasive component is limited to the bronchial wall and may extend proximal to the main bronchus also is classified as T1a, but these tumors are uncommon. | ||
| –T1b = Tumor >1 cm but ≤2 cm in greatest dimension. | ||
| –T1c = Tumor >2 cm but ≤3 cm in greatest dimension. | ||
| N2 = Metastasis in ipsilateral mediastinal and/or subcarinal lymph node(s). | ||
| M0 = No distant metastasis. | ||
| T2a, N2, M0 | T2 = Tumor >3 cm but ≤5 cm or having any of the following features: involves the main bronchus regardless of distance to the carina, but without involvement of the carina; invades visceral pleura (PL1 or PL2); associated with atelectasis or obstructive pneumonitis that extends to the hilar region, involving part of rall of the lung. T2 tumors with these features are classified as T2a if ≤4 cm or if the size cannot be determined and T2b if >4 cm but ≤5 cm. | |
| –T2a = Tumor >3 cm but ≤4 cm in greatest dimension. | ||
| N2 = Metastasis in ipsilateral mediastinal and/or subcarinal lymph node(s). | ||
| M0 = No distant metastasis. | ||
| T2b, N2, M0 | T2 = Tumor >3 cm but ≤5 cm or having any of the following features: involves the main bronchus regardless of distance to the carina, but without involvement of the carina; invades visceral pleura (PL1 or PL2); associated with atelectasis or obstructive pneumonitis that extends to the hilar region, involving part of rall of the lung. T2 tumors with these features are classified as T2a if ≤4 cm or if the size cannot be determined and T2b if >4 cm but ≤5 cm. | |
| –T2a = Tumor >3 cm but ≤4 cm in greatest dimension. | ||
| –T2b = Tumor >4 cm but ≤5 cm in greatest dimension. | ||
| N2 = Metastasis in ipsilateral mediastinal and/or subcarinal lymph node(s). | ||
| M0 = No distant metastasis. | ||
| T3, N1, M0 | T3 = Tumor >5 cm but ≤7 cm in greatest dimension or directly invading any of the following: parietal pleura (PL3), chest wall (including superior sulcus tumors), phrenic nerve, parietal pericardium; or separate tumor nodule(s) in the same lobe as the primary. | |
| N1 = Metastasis in ipsilateral peribronchial and/or ipsilateral hilar lymph nodes and intrapulmonary nodes, including involvement by direct extension. | ||
| M0 = No distant metastasis. | ||
| T4, N0, M0 | T4 = Tumor >7 cm or tumor of any size invading one or more of the following: diaphragm, mediastinum, heart, great vessels, trachea, recurrent laryngeal nerve, esophagus, vertebral body, or carina; separate tumor nodule(s) in an ipsilateral lobe different from that of the primary. | |
| N0 = No regional lymph node metastasis. | ||
| M0 = No distant metastasis. | ||
| T4, N1, M0 | T4 = Tumor >7 cm or tumor of any size invading one or more of the following: diaphragm, mediastinum, heart, great vessels, trachea, recurrent laryngeal nerve, esophagus, vertebral body, or carina; separate tumor nodule(s) in an ipsilateral lobe different from that of the primary. | |
| N1 = Metastasis in ipsilateral peribronchial and/or ipsilateral hilar lymph nodes and intrapulmonary nodes, including involvement by direct extension. | ||
| M0 = No distant metastasis. | ||
| IIIB | T1a, N3, M0 | T1 = Tumor ≤3 cm in greatest dimension, surrounded by lung or visceral pleura, without bronchoscopic evidence of invasion more proximal than the lobar bronchus (i.e., not in the main bronchus). |
| –T1a = Tumor ≤1 cm in greatest dimension. A superficial, spreading tumor of any size whose invasive component is limited to the bronchial wall and may extend proximal to the main bronchus also is classified as T1a, but these tumors are uncommon. | ||
| N3 = Metastasis in contralateral mediastinal, contralateral hilar, ipsilateral or contralateral scalene, or supraclavicular lymph node(s). | ||
| M0 = No distant metastasis. | ||
| T1b, N3, M0 | T1 = Tumor ≤3 cm in greatest dimension, surrounded by lung or visceral pleura, without bronchoscopic evidence of invasion more proximal than the lobar bronchus (i.e., not in the main bronchus). | |
| –T1a = Tumor ≤1 cm in greatest dimension. A superficial, spreading tumor of any size whose invasive component is limited to the bronchial wall and may extend proximal to the main bronchus also is classified as T1a, but these tumors are uncommon. | ||
| –T1b = Tumor >1 cm but ≤2 cm in greatest dimension. | ||
| N3 = Metastasis in contralateral mediastinal, contralateral hilar, ipsilateral or contralateral scalene, or supraclavicular lymph node(s). | ||
| M0 = No distant metastasis. | ||
| T1c, N3, M0 | T1 = Tumor ≤3 cm in greatest dimension, surrounded by lung or visceral pleura, without bronchoscopic evidence of invasion more proximal than the lobar bronchus (i.e., not in the main bronchus). | |
| –T1a = Tumor ≤1 cm in greatest dimension. A superficial, spreading tumor of any size whose invasive component is limited to the bronchial wall and may extend proximal to the main bronchus also is classified as T1a, but these tumors are uncommon. | ||
| –T1b = Tumor >1 cm but ≤2 cm in greatest dimension. | ||
| –T1c = Tumor >2 cm but ≤3 cm in greatest dimension. | ||
| N3 = Metastasis in contralateral mediastinal, contralateral hilar, ipsilateral or contralateral scalene, or supraclavicular lymph node(s). | ||
| M0 = No distant metastasis. | ||
| T2a, N3, M0 | T2 = Tumor >3 cm but ≤5 cm or having any of the following features: involves the main bronchus regardless of distance to the carina, but without involvement of the carina; invades visceral pleura (PL1 or PL2); associated with atelectasis or obstructive pneumonitis that extends to the hilar region, involving part of rall of the lung. T2 tumors with these features are classified as T2a if ≤4 cm or if the size cannot be determined and T2b if >4 cm but ≤5 cm. | |
| –T2a = Tumor >3 cm but ≤4 cm in greatest dimension. | ||
| N3 = Metastasis in contralateral mediastinal, contralateral hilar, ipsilateral or contralateral scalene, or supraclavicular lymph node(s). | ||
| M0 = No distant metastasis. | ||
| T2b, N3, M0 | T2 = Tumor >3 cm but ≤5 cm or having any of the following features: involves the main bronchus regardless of distance to the carina, but without involvement of the carina; invades visceral pleura (PL1 or PL2); associated with atelectasis or obstructive pneumonitis that extends to the hilar region, involving part of rall of the lung. T2 tumors with these features are classified as T2a if ≤4 cm or if the size cannot be determined and T2b if >4 cm but ≤5 cm. | |
| –T2a = Tumor >3 cm but ≤4 cm in greatest dimension. | ||
| –T2b = Tumor >4 cm but ≤5 cm in greatest dimension. | ||
| N3 = Metastasis in contralateral mediastinal, contralateral hilar, ipsilateral or contralateral scalene, or supraclavicular lymph node(s). | ||
| M0 = No distant metastasis. | ||
| T3, N2, M0 | T3 = Tumor >5 cm but ≤7 cm in greatest dimension or directly invading any of the following: parietal pleura (PL3), chest wall (including superior sulcus tumors), phrenic nerve, parietal pericardium; or separate tumor nodule(s) in the same lobe as the primary. | |
| N2 = Metastasis in ipsilateral mediastinal and/or subcarinal lymph node(s). | ||
| M0 = No distant metastasis. | ||
| T4, N2, M0 | T4 = Tumor >7 cm or tumor of any size invading one or more of the following: diaphragm, mediastinum, heart, great vessels, trachea, recurrent laryngeal nerve, esophagus, vertebral body, or carina; separate tumor nodule(s) in an ipsilateral lobe different from that of the primary. | |
| N2 = Metastasis in ipsilateral mediastinal and/or subcarinal lymph node(s). | ||
| M0 = No distant metastasis. | ||
| IIIC | T3, N3, M0 | T3 = Tumor >5 cm but ≤7 cm in greatest dimension or directly invading any of the following: parietal pleura (PL3), chest wall (including superior sulcus tumors), phrenic nerve, parietal pericardium; or separate tumor nodule(s) in the same lobe as the primary. |
| N3 = Metastasis in contralateral mediastinal, contralateral hilar, ipsilateral or contralateral scalene, or supraclavicular lymph node(s). | ||
| M0 = No distant metastasis. | ||
| T4, N3, M0 | T4 = Tumor >7 cm or tumor of any size invading one or more of the following: diaphragm, mediastinum, heart, great vessels, trachea, recurrent laryngeal nerve, esophagus, vertebral body, or carina; separate tumor nodule(s) in an ipsilateral lobe different from that of the primary. | |
| N3 = Metastasis in contralateral mediastinal, contralateral hilar, ipsilateral or contralateral scalene, or supraclavicular lymph node(s). | ||
| M0 = No distant metastasis. |
-
T = primary tumor; N = regional lymph node; M = distant metastasis.
-
aReprinted with permission from AJCC: Lung. In: Amin MB, Edge SB, Greene FL, et al., eds.: AJCC Cancer Staging Manual. 8th ed. New York, NY: Springer, 2017, pp 431–56.
Table 6. Definitions of TNM Stages IV, IVA, and IVBa
| Stage | TNM | Description |
|---|---|---|
| IV | Any T, Any N, M1 | TX = Primary tumor cannot be assessed, or tumor proven by the presence of malignant cells in sputum or bronchial washings but not visualized by imaging or bronchoscopy. |
| T0 = No evidence of primary tumor. | ||
| Tis = carcinoma in situ; SCIS = squamous cell carcinoma in situ; AIS = adenocarcinoma in situ: Adenocarcinoma with pure lepidic pattern, ≤3 cm in greatest dimension. | ||
| T1 = Tumor ≤3 cm in greatest dimension, surrounded by lung or visceral pleura, without bronchoscopic evidence of invasion more proximal than the lobar bronchus (i.e., not in the main bronchus). | ||
| –T1mi = Minimally invasive adenocarcinoma: Adenocarcinoma (≤3 cm in greatest dimension) with a predominantly lepidic pattern and ≤5 mm invasion in greatest dimension. | ||
| –T1a = Tumor ≤1 cm in greatest dimension. A superficial, spreading tumor of any size whose invasive component is limited to the bronchial wall and may extend proximal to the main bronchus also is classified as T1a, but these tumors are uncommon. | ||
| –T1b = Tumor >1 cm but ≤2 cm in greatest dimension. | ||
| –T1c = Tumor >2 cm but ≤3 cm in greatest dimension. | ||
| T2 = Tumor >3 cm but ≤5 cm or having any of the following features: involves the main bronchus regardless of distance to the carina, but without involvement of the carina; nvades visceral pleura (PL1 or PL2); associated with atelectasis or obstructive pneumonitis that extends to the hilar region, involving part of all of the lung. T2 tumors with these features are classified as T2a if ≤4 cm or if the size cannot be determined and T2b if >4 cm but ≤5 cm. | ||
| –T2a = Tumor >3 cm but ≤4 cm in greatest dimension. | ||
| –T2b = Tumor >4 cm but ≤5 cm in greatest dimension. | ||
| T3 = Tumor >5 cm but ≤7 cm in greatest dimension or directly invading any of the following: parietal pleura (PL3), chest wall (including superior sulcus tumors), phrenic nerve, parietal pericardium; or separate tumor nodule(s) in the same lobe as the primary. | ||
| T4 = Tumor >7 cm or tumor of any size invading one or more of the following: diaphragm, mediastinum, heart, great vessels, trachea, recurrent laryngeal nerve, esophagus, vertebral body, or carina; separate tumor nodule(s) in an ipsilateral lobe different from that of the primary. | ||
| NX = Regional lymph nodes cannot be assessed. | ||
| N0 = No regional lymph node metastasis. | ||
| N1 = Metastasis in ipsilateral peribronchial and/or ipsilateral hilar lymph nodes and intrapulmonary nodes, including involvement by direct extension. | ||
| N2 = Metastasis in ipsilateral mediastinal and/or subcarinal lymph node(s). | ||
| N3 = Metastasis in contralateral mediastinal, contralateral hilar, ipsilateral or contralateral scalene, or supraclavicular lymph node(s). | ||
| M1 = Distant metastasis. | ||
| IVA | Any T, Any N, M1a | Any T = See T descriptions above in Any T, Any N, M1. |
| Any N = See N descriptions above in Any T, Any N, M1. | ||
| M1 = Distant metastasis. | ||
| –M1a = Separate tumor nodule(s) in a contralateral lobe; tumor with pleural or pericardial nodules or malignant pleural or pericardial effusion. Most pleural (pericardial) effusions with lung cancer are a result of the tumor. In a few patients, however, multiple microscopic examinations of pleural (pericardial) fluid are negative for tumor, and the fluid is nonbloody and not an exudate. If these elements and clinical judgment dictate that the effusion is not related to the tumor, the effusion should be excluded as a staging descriptor. | ||
| Any T, Any N, M1b | Any T = See T descriptions above in Any T, Any N, M1. | |
| Any N = See N descriptions above in Any T, Any N, M1. | ||
| M1 = Distant metastasis. | ||
| –M1a = Separate tumor nodule(s) in a contralateral lobe; tumor with pleural or pericardial nodules or malignant pleural or pericardial effusion. Most pleural (pericardial) effusions with lung cancer are a result of the tumor. In a few patients, however, multiple microscopic examinations of pleural (pericardial) fluid are negative for tumor, and the fluid is nonbloody and not an exudate. If these elements and clinical judgment dictate that the effusion is not related to the tumor, the effusion should be excluded as a staging descriptor. | ||
| –M1b = Single extrathoracic metastases in a single organ (including involvement of a single nonregional node). | ||
| IVB | Any T, Any N, M1c | Any T = See T descriptions above in Any T, Any N, M1. |
| Any N = See N descriptions above in Any T, Any N, M1. | ||
| M1 = Distant metastasis. | ||
| –M1a = Separate tumor nodule(s) in a contralateral lobe; tumor with pleural or pericardial nodules or malignant pleural or pericardial effusion. Most pleural (pericardial) effusions with lung cancer are a result of the tumor. In a few patients, however, multiple microscopic examinations of pleural (pericardial) fluid are negative for tumor, and the fluid is nonbloody and not an exudate. If these elements and clinical judgment dictate that the effusion is not related to the tumor, the effusion should be excluded as a staging descriptor. | ||
| –M1b = Single extrathoracic metastases in a single organ (including involvement of a single nonregional node). | ||
| –M1c = Multiple extrathoracic metastases in a single organ or in multiple organs. |
-
T = primary tumor; N = regional lymph node; M = distant metastasis.
-
aReprinted with permission from AJCC: Lung. In: Amin MB, Edge SB, Greene FL, et al., eds.: AJCC Cancer Staging Manual. 8th ed. New York, NY: Springer, 2017, pp 431–56.
Treatment Option Overview for NSCLC
In non-small cell lung cancer (NSCLC), results of standard treatment are poor except for the most localized cancers. All newly diagnosed patients with NSCLC are potential candidates for studies evaluating new forms of treatment.
Surgery is potentially the most curative therapeutic option for this disease. Postoperative chemotherapy may provide an additional benefit to patients with resected NSCLC. Radiation therapy combined with chemotherapy can produce a cure in a small number of patients and can provide palliation in most patients. Prophylactic cranial irradiation may reduce the incidence of brain metastases, but there is no evidence of a survival benefit and the effect of prophylactic cranial irradiation on quality of life is not known.[1,2] In patients with advanced-stage disease, chemotherapy or epidermal growth factor receptor (EGFR) kinase inhibitors offer modest improvements in median survival, although overall survival is poor.[3,4]
Chemotherapy has produced short-term improvement in disease-related symptoms in patients with advanced NSCLC. Several clinical trials have attempted to assess the impact of chemotherapy on tumor-related symptoms and quality of life. In total, these studies suggest that tumor-related symptoms may be controlled by chemotherapy without adversely affecting overall quality of life;[5,6] however, the impact of chemotherapy on quality of life requires more study. In general, medically fit elderly patients with good performance status obtain the same benefits from treatment as younger patients.
The identification of gene mutations in lung cancer has led to the development of molecularly targeted therapy to improve the survival of subsets of patients with metastatic disease.[7] In particular, genetic abnormalities in EGFR, MAPK, and PI3K signaling pathways in subsets of NSCLC may define mechanisms of drug sensitivity and primary or acquired resistance to kinase inhibitors. EGFR mutations strongly predict the improved response rate and progression-free survival of inhibitors of EGFR. Fusions of ALK with EML4 and other genes form translocation products that occur in ranges from 3% to 7% in unselected NSCLC and are responsive to pharmacological inhibition of ALK by agents such as crizotinib. The MET oncogene encodes hepatocyte growth factor receptor. Amplification of this gene has been associated with secondary resistance to EGFR tyrosine kinase inhibitors.
The standard treatment options for each stage of NSCLC are presented in Table 7.
Table 7. Standard Treatment Options for NSCLC
-
ALK = anaplastic lymphoma kinase; BRAF = V-raf murine sarcoma viral oncogene homolog B1; EGFR = epidermal growth factor receptor; MEK = MAPK kinase 1; NSCLC = non-small cell lung cancer; PD-L1 = programmed death-ligand 1; TKI = tyrosine kinase inhibitors; TNM = T, size of tumor and any spread of cancer into nearby tissue; N, spread of cancer to nearby lymph nodes; M, metastasis or spread of cancer to other parts of body.
In addition to the standard treatment options presented in Table 7, treatment options under clinical evaluation include the following:
-
Combining local treatment (surgery).
-
Regional treatment (radiation therapy).
-
Systemic treatments (chemotherapy, immunotherapy, and targeted agents).
-
Developing more effective systemic therapy.
Follow-Up
Several small series have reported that reduction in fluorine F 18-fludeoxyglucose positron emission tomography (18F-FDG PET) after chemotherapy, radiation therapy, or chemoradiation therapy correlates with pathological complete response and favorable prognosis.[8–15] Studies have used different timing of assessments, 18F-FDG PET parameters, and cutpoints to define 18F-FDG PET response. Reduction in maximum standardized uptake value (SUV) of higher than 80% predicted for complete pathological response with a sensitivity of 90%, specificity of 100%, and accuracy of 96%.[16] Median survival after resection was longer for patients with tumor SUV values of lower than 4 (56 months vs. 19 months).[15] Patients with complete metabolic response following radiation therapy were reported to have median survivals of 31 months versus 11 months.[17]
18F-FDG PET may be more sensitive and specific than computed tomography (CT) scan in assessing response to induction therapy. Optimal timing of imaging remains to be defined; however, one study suggested that greater sensitivity and specificity of 18F-FDG PET is achieved if repeat imaging is delayed until 30 days after radiation therapy.[16]
There is no clear role for routine posttreatment PET-CT scans.[18][Level of evidence: 3iiA]
Evidence (surveillance imaging after radiation therapy with or without chemotherapy):
-
A prospective multicenter trial led by the American College of Radiology Imaging Network (ACRIN) and the Radiation Therapy Oncology Group (RTOG) cooperative group (ACRIN 6668/RTOG 0235 [NCT00083083]) studied the role of posttreatment PET-CT at approximately 14 weeks (range, 12–16 weeks) to predict overall survival (OS) after standard-of-care concurrent chemotherapy and radiation therapy in 173 patients with stage III disease.
-
The primary endpoint was to determine the relationship between SUVpeak at a prespecified binary cutoff of SUVpeak 3.5 with OS.
-
The study demonstrated no association between OS and SUVpeak of 3.5 or lower compared with SUVpeak higher than 3.5 with 2-year OS estimates of 51% vs. 37% (P = 0.29).
-
Exploratory analyses showed associations between OS and SUVpeak as a continuous variable, and binary cutoffs of SUVpeak 5.0 and 7.0.
-
Current Clinical Trials
Use our advanced clinical trial search to find NCI-supported cancer clinical trials that are now enrolling patients. The search can be narrowed by location of the trial, type of treatment, name of the drug, and other criteria. General information about clinical trials is also available
Occult NSCLC Treatment
In occult lung cancer, a diagnostic evaluation often includes chest x-ray and selective bronchoscopy with close follow-up (e.g., computed tomography scan), when needed, to define the site and nature of the primary tumor; tumors discovered in this fashion are generally early stage and curable by surgery.
After discovery of the primary tumor, treatment involves establishing the stage of the tumor. Therapy is identical to that recommended for other non-small cell lung cancer (NSCLC) patients with similar-stage disease.
Standard Treatment Options for Occult NSCLC
Standard treatment options for occult NSCLC include the following:
-
Surgery.
Current Clinical Trials
Use our advanced clinical trial search to find NCI-supported cancer clinical trials that are now enrolling patients. The search can be narrowed by location of the trial, type of treatment, name of the drug, and other criteria. General information about clinical trials is also available.
Stage 0 NSCLC Treatment
Stage 0 non-small cell lung cancer (NSCLC) frequently progresses to invasive cancer.[1–3] Patients may be offered surveillance bronchoscopies and, if lesions are detected, potentially curative therapies.
Standard Treatment Options for Stage 0 NSCLC
Standard treatment options for stage 0 NSCLC include the following:
-
Endobronchial therapies, including photodynamic therapy, electrocautery, cryotherapy, and neodymium-doped yttrium aluminium garnet (Nd-YAG) laser therapy.
Surgery
Segmentectomy or wedge resection are used to preserve maximum normal pulmonary tissue because patients with stage 0 NSCLC are at a high risk for second lung cancers. Because these tumors are by definition noninvasive and incapable of metastasizing, they should be curable with surgical resection; however, such lesions, when identified, are often centrally located and may require a lobectomy.
Endobronchial therapies
Patients with central lesions may be candidates for curative endobronchial therapy. Endobronchial therapies that preserve lung function include photodynamic therapy, electrocautery, cryotherapy, and Nd-YAG laser therapy.[3–6]
Evidence (endobronchial therapies):
-
Small case series have reported high complete response rates and long-term survival in selected patients.[7,8][Level of evidence: 3iiiDiii]
Efficacy of these treatment modalities in the management of patients with early NSCLC remains to be proven in definitive randomized controlled trials.
There is a high incidence of second primary cancers developing.[1,2]
Current Clinical Trials
Use our advanced clinical trial search to find NCI-supported cancer clinical trials that are now enrolling patients. The search can be narrowed by location of the trial, type of treatment, name of the drug, and other criteria. General information about clinical trials is also available.
Stages IA and IB NSCLC Treatment
Standard Treatment Options for Stages IA and IB NSCLC
Standard treatment options for stages IA non-small cell lung cancer (NSCLC) and IB NSCLC include the following:
-
Radiation therapy (for patients who cannot have surgery or choose not to have surgery).
Chemotherapy and radiation therapy have not been shown to improve outcomes in stage I NSCLC that has been completely resected.
Surgery
Surgery is the treatment of choice for patients with stage I NSCLC. A lobectomy or segmental, wedge, or sleeve resection may be performed as appropriate. Patients with impaired pulmonary function are candidates for segmental or wedge resection of the primary tumor. Careful preoperative assessment of the patient’s overall medical condition, especially the patient’s pulmonary reserve, is critical in considering the benefits of surgery. The immediate postoperative mortality rate is age related, but a 3% to 5% mortality rate with lobectomy can be expected.[1]
Evidence (surgery):
-
The Lung Cancer Study Group conducted a randomized study (LCSG-821) that compared lobectomy with limited resection for patients with stage I lung cancer. Results of the study showed the following:[2]
-
A reduction in local recurrence for patients treated with lobectomy compared with those treated with limited excision.
-
No significant difference in overall survival (OS).
-
-
Similar results have been reported from a nonrandomized comparison of anatomic segmentectomy and lobectomy.[3]
-
A survival advantage was noted with lobectomy for patients with tumors larger than 3 cm but not for those with tumors smaller than 3 cm.
-
The rate of locoregional recurrence was significantly less after lobectomy, regardless of primary tumor size.
-
-
The Cochrane Collaboration reviewed 11 randomized trials with a total of 1,910 patients who underwent surgical interventions for early-stage (I–IIIA) lung cancer.[5] A pooled analysis of three trials reported the following:
-
Four-year survival was superior in patients with resectable stage I, II, or IIIA NSCLC who underwent resection and complete ipsilateral mediastinal lymph node dissection (CMLND), compared with those who underwent resection and lymph node sampling; the hazard ratio (HR) was estimated to be 0.78 (95% confidence interval [CI], 0.65–0.93, P = .005).[5][Level of evidence: 1iiA]
-
There was a significant reduction in any cancer recurrence (local or distant) in the CMLND group (relative risk [RR], 0.79; 95% CI, 0.66–0.95; P = .01) that appeared mainly because of a reduction in the number of distant recurrences (RR, 0.78; 95% CI, 0.61–1.00; P = .05).
-
There was no difference in operative mortality.
-
Air leak lasting more than 5 days was significantly more common in patients assigned to CMLND (RR, 2.94; 95% CI, 1.01–8.54; P = .05).
-
-
CMLND versus lymph node sampling was evaluated in a large randomized phase III trial (ACOSOG-Z0030[NCT00003831]).[6,7]
-
There was no difference in OS, disease-free survival, local recurrence, and regional recurrence.[7][Level of evidence: 1iiA]
Current evidence suggests that lung cancer resection combined with CMLND is not associated with improvement in survival compared with lung cancer resection combined with systematic sampling of mediastinal lymph nodes in patients with stage I, II, or IIIA NSCLC.[7][Level of evidence: 1iiA]
Limitations of evidence (surgery):
Conclusions about the efficacy of surgery for patients with local and locoregional NSCLC are limited by the small number of participants studied to date and the potential methodological weaknesses of the trials.
Adjuvant therapy
Many patients treated surgically subsequently develop regional or distant metastases.[8] Such patients are candidates for entry into clinical trials evaluating postoperative treatment with chemotherapy or radiation therapy following surgery. At present, neither chemotherapy nor radiation therapy has been found to improve the outcome of patients with stage I NSCLC that has been completely resected.
Adjuvant radiation therapy
The value of postoperative (adjuvant) radiation therapy (PORT) has been evaluated and has not been found to improve the outcome of patients with completely resected stage I NSCLC.[9]
Evidence (adjuvant radiation therapy):
-
A meta-analysis, based on the results of ten randomized controlled trials and 2,232 individuals, reported the following:[9]
-
An 18% relative increase in the risk of death for patients who received PORT compared with surgery alone (HR, 1.18; P = .002). This is equivalent to an absolute detriment of 6% at 2 years (95% CI, 2–9), reducing OS from 58% to 52%. Exploratory subgroup analyses suggested that this detrimental effect was most pronounced for patients with stage I/II, N0-N1 disease, whereas for patients with stage III, N2 disease, there was no clear evidence of an adverse effect.
-
Results for local (HR, 1.13; P = .02), distant (HR, 1.14; P = .02), and overall (HR, 1.10; P = .06) recurrence-free survival similarly showed a detriment of PORT.[9][Level of evidence: 1iiA]
-
Further analysis is needed to determine whether these outcomes can potentially be modified with technical improvements, better definitions of target volumes, and limitation of cardiac volume in the radiation portals.
Adjuvant brachytherapy
The value of intraoperative (adjuvant) brachytherapy applied to the suture line has been evaluated in patients undergoing sublobar resections for stage I NSCLC to improve local control; it has not been found to improve outcomes.
Evidence (adjuvant brachytherapy):
-
A phase III trial that randomly assigned 222 patients to undergo sublobar resection with or without suture line brachytherapy reported the following:[10]
-
No difference in the primary endpoint of local recurrence (5-year estimate, 14.0% vs. 16.7%; P = .59).
-
No difference in OS (5-year estimate, 61.4% vs. 55.6%; P = .38).[10][Level of evidence: 1iiDiii] vs [Level of evidence: 1iiA]
-
Adjuvant chemotherapy
Based on a meta-analysis, postoperative chemotherapy is not recommended outside of a clinical trial for patients with completely resected stage I NSCLC.[11,12][Level of evidence: 1iiA]
Evidence (adjuvant chemotherapy for stage I NSCLC):
-
Data on individual patient outcomes from the five largest trials (4,584 patients) that were conducted after 1995 of cisplatin-based chemotherapy in patients with completely resected NSCLC were collected and pooled into a meta-analysis.[13]
-
With a median follow-up of 5.2 years, the overall HRdeath was 0.89 (95% CI, 0.82–0.96; P = .005), corresponding to a 5-year absolute benefit of 5.4% from chemotherapy.
-
The benefit varied with stage (test for trend, P = .04; HR for stage IA, 1.40; 95% CI, 0.95–2.06; HR for stage IB, 0.93; 95% CI, 0.78–1.10; HR for stage II, 0.83; 95% CI, 0.73–0.95; and HR for stage III, 0.83; 95% CI, 0.72–0.94).
-
The effect of chemotherapy did not vary significantly (test for interaction, P = .11) with the associated drugs, including vinorelbine (HR, 0.80; 95% CI, 0.70–0.91), etoposide or vinca alkaloid (HR, 0.92; 95% CI, 0.80–1.07), or other drugs (HR, 0.97; 95% CI, 0.84–1.13).
-
The apparent greater benefit seen with vinorelbine should be interpreted cautiously as vinorelbine and cisplatin combinations generally required that a higher dose of cisplatin be given. Chemotherapy effect was higher in patients with a better performance status.
-
There was no interaction between chemotherapy effect and any of the following:
-
Sex.
-
Age.
-
Histology.
-
Type of surgery.
-
Planned radiation therapy.
-
Planned total dose of cisplatin.
-
-
Although there is sufficient evidence that postoperative chemotherapy is effective in patients with stage II or stage IIIA NSCLC, its usefulness in patients with stage IB NSCLC is less clear.
Evidence (adjuvant chemotherapy for stage IB NSCLC):
-
The Cancer and Leukemia Group B study (CALGB-9633 [NCT00002852]) addressed the results of adjuvant carboplatin and paclitaxel versus observation for OS in 344 patients with resected stage IB (i.e., pathological T2, N0) NSCLC. Within 4 to 8 weeks of resection, patients were randomly assigned to postoperative chemotherapy or observation.[20]
-
Survival was not significantly different (HR, 0.83; CI, 0.64–1.08; P = .12) at a median follow-up of 74 months.
-
Grades 3 to 4 neutropenia were the predominant toxicity; there were no treatment-related deaths.
-
A post-hoc exploratory analysis demonstrated a significant survival difference in favor of postoperative chemotherapy for patients who had tumors 4 cm or larger in diameter (HR, 0.69; CI, 0.48–0.99; P = .043).
-
Given the magnitude of observed survival differences, CALGB-9633 may have been underpowered to detect small but clinically meaningful improvements in survival. In addition, the use of a carboplatin versus a cisplatin combination might have affected the results. At present, there is no reliable evidence that postoperative chemotherapy improves survival of patients with stage IB NSCLC.[20][Level of evidence: 1iiA]
Radiation therapy
Patients with potentially resectable tumors with medical contraindications to surgery or those with inoperable stage I disease and with sufficient pulmonary reserve may be candidates for radiation therapy with curative intent.
Conventional radiation therapy
Historically, conventional primary radiation therapy consisted of approximately 60 Gy to 70 Gy delivered with megavoltage equipment to the midplane of the known tumor volume using conventional fractionation (1.8–2.0 Gy per day).
Prognosis:
In the largest retrospective conventional radiation therapy series, patients with inoperable disease treated with definitive radiation therapy achieved 5-year survival rates of 10% to 30%.[21–23] Several series demonstrated that patients with T1, N0 tumors had better outcomes, and 5-year survival rates of 30% to 60% were found in this subgroup.[21,22,24] However, local-only failure occurs in as many as 50% of patients treated with conventional radiation therapy to doses in the range of 60 Gy to 65 Gy.[25,26]
Evidence (conventional radiation therapy):
-
A single report of patients older than 70 years who had resectable lesions smaller than 4 cm but who had medically inoperable disease or who refused surgery reported the following:[24]
-
Survival at 5 years after radiation therapy with curative intent was comparable with a historical control group of patients of similar age who were resected with curative intent.
-
-
A small case series using matched controls reported the following:[4]
-
The addition of endobronchial brachytherapy improved local disease control compared with external-beam radiation therapy (EBRT).[4][Level of evidence: 3iiiDiii]
-
A substantial number of patients are ineligible for standard surgical resection because of comorbid conditions that are associated with unacceptably high perioperative risk. Observation and radiation therapy may be considered for these patients.[27–29] Nonrandomized observational studies comparing treatment outcomes associated with resection, radiation therapy, and observation have demonstrated shorter survival times and higher mortality for patients treated with observation only.[27,30]
Improvements in radiation techniques include planning techniques to account for tumor motion, more conformal planning techniques (e.g., 3-D conformal radiation therapy and intensity-modulated radiation therapy), and image guidance during treatment. Modern approaches to delivery of EBRT include hypofractionated radiation therapy and stereotactic body radiation therapy (SBRT).However, there are limited reliable data from comparative trials to determine which approaches yield superior outcomes.[28,29]
Hypofractionated radiation therapy
Hypofractionated radiation therapy involves the delivery of a slightly higher dose of radiation therapy per day (e.g., 2.4–4.0 Gy) over a shorter period of time compared with conventionally fractionated radiation therapy. Multiple prospective phase I/II trials have demonstrated that hypofractionated radiation therapy to a dose of 60 Gy to 70 Gy delivered over 3 to 4 weeks with 2.4 Gy to 4.0 Gy per day resulted in a low incidence of moderate to severe toxicity, 2-year OS of 50% to 60%, and 2-year tumor local control of 80% to 90%.[31–33][Level of evidence: 3iiiA]
Stereotactic body radiation therapy (SBRT)
SBRT involves the delivery of highly conformal, high-dose radiation therapy over an extremely hypofractionated course (e.g., one to five treatments) delivered over 1 to 2 weeks. Commonly used regimens include 18 Gy × 3, 12 Gy to 12.5 Gy × 4, and 10 Gy to 12 Gy × 5, and deliver a substantially higher biologically effective dose compared with historic conventional radiation therapy regimens.
Multiple prospective phase I/II trials and institutional series have demonstrated that SBRT results in a low incidence of pulmonary toxicity (<10% risk of symptomatic radiation pneumonitis), 2-year OS of 50% to 60%, and 2-year tumor control of 90% to 95%.[34–40][Level of evidence: 3iiiA]
Evidence (SBRT):
-
Early phase I/II trials from Indiana University identified the maximum tolerated dose of three-fraction SBRT at 18 Gy × 3 for T1 tumors, and this regimen resulted in 2-year OS of 55% and 2-year local tumor control of 95%.
-
An unacceptably high incidence (8.6%) of grade 5 toxicity was observed in patients with central tumors (defined as within 2 cm of the tracheobronchial tree from the trachea to the level of the lobar bronchi).[35]
-
-
A subsequent multicenter trial (RTOG-0236 [NCT00087438]) studied the 18 Gy × 3 regimen in 55 patients with peripheral T1 to T2 tumors only and demonstrated 3-year OS of 56% and 3-year primary tumor control of 98%.
-
The incidence of moderate to severe toxicity was low, with grade 3 toxicity in 24% of patients, grade 4 toxicity in 4% of patients, and no grade 5 toxicity, with a 4% incidence of grade 3 radiation pneumonitis.[39]
-
-
In the largest reported series from VU University Medical Center Amsterdam, 676 patients with T1 to T2 tumors were treated with three-, five-, and eight-fraction SBRT using a risk-adapted approach (a tailored fractionation regimen based on tumor proximity to critical organs).
-
With a median follow-up of 32.9 months, the median OS was 40.7 months, and 2-year local tumor control was 95%.[40]
-
-
While central location is a contraindication to three-fraction SBRT based on data from the Indiana phase II study, a subsequent systematic review of published reports of 315 patients with 563 central tumors demonstrated a much lower incidence of severe toxicity, including a 1% to 5% risk of grade 5 events with more protracted SBRT regimens (e.g., four to ten fractions).[41] A multicenter phase I/II trial (RTOG-0813[NCT00750269]) is ongoing to identify the maximum tolerated dose for a five-fraction SBRT regimen for central tumors.
Randomized trials of conventional radiation therapy versus SBRT (NCT01014130), and hypofractionated radiation therapy versus SBRT (LUSTRE [NCT01968941]) are ongoing to determine the optimal radiation therapy regimen, but stereotactic body radiation therapy has been widely adopted for patients with medically inoperable stage I NSCLC.
Treatment Options Under Clinical Evaluation
Treatment options under clinical evaluation include the following:
-
Clinical trials of postoperative chemoprevention (as evidenced in the Eastern Cooperative Oncology Group (ECOG) (ECOG-5597 [NCT00008385] trial, for example).
-
Endobronchial therapies, including photodynamic therapy, for highly selected patients with T1, N0, M0 tumors.
Current Clinical Trials
Use our advanced clinical trial search to find NCI-supported cancer clinical trials that are now enrolling patients. The search can be narrowed by location of the trial, type of treatment, name of the drug, and other criteria. General information about clinical trials is also available.
Stages IIA and IIB NSCLC Treatment
Standard Treatment Options for Stages IIA and IIB NSCLC
Standard treatment options for stages IIA non-small cell lung cancer (NSCLC) and IIB NSCLC include the following:
-
Radiation therapy (for patients who cannot have surgery).
Adjuvant radiation therapy has not been shown to improve outcomes in patients with stage II NSCLC.
Surgery
Surgery is the treatment of choice for patients with stage II NSCLC. A lobectomy, pneumonectomy, or segmental resection, wedge resection, or sleeve resection may be performed as appropriate. Careful preoperative assessment of the patient’s overall medical condition, especially the patient’s pulmonary reserve, is critical in considering the benefits of surgery. Despite the immediate and age-related postoperative mortality rate, a 5% to 8% mortality rate with pneumonectomy or a 3% to 5% mortality rate with lobectomy can be expected.
Evidence (surgery):
-
The Cochrane Collaboration reviewed 11 randomized trials with a total of 1,910 patients who underwent surgical interventions for early-stage (I–IIIA) lung cancer.[1] A pooled analysis of three trials reported the following:
-
Four-year survival was superior in patients with resectable stage I, II, or IIIA NSCLC who underwent resection and complete ipsilateral mediastinal lymph node dissection (CMLND), compared with those who underwent resection and lymph node sampling; the hazard ratio (HR) was estimated to be 0.78 (95% confidence interval [CI], 0.65–0.93; P = .005).[1][Level of evidence: 1iiA]
-
There was a significant reduction in any cancer recurrence (local or distant) in the CMLND group (relative risk [RR], 0.79; 95% CI, 0.66–0.95; P = .01) that appeared mainly as the result of a reduction in the number of distant recurrences (RR, 0.78; 95% CI, 0.61–1.00; P = .05).
-
There was no difference in operative mortality.
-
Air leak lasting more than 5 days was significantly more common in patients assigned to CMLND (RR, 2.94; 95% CI, 1.01–8.54; P = .05).
-
-
CMLND versus lymph node sampling was evaluated in a large randomized phase III trial (ACOSOG-Z0030[NCT00003831]).[2]
-
Preliminary analyses of operative morbidity and mortality showed comparable rates from the procedures.[2]
-
There was no difference in overall survival (OS), disease-free survival (DFS), local recurrence, and regional recurrence.[3][Level of evidence: 1iiA]
-
Current evidence suggests that lung cancer resection combined with CMLND is not associated with improvement in survival compared with lung cancer resection combined with systematic sampling of mediastinal lymph nodes in patients with stage I, II, or IIIA NSCLC.[3][Level of evidence: 1iiA]
Limitations of evidence (surgery):
Conclusions about the efficacy of surgery for patients with local and locoregional NSCLC are limited by the small number of participants studied to date and potential methodological weaknesses of the trials.
Adjuvant chemotherapy
The preponderance of evidence indicates that postoperative cisplatin combination chemotherapy provides a significant survival advantage to patients with resected stage II NSCLC. Preoperative chemotherapy may also provide survival benefit. The optimal sequence of surgery and chemotherapy and the benefits and risks of postoperative radiation therapy in patients with resectable NSCLC remain to be determined.
After surgery, many patients develop regional or distant metastases.[4] Several randomized, controlled trials and meta-analyses have evaluated the use of postoperative chemotherapy in patients with stage I, II, and IIIA NSCLC.[5–11]
Evidence (adjuvant chemotherapy):
-
Data on individual patient outcomes were collected and pooled into a meta-analysis from the five largest trials (4,584 patients) that were conducted after 1995 of cisplatin-based chemotherapy in patients with completely resected NSCLC.[7]
-
With a median follow-up time of 5.2 years, the overall HRdeath was 0.89 (95% CI, 0.82–0.96; P = .005), corresponding to a 5-year absolute benefit of 5.4% from chemotherapy.
-
The benefit varied with stage (test for trend, P = .04; HR for stage IA, 1.40; 95% CI, 0.95–2.06; HR for stage IB, 0.93; 95% CI, 0.78–1.10; HR for stage II, 0.83; 95% CI, 0.73–0.95; and HR for stage III, 0.83; 95% CI, 0.72–0.94).
-
The effect of chemotherapy did not vary significantly (test for interaction, P = .11) with the associated drugs, including vinorelbine (HR, 0.80; 95% CI, 0.70–0.91), etoposide or vinca alkaloid (HR, 0.92; 95% CI, 0.80–1.07), or other drugs (HR, 0.97; 95% CI, 0.84–1.13).
-
The greater effect on survival observed with the doublet of cisplatin plus vinorelbine compared with other regimens should be interpreted cautiously as the total dose of cisplatin received was significantly higher in patients treated with vinorelbine.
-
-
The meta-analysis and the individual studies [5,12] support the administration of postoperative cisplatin-based chemotherapy in combination with vinorelbine.
-
Superior OS for the trial population and patients with stage II disease was reported for the LACE pooled analysis (pooled HR, 0.83; 95% CI, 0.73–0.95); the Adjuvant Navelbine International Trialist Association (ANITA) trial (HR, 0.71; 95% CI, 0.49–1.03); and the National Cancer Institute of Canada Clinical Trials Group JBR.10 trial (HR, 0.59; 95% CI, 0.42–0.85).
-
Chemotherapy effect was higher in patients with better performance status (PS).
-
There was no interaction between chemotherapy effect and any of the following:
-
Sex.
-
Age.
-
Histology.
-
Type of surgery.
-
Planned radiation therapy.
-
Planned total dose of cisplatin.
-
-
-
In a retrospective analysis of a phase III trial of postoperative cisplatin and vinorelbine, patients older than 65 years were found to benefit from treatment.[13]
-
Chemotherapy significantly prolonged OS for elderly patients (HR, 0.61; 95% CI, 0.38–0.98; P = .04).
-
There were no significant differences in toxic effects, hospitalization, or treatment-related death by age group, although elderly patients received less treatment.[13]
-
Based on these data, patients with completely resected stage II lung cancer may benefit from postoperative cisplatin-based chemotherapy.[13][Level of evidence: 1iiA]
Neoadjuvant chemotherapy
The role of chemotherapy before surgery was tested in clinical trials. The proposed benefits of preoperative chemotherapy include the following:
-
A reduction in tumor size that may facilitate surgical resection.
-
Early eradication of micrometastases.
-
Better tolerability.
Preoperative chemotherapy may, however, delay potentially curative surgery.
Evidence (neoadjuvant chemotherapy):
-
The Cochrane Collaboration reported a systematic review and meta-analysis of seven randomized controlled trials that included 988 patients and evaluated the addition of preoperative chemotherapy to surgery versus surgery alone. These trials evaluated patients with stages I, II, and IIIA NSCLC.[14]
-
Preoperative chemotherapy provided an absolute benefit in survival of 6% across all stages of disease, from 14% to 20% at 5 years (HR, 0.82; 95% CI, 0.69–0.97; P = .022).[14][Level of evidence: 1iiA]
-
This analysis was unable to address questions such as whether particular types of patients may benefit more or less from preoperative chemotherapy.
-
-
In the largest trial reported to date, 519 patients were randomly assigned to receive either surgery alone or three cycles of platinum-based chemotherapy followed by surgery. Most patients (61%) had clinical stage I disease; 31% had stage II disease; and 7% had stage III disease.[15]
-
No survival advantage was seen.[15]
-
Postoperative complications were similar between groups, and no impairment of quality of life was observed.
-
There was no evidence of a benefit in terms of OS (HR, 1.02; 95% CI, 0.80–1.31; P = .86).
-
Updating the systematic review by addition of the present result suggests a 12% relative survival benefit with the addition of neoadjuvant (preoperative) chemotherapy (1,507 patients; HR, 0.88; 95% CI, 0.76–1.01; P = .07), equivalent to an absolute improvement in survival of 5% at 5 years.
-
Adjuvant radiation therapy
The value of postoperative (adjuvant) radiation therapy (PORT) has been evaluated.[16]
Evidence (adjuvant radiation therapy):
-
A meta-analysis, based on the results of ten randomized controlled trials and 2,232 individuals, reported the following:[16]
-
An 18% relative increase in the risk of death for patients who received PORT compared with surgery alone (HR, 1.18; P = .002). This is equivalent to an absolute detriment of 6% at 2 years (95% CI, 2%–9%), reducing OS from 58% to 52%. Exploratory subgroup analyses suggested that this detrimental effect was most pronounced for patients with stage I/II, N0–N1 disease, whereas for patients with stage III, N2 disease there was no clear evidence of an adverse effect.
-
Results for local (HR, 1.13; P = .02), distant (HR, 1.14; P = .02), and overall (HR, 1.10; P = .06) recurrence-free survival similarly showed a detriment of PORT.[16][Level of evidence: 1iiA]
-
Further analysis is needed to determine whether these outcomes can potentially be modified with technical improvements, better definitions of target volumes, and limitation of cardiac volume in the radiation portals.
Radiation therapy
Patients with potentially operable tumors with medical contraindications to surgery or those with inoperable stage II disease and with sufficient pulmonary reserve are candidates for radiation therapy with curative intent.[17] Primary radiation therapy often consists of approximately 60 Gy delivered with megavoltage equipment to the midplane of the volume of the known tumor using conventional fractionation. A boost to the cone down field of the primary tumor is frequently used to enhance local control. Careful treatment planning with precise definition of target volume and avoidance of critical normal structures, to the extent possible, is needed for optimal results; this requires the use of a simulator.
Prognosis:
Among patients with excellent PS, a 3-year survival rate of 20% may be expected if a course of radiation therapy with curative intent can be completed.
Evidence (radiation therapy):
-
In the largest retrospective series reported to date, 152 patients with medically inoperable NSCLC were treated with definitive radiation therapy. The study reported the following:[18]
-
A 5-year OS rate of 10%.
-
Forty-four patients with T1 tumors achieved an actuarial DFS rate of 60%.
-
This retrospective study also suggested that improved DFS was obtained with radiation therapy doses greater than 60 Gy.[18]
-
Treatment Options Under Clinical Evaluation
Treatment options under clinical evaluation include the following:
-
Clinical trials of radiation therapy after curative surgery.
Current Clinical Trials
Use our advanced clinical trial search to find NCI-supported cancer clinical trials that are now enrolling patients. The search can be narrowed by location of the trial, type of treatment, name of the drug, and other criteria. General information about clinical trials is also available.
Stage IIIA NSCLC Treatment
Patients with stage IIIA non-small cell lung cancer (NSCLC) are a heterogenous group. Patients may have metastases to ipsilateral mediastinal nodes, potentially resectable T3 tumors invading the chest wall, or mediastinal involvement with metastases to peribronchial or hilar lymph nodes (N1). Presentations of disease range from resectable tumors with microscopic metastases to lymph nodes to unresectable, bulky disease involving multiple nodal stations.
Prognosis:
Patients with clinical stage IIIA N2 disease have a 5-year overall survival (OS) rate of 10% to 15%; however, patients with bulky mediastinal involvement (i.e., visible on chest radiography) have a 5-year survival rate of 2% to 5%. Depending on clinical circumstances, the principal forms of treatment that are considered for patients with stage IIIA NSCLC are radiation therapy, chemotherapy, surgery, and combinations of these modalities.
Treatment options vary according to the location of the tumor and whether it is resectable.
Standard Treatment Options for Resected/Resectable Stage IIIA N2 NSCLC
Despite careful preoperative staging, some patients will be found to have metastases to mediastinal N2 lymph nodes at thoracotomy.
Standard treatment options for resected/resectable disease include the following:
The preponderance of evidence indicates that postoperative cisplatin combination chemotherapy provides a significant survival advantage to patients with resected NSCLC with occult N2 disease discovered at surgery. The optimal sequence of surgery and chemotherapy and the benefits and risks of postoperative radiation therapy in patients with resectable NSCLC are yet to be determined.
Surgery
If complete resection of tumor and lymph nodes is possible, such patients may benefit from surgery followed by postoperative chemotherapy. Current evidence suggests that lung cancer resection combined with complete ipsilateral mediastinal lymph node dissection (CMLND) is not associated with improvement in survival compared with lung cancer resection combined with systematic sampling of mediastinal lymph nodes in patients with stage I, II, or IIIA NSCLC.[1][Level of evidence: 1iiA]
The addition of surgery to chemoradiation therapy for patients with stage IIIA NSCLC did not result in improved OS in a phase III trial but did improve progression-free survival (PFS) and local control.[2][Level of evidence: 1iiDiii]
Evidence (surgery):
-
The Cochrane Collaboration reviewed 11 randomized trials with a total of 1,910 patients who underwent surgical interventions for early-stage (I–IIIA) lung cancer.[3] A pooled analysis of three trials reported the following:
-
Four-year survival was superior in patients with resectable stage I, II, or IIIA NSCLC who underwent resection and CMLND, compared with those who underwent resection and lymph node sampling; the hazard ratio (HR) was estimated to be 0.78 (95% confidence interval [CI], 0.65–0.93; P = .005).[3][Level of evidence: 1iiA]
-
-
CMLND versus lymph node sampling was evaluated in a large randomized phase III trial (ACOSOG-Z0030). Preliminary analyses of operative morbidity and mortality showed comparable rates from the procedures.[4]
-
There was no difference in OS, disease-free survival (DFS), local recurrence, and regional recurrence.[1][Level of evidence: 1iiA]
-
Limitations of evidence (surgery):
Conclusions about the efficacy of surgery for patients with local and locoregional NSCLC are limited by the small number of participants studied to date and by the potential methodological weaknesses of the trials.
Neoadjuvant therapy
Neoadjuvant chemotherapy
The role of chemotherapy before surgery in patients with stage III N2 NSCLC has been extensively tested in clinical trials. The proposed benefits of preoperative (neoadjuvant) chemotherapy include the following:
-
A reduction in tumor size that may facilitate surgical resection.
-
Early eradication of micrometastases.
-
Better tolerability.
Evidence (neoadjuvant chemotherapy):
-
The Cochrane Collaboration provided a systematic review and meta-analysis of seven randomized controlled trials that included 988 patients and evaluated the addition of preoperative chemotherapy to surgery versus surgery alone.[5] These trials evaluated patients with stages I, II, and IIIA NSCLC.
-
Preoperative chemotherapy provided an absolute benefit in survival of 6% across all stages of disease, from 14% to 20% at 5 years (HR, 0.82; 95% CI, 0.69–0.97; P = .022).[5][Level of evidence: 1iiA]
-
This analysis was unable to address questions such as whether particular types of patients may benefit more or less from preoperative chemotherapy.[6]
-
-
In the largest trial reported to date, 519 patients were randomly assigned to receive either surgery alone or three cycles of platinum-based chemotherapy followed by surgery.[7] Most patients (61%) had clinical stage I disease, 31% had stage II disease, and 7% had stage III disease.
-
Postoperative complications were similar between groups, and no impairment of quality of life was observed.
-
There was no evidence of a benefit in terms of OS (HR, 1.02; 95% CI, 0.80–1.31; P = .86).
-
Updating the systematic review by addition of the present result suggests a 12% relative survival benefit with the addition of preoperative chemotherapy (1,507 patients, HR, 0.88; 95% CI, 0.76–1.01; P = .07), equivalent to an absolute improvement in survival of 5% at 5 years.[7]
-
Neoadjuvant chemoradiation therapy
Administering concurrent neoadjuvant chemotherapy and radiation therapy before surgery may intensify treatment and increase the likelihood of downstaging the tumor burden. Commonly utilized regimens that have been tested in the phase II setting include cisplatin/etoposide (EP5050) and weekly carboplatin/paclitaxel.[8,9] In a randomized trial of neoadjuvant chemoradiation therapy and surgery versus concurrent chemoradiation therapy alone, there was no difference in OS, but surgery improved PFS and local control.[2][Level of evidence: 1iiDiii]
Evidence (neoadjuvant chemoradiation therapy):
-
The Intergroup-0139 [NCT00002550] trial compared chemoradiation therapy alone with neoadjuvant chemoradiation followed by surgery in 396 patients with stage IIIA NSCLC.[2]
-
Surgery did not improve OS (5-year OS, 27% vs. 20%; HR: 0.87 [0.70–1.10]; P = .24).
-
Surgery improved PFS (5-year PFS, 22% vs. 11%; HR 0.77 [0.62–0.96]; P = .017) and decreased the risk of local recurrence (10% vs. 22%; P = .002).
-
There was increased treatment mortality with neoadjuvant chemoradiation with surgery (8% vs. 2%), particularly in the subset of patients who underwent pneumonectomy.
-
A direct comparison of neoadjuvant chemotherapy versus neoadjuvant chemoradiation therapy using modern treatment regimens has not been performed to date; the optimal neoadjuvant approach remains unclear.
Adjuvant therapy
Adjuvant chemotherapy
Patients with completely resected stage IIIA NSCLC may benefit from postoperative cisplatin-based chemotherapy.[10][Level of evidence: 1iiA]
Evidence (adjuvant chemotherapy):
Evidence from randomized controlled clinical trials indicates that when stage IIIA NSCLC is encountered unexpectedly at surgery, chemotherapy given after complete resection improves survival.
Several randomized, controlled trials and meta-analyses have evaluated the use of postoperative chemotherapy in patients with stages I, II, and IIIA NSCLC.[10–16]
-
Data on individual patient outcomes from the five largest trials (4,584 patients) that were conducted after 1995 of cisplatin-based chemotherapy in patients with completely resected NSCLC were collected and pooled into a meta-analysis.[10]
-
With a median follow-up of 5.2 years, the overall HRdeath was 0.89 (95% CI, 0.82–0.96; P = .005), corresponding to a 5-year absolute benefit of 5.4% from chemotherapy.
-
The effect of chemotherapy did not vary significantly (test for interaction, P = .11) with the associated drugs, including vinorelbine (HR, 0.80; 95% CI, 0.70–0.91), etoposide or vinca alkaloid (HR, 0.92; 95% CI, 0.80–1.07), or other drugs (HR, 0.97; 95% CI, 0.84–1.13).
-
The benefit varied with stage (HR for stage IIIA, 0.83; 95% CI, 0.72–0.94).
-
The greater effect on survival observed with the doublet of cisplatin plus vinorelbine compared with other regimens should be interpreted with caution as the total dose of cisplatin received was significantly higher in patients treated with vinorelbine.
-
-
Two trials (FRE-IALT and the Adjuvant Navelbine International Trialist Association [ANITA] trial) reported significant OS benefits associated with postoperative chemotherapy in stage IIIA disease.[6,12]
-
For the subgroup of stage IIIA patients in the ANITA trial (n = 325), the HR was 0.69 (95% CI, 0.53–0.90), and the result for the FRE-IALT trial (n = 728) was HR, 0.79 (95% CI, 0.66–0.95).
-
The chemotherapy effect was higher in patients with a better performance status (PS).
-
There was no interaction between the chemotherapy effect and any of the following:
-
Sex.
-
Age.
-
Histology.
-
Type of surgery.
-
Planned radiation therapy.
-
Planned total dose of cisplatin.
-
-
-
In a retrospective analysis of a phase III trial of postoperative cisplatin and vinorelbine, patients older than 65 years were found to benefit from treatment.[17]
-
Chemotherapy significantly prolonged OS for elderly patients (HR, 0.61; 95% CI, 0.38–0.98; P = .04).
-
There were no significant differences in toxic effects, hospitalization, or treatment-related death by age group, although elderly patients received less treatment.
-
Adjuvant chemoradiation therapy
Combination chemotherapy and radiation therapy administered before or following surgery should be viewed as investigational and requiring evaluation in future clinical trials.
Evidence (adjuvant chemoradiation therapy):
-
Five randomized trials have assessed the value of postoperative combination chemoradiation therapy versus radiation therapy following surgical resection.[5,7,18–20][Level of evidence: 1iiA]
-
Only one trial reported improved DFS and no trial reported improved OS.
-
-
Three trials have evaluated platinum-based combination chemotherapy followed by surgery versus platinum-based chemotherapy followed by radiation therapy (60–69.6 Gy) alone to determine whether surgery or radiation therapy was most efficacious.[20–22] Although the studies were small, enrolling 73 (Radiation Therapy Oncology Group [RTOG]) (RTOG 89-01), 107 (The University of Texas M.D. Anderson Cancer Center), and 333 (European Organization for Research and Treatment of Cancer [EORTC-08941; NCT00002623]) patients with stage IIIA N2 disease, no trial reported a difference in local control or survival.[20–22][Level of evidence: 1iiA]
-
In the largest series (EORTC-08941), 579 patients with histologic- or cytologic-proven stage IIIA N2 NSCLC were given three cycles of platinum-based induction chemotherapy.[22] The 333 responding patients were subsequently randomly assigned to surgical resection or radiation therapy. Of the 154 patients (92%) who underwent surgery, 50% had a radical resection, 42% had a pathologic downstaging, and 5% had a pathologic complete response; 4% died after surgery. Postoperative (adjuvant) radiation therapy (PORT) was administered to 62 patients (40%) in the surgery arm. Among the 154 patients (93%) who received radiation therapy, overall compliance to the radiation therapy prescription was 55%, and grade 3 to 4 acute and late esophageal and pulmonary toxic effects occurred in 4% and 7% of patients; one patient died of radiation pneumonitis.
-
Median OS was 16.4 months for patients assigned to resection versus 17.5 months for patients assigned to radiation therapy; 5-year OS was 15.7% for patients assigned to resection versus 14% for patients assigned to radiation therapy (HR, 1.06; 95% CI, 0.84–1.35).[22]
-
Rates of PFS were also similar in both groups. In view of its low morbidity and mortality, it was concluded that radiation therapy should be considered the preferred locoregional treatment for these patients.[22]
-
-
Adjuvant radiation therapy
The value of PORT has been assessed.[18] Although some studies suggest that PORT can improve local control for node-positive patients whose tumors were resected, it remains controversial whether it can improve survival. The optimal dose of thoracic PORT is not known at this time. The majority of studies cited used doses ranging from 30 Gy to 60 Gy, typically provided in 2 Gy to 2.5 Gy fractions.[18]
As referred to in the National Cancer Institute of Canada (NCIC) Clinical Trials Group JBR.10 study (NCT00002583), PORT may be considered in selected patients to reduce the risk of local recurrence, if any of the following are present:[17]
-
Involvement of multiple nodal stations.
-
Extracapsular tumor spread.
-
Close or microscopically positive resection margins.
Evidence (adjuvant radiation therapy):
Evidence from one large meta-analysis, subset analyses of randomized trials, and one large population study suggest that PORT may reduce local recurrence. Results from these studies on the effect of PORT on OS are conflicting.
-
A meta-analysis of ten randomized trials that evaluated PORT versus surgery alone showed the following:
-
No difference in OS for the entire PORT group or for the subset of N2 patients.[12][Level of evidence: 1iiA]
-
-
Results from a nonrandomized subanalysis of the ANITA trial, comparing 5-year OS in N2 patients who did or did not receive PORT, found the following:[6]
-
Higher survival rates in patients who received radiation therapy in the observation arm (21% in patients who received PORT vs. 17% in patients who did not receive PORT) and in the chemotherapy arm (47% with PORT vs. 34% without PORT); however, statistical tests of comparison were not conducted.[6]
-
-
Results from the Surveillance, Epidemiology, and End Results (SEER) program [19] suggest the following:
-
The large SEER retrospective study (N = 7,465) found superior survival rates associated with radiation therapy in N2 disease (HR, 0.855; 95% CI, 0.762–0.959).
-
There is benefit of PORT in stage IIIA N2 disease, and the role of PORT in early stages of NSCLC should be clarified in ongoing phase III trials. Further analysis is needed to determine whether these outcomes can be modified with technical improvements, better definitions of target volumes, and limitation of cardiac volume in the radiation portals.[12]
Standard Treatment Options for Unresectable Stage IIIA N2 NSCLC
Standard treatment options for patients with unresectable NSCLC include the following:
Radiation therapy
For treatment of locally advanced unresectable tumor
Radiation therapy alone, administered sequentially with chemotherapy and concurrently with chemotherapy, may provide benefit to patients with locally advanced unresectable stage III NSCLC.
Prognosis:
Radiation therapy with traditional dose and fractionation schedules (1.8–2.0 Gy per fraction per day to 60–70 Gy in 6–7 weeks) results in reproducible long-term survival benefit in 5% to 10% of patients and significant palliation of symptoms.[23]
Evidence (radiation therapy for locally advanced unresectable tumor):
-
One prospective randomized clinical study showed the following:[24]
-
Radiation therapy given continuously (including weekends) as three daily fractions (continuous hyperfractionated accelerated radiation therapy) improved OS compared with radiation therapy given as one daily fraction.[24][Level of evidence: 1iiA]
-
Patterns of failure for patients treated with radiation therapy alone included both locoregional and distant failures.
-
Although patients with unresectable stage IIIA disease may benefit from radiation therapy, long-term outcomes have generally been poor because of local and systemic relapse.
For patients requiring palliative treatment
Radiation therapy may be effective in palliating symptomatic local involvement with NSCLC, such as the following:
-
Tracheal, esophageal, or bronchial compression.
-
Pain.
-
Vocal cord paralysis.
-
Hemoptysis.
-
Superior vena cava syndrome.
In some cases, endobronchial laser therapy and/or brachytherapy has been used to alleviate proximal obstructing lesions.[25]
Evidence (radiation therapy for palliative treatment):
-
A systematic review identified six randomized trials of high-dose rate endobronchial brachytherapy (HDREB) alone or with external-beam radiation therapy (EBRT) or laser therapy.[26]
-
Better overall symptom palliation and fewer re-treatments were required in previously untreated patients using EBRT alone.[26][Level of evidence: 1iiC]
-
Although EBRT is frequently prescribed for symptom palliation, there is no consensus about when the fractionation scheme should be used.
-
For EBRT, different multifraction regimens appear to provide similar symptom relief;[27–32] however, single-fraction radiation therapy may be insufficient for symptom relief compared with hypofractionated or standard regimens, as seen in the NCIC Clinical Trials Group trial (NCT00003685).[29][Level of evidence: 1iiC]
-
Evidence of a modest increase in survival in patients with better PS given high-dose EBRT is available.[27,28][Level of evidence: 1iiA]
-
HDREB provided palliation of symptomatic patients with recurrent endobronchial obstruction previously treated by EBRT, when it was technically feasible.
-
Chemoradiation therapy
The addition of sequential and concurrent chemotherapy to radiation therapy has been evaluated in prospective randomized trials and meta-analyses. Overall, concurrent treatment may provide the greatest benefit in survival with an increase in toxic effects.
Concomitant platinum-based radiation chemotherapy may improve survival of patients with locally advanced NSCLC. However, the available data are insufficient to accurately define the size of such a potential treatment benefit and the optimal schedule of chemotherapy.[33]
Evidence (chemoradiation therapy):
-
A meta-analysis of patient data from 11 randomized clinical trials showed the following:[34]
-
Cisplatin-based combinations plus radiation therapy resulted in a 10% reduction in the risk of death compared with radiation therapy alone.[34][Level of evidence: 1iiA]
-
-
A meta-analysis of 13 trials (based on 2,214 evaluable patients) showed the following:[35]
-
The addition of concurrent chemotherapy to radical radiation therapy reduced the risk of death at 2 years (relative risk [RR], 0.93; 95% CI, 0.88–0.98; P = .01).
-
For the 11 trials with platinum-based chemotherapy, RR was 0.93 (95% CI, 0.87–0.99; P = .02).[35]
-
-
A meta-analysis of individual data from 1,764 patients was based on nine trials and showed the following:[33]
-
The HRdeath among patients treated with radiation therapy and chemotherapy compared with radiation therapy alone was 0.89 (95% CI, 0.81–0.98; P = .02), corresponding to an absolute benefit of chemotherapy of 4% at 2 years.
-
The combination of platinum with etoposide appeared to be more effective than platinum alone.
-
Concurrent versus sequential chemoradiation therapy
The results from two randomized trials (including RTOG-9410 [NCT01134861]) and a meta-analysis indicate that concurrent chemotherapy and radiation therapy may provide greater survival benefit, albeit with more toxic effects, than sequential chemotherapy and radiation therapy.[36–38][Level of evidence: 1iiA]
Evidence (concurrent vs. sequential chemoradiation therapy):
-
In the first trial, the combination of mitomycin C, vindesine, and cisplatin were given concurrently with split-course daily radiation therapy to 56 Gy compared with chemotherapy followed by continuous daily radiation therapy to 56 Gy.[36]
-
Five-year OS favored concurrent therapy (27% vs. 9%).
-
Myelosuppression was greater among patients in the concurrent arm, but treatment-related mortality was less than 1% in both arms.[36]
-
-
In the second trial, 610 patients were randomly assigned to sequential chemotherapy with cisplatin and vinblastine followed by 60 Gy of radiation therapy, concurrent chemotherapy, or concurrent chemotherapy with cisplatin and vinblastine with twice-daily radiation therapy.[38]
-
Median and 5-year survival were superior in the concurrent chemotherapy with daily radiation therapy arm (17 months vs. 14.6 months and 16% vs. 10% for sequential regimen [P = .046]).[38]
-
-
Two smaller studies also reported OS results that favored concurrent over sequential chemotherapy and radiation, although the results did not reach statistical significance.[37,39][Level of evidence: 1iiA]
-
A meta-analysis of three trials evaluated concurrent versus sequential treatment (711 patients).[35]
-
The analysis indicated a significant benefit of concurrent over sequential treatment (RR, 0.86; 95% CI, 0.78–0.95; P = .003). All studies used cisplatin-based regimens and once-daily radiation therapy.[35]
-
More deaths (3% OS rate) were reported in the concurrent arm, but this did not reach statistical significance (RR, 1.60; CI, 0.75–3.44; P = .2).
-
There was more acute esophagitis (grade 3 or worse) with concurrent treatment (range, 17%–26%) compared with sequential treatment (range, 0%–4%; RR, 6.77; P = .001). Overall, the incidence of neutropenia (grade 3 or worse) was similar in both arms.
-
Radiation therapy dose escalation for concurrent chemoradiation
With improvement in radiation therapy–delivery technology in the 1990s, including tumor-motion management and image guidance, phase I/II trials demonstrated the feasibility of dose-escalation radiation therapy to 74 Gy with concurrent chemotherapy.[40–42] However, a phase III trial of a conventional dose of 60 Gy versus dose escalation to 74 Gy with concurrent weekly carboplatin/paclitaxel did not demonstrate improved local control or PFS, and OS was worse with dose escalation (HR, 1.38 [1.09–1.76]; P = .004). There was a nonsignificant increase in grade 5 events with dose escalation (10% vs. 2%) and higher incidence of grade 3 esophagitis (21% vs. 7%; P =.0003). Thus, there is no clear benefit in radiation dose escalation beyond 60 Gy for stage III NSCLC.[43][Level of evidence: 1iiA]
Choice of systemic therapy for concurrent chemoradiation
Evidence (systemic therapy for concurrent chemoradiation):
-
The randomized phase III PROCLAIM study [NCT00686959] enrolled 598 patients with newly diagnosed, stage IIIA/B, unresectable, nonsquamous NSCLC.[44] Patients were randomly assigned on a 1:1 ratio to either of two arms:
-
Arm A: Pemetrexed (500 mg/m2) and cisplatin (75 mg/m2) intravenously every 3 weeks for three cycles plus concurrent thoracic radiation therapy (60 to 66 Gy) followed by pemetrexed consolidation every 3 weeks for four cycles.
-
Arm B: Standard therapy with etoposide (50 mg/m2) and cisplatin (50 mg/m2) intravenously every 4 weeks for two cycles plus concurrent thoracic radiation therapy (60 to 66 Gy) followed by two cycles of consolidation platinum-based doublet chemotherapy.
The primary objective was OS. The study was designed as a superiority trial with 80% power to detect an OS HR of 0.74 with a type 1 error of .05. This study randomly assigned 598 patients (arm A, 301; arm B, 297) and treated 555 patients (arm A, 283; arm B, 272).
-
Enrollment was stopped early because of futility.
-
OS in arm A was not superior to arm B (HR, 0.98; 95% CI, 0.79–1.20; median, 26.8 vs. 25.0 months; P = .831).
-
Arm A had a significantly lower incidence of any drug-related grade 3 to 4 adverse events (64.0% vs. 76.8%; P = .001), including neutropenia (24.4% vs. 44.5%; P < .001), during the overall treatment period.
-
Additional systemic therapy before or after concurrent chemotherapy and radiation therapy
The addition of induction chemotherapy before concurrent chemotherapy and radiation therapy has not been shown to improve survival.[45][Level of evidence: 1iiA]
Consolidation Immunotherapy
Durvalumab
Durvalumab is a selective human IgG1 monoclonal antibody that blocks programmed death ligand 1 (PD-L1) binding to programmed death 1 (PD-1) and CD80, allowing T cells to recognize and kill tumor cells.[46]
Evidence (durvalumab):
-
The phase III PACIFIC trial (NCT02125461) enrolled 713 patients with stage III NSCLC whose disease had not progressed after two or more cycles of platinum-based chemoradiation therapy. Patients were randomly assigned in a 2:1 ratio to receive durvalumab (10 mg/kg intravenously) or placebo (every 2 weeks for up to 12 months).[46] The coprimary endpoints were PFS assessed by blinded independent central review and OS (unplanned for the interim analysis).
-
At the interim analysis, the coprimary endpoint of PFS was met. The median PFS was 16.8 months with durvalumab versus 5.6 months with placebo (HR, 0.52; 95% CI, 0.42–0.65; P< .001).[46][Level of evidence:1iiDiii] The 18-month PFS rate was 44.2% with durvalumab versus 27% with placebo.
-
PFS benefit was seen across all prespecified subgroups and was irrespective of PD-L1 expression before chemoradiation therapy or smoking status. Epidermal growth factor receptor (EGFR) mutations were observed in 6% of patients (29 treated with durvalumab vs. 14 treated with placebo). The unstratified HR for the EGFR-mutated subgroup was 0.76 (95% CI, 0.35–1.64).
-
Grade 3 or 4 adverse events occurred in 29.9% of patients treated with durvalumab and in 26.1% of patients treated with placebo. The most common adverse event of grade 3 or 4 was pneumonia in 4.4% of the patients receiving durvalumab and in 3.8% of the patients receiving placebo.
-
OS was not assessed at the interim analysis.
-
Other systemic consolidation therapies
Randomized trials of other consolidation systemic therapies, including docetaxel,[47] gefitinib,[48] and tecemotide (MUC1 antigen-specific immunotherapy) [49] have not shown an improvement in OS.[Level of evidence: 1iiA]
Standard Treatment Options for Superior Sulcus Tumors (T3, N0 or N1, M0)
Standard treatment options for superior sulcus tumors include the following:
NSCLC of the superior sulcus, frequently termed Pancoast tumors, occurs in less than 5% of patients.[50,51] Superior sulcus tumors usually arise from the apex of the lung and are challenging to treat because of their proximity to structures at the thoracic inlet. At this location, tumors may invade the parietal pleura, chest wall, brachial plexus, subclavian vessels, stellate ganglion, and adjacent vertebral bodies. However, Pancoast tumors are amenable to curative treatment, especially in patients with T3, N0 disease.
Adverse prognostic factors include the presence of mediastinal nodal metastases (N2 disease), spine or subclavian-vessel involvement (T4 disease), and limited resection (R1 or R2).
Radiation therapy alone
While radiation therapy is an integral part of the treatment of Pancoast tumors, variations in dose, treatment technique, and staging that were used in various published series make it difficult to determine its effectiveness.[50,51]
Prognosis:
Small, retrospective series of radiation therapy in patients who were only clinically staged have reported 5-year survival rates of 0% to 40%, depending on T stage, total radiation dose, and other prognostic factors. Induction radiation therapy and en-bloc resection was shown to be potentially curative.
Evidence (radiation therapy):
Surgery
Evidence (surgery):
-
Retrospective case series have reported that complete resection was achieved in only 64% of T3, N0 tumors and 39% of T4, N0 tumors.[52]
Chemoradiation therapy followed by surgery
Evidence (chemoradiation therapy):
-
Two large, prospective, multicenter phase II trials have evaluated induction chemoradiation therapy followed by resection.[53,54]
-
In the first trial (NCT00002642), 110 eligible patients were enrolled with mediastinoscopy negative, clinical T3–4, N0–1 tumors of the superior sulcus.[54] Induction treatment was two cycles of etoposide and cisplatin with 45 Gy of concurrent radiation therapy.
-
The induction regimen was well tolerated, and only five participants had grade 3 or higher toxic effects.
-
Induction chemoradiation therapy could sterilize the primary lesion. Induction therapy was completed by 104 patients (95%). Of the 95 patients eligible for surgery, 88 (80%) underwent thoracotomy, two (1.8%) died postoperatively, and 83 (76%) had complete resections.
-
Pathologic complete response or minimal microscopic disease was seen in 61 (56%) resection specimens. Pathologic complete response led to better survival than when any residual disease was present (P = .02).
-
Five-year survival was 44% for all patients and 54% after complete resection, with no difference between T3 and T4 tumors. Disease progression occurred mainly in distant sites.
-
-
In the second trial, 75 patients were enrolled and treated with induction therapy with mitomycin C, vindesine, and cisplatin combined with 45 Gy of radiation therapy.[53] Fifty-seven patients (76%) underwent surgical resection, and complete resection was achieved in 51 patients (68%).
-
There were 12 patients with pathologic complete response.
-
Major postoperative morbidity, including chylothorax, empyema, pneumonitis, adult respiratory distress syndrome, and bleeding, was observed in eight patients. There were three treatment-related deaths.
-
At 3 years, the DFS rate was 49%, and the OS rate was 61%; at 5 years, the DFS rate was 45%, and the OS rate was 56%.[53][Level of evidence: 3iiiDi]
-
-
Radiation therapy dose escalation for concurrent chemoradiation
With improvement in radiation therapy–delivery technology in the 1990s, including tumor-motion management and image guidance, phase I/II trials demonstrated the feasibility of dose-escalation radiation therapy to 74 Gy with concurrent chemotherapy.[40–42] However, a phase III trial of a conventional dose of 60 Gy versus dose escalation to 74 Gy with concurrent weekly carboplatin/paclitaxel did not demonstrate improved local control or PFS, and OS was worse with dose escalation (HR, 1.38 [1.09–1.76]; P = .004). There was a nonsignificant increase in grade 5 events with dose escalation (10% vs. 2%) and higher incidence of grade 3 esophagitis (21% vs. 7%; P = .0003). Thus, there is no clear benefit in radiation dose escalation beyond 60 Gy for stage III NSCLC.[43][Level of evidence: 1iiA]
Choice of systemic therapy for concurrent chemoradiation
Evidence (systemic therapy for concurrent chemoradiation):
-
The randomized phase III PROCLAIM study [NCT00686959] enrolled 598 patients with newly diagnosed stage IIIA/B unresectable nonsquamous NSCLC.[44] Patients were randomly assigned in a 1:1 ratio to either of two arms:
-
Arm A: Pemetrexed (500 mg/m2) and cisplatin (75 mg/m2) intravenously every 3 weeks for three cycles plus concurrent thoracic radiation therapy (60 to 66 Gy) followed by pemetrexed consolidation every 3 weeks for four cycles.
-
Arm B: Standard therapy with etoposide (50 mg/m2) and cisplatin (50 mg/m2) intravenously every 4 weeks for two cycles plus concurrent thoracic radiation therapy (60 to 66 Gy) followed by two cycles of consolidation platinum-based doublet chemotherapy.
The primary objective was OS. The study was designed as a superiority trial with 80% power to detect an OS HR of 0.74 with a type 1 error of .05. This study randomly assigned 598 patients (arm A, 301; arm B, 297) and treated 555 patients (arm A, 283; arm B, 272).
-
Enrollment was stopped early because of futility.
-
OS in arm A was not superior to arm B (HR, 0.98; 95% CI, 0.79–1.20; median, 26.8 vs. 25.0 months; P = .831).
-
Arm A had a significantly lower incidence of any drug-related grade 3 to 4 adverse events (64.0% vs. 76.8%; P = .001), including neutropenia (24.4% vs. 44.5%; P < .001), during the overall treatment period.
-
Additional systemic therapy before or after concurrent chemotherapy and radiation therapy
The addition of induction chemotherapy before concurrent chemotherapy and radiation therapy has not been shown to improve survival.[45][Level of evidence: 1iiA]
The role of consolidation systemic therapy after concurrent chemotherapy and radiation therapy for unresectable NSCLC remains unclear. Randomized trials of consolidation systemic therapy including docetaxel,[47] gefitinib,[48] and tecemotide (MUC1 antigen-specific immunotherapy) [49] have not shown an improvement in OS.[Level of evidence: 1iiA]
Standard Treatment Options for Tumors That Invade the Chest Wall (T3, N0 or N1, M0)
Standard treatment options for tumors that invade the chest wall include the following:
-
Surgery.
-
Surgery and radiation therapy.
-
Radiation therapy alone.
-
Chemotherapy combined with radiation therapy and/or surgery.
Selected patients with bulky primary tumors that directly invade the chest wall can obtain long-term survival with surgical management provided that their tumor is completely resected.
Evidence (radical surgery):
-
In a small case series of 97 patients, the 5-year survival rate of patients who had completely resected T3, N0, M0 disease was 44.2%. For patients with completely resected T3, N1, M0 disease, the 5-year survival rate was 40.0%. In patients with completely resected T3, N2, M0 disease, the 5-year survival rate was 6.2%.[55][Level of evidence: 3iiiDi]
-
In a small case series of 104 patients, the 5-year survival rate of patients who had completely resected T3, N0, M0 disease was 67.3%. For patients with completely resected T3, N1, M0 disease, the 5-year survival rate was 100.0%. In patients with completely resected T3, N2, M0 disease, the 5-year survival rate was 17.9%.[56][Level of evidence: 3iiiDi]
-
In a case series of 309 patients treated at three centers, patients who underwent en bloc resection had superior outcomes compared with patients who underwent extrapleural resections (60.3% vs. 39.1%; P = .03).[57][Level of evidence: 3iiiDi]
Adjuvant chemotherapy is recommended and radiation therapy is reserved for cases with unclear resection margins. Survival rates were lower in patients who underwent incomplete resection and had mediastinal lymph node involvement. Combined-modality approaches have been evaluated to improve ability to achieve complete resection.
Treatment Options Under Clinical Evaluation
Treatment options under clinical evaluation include the following:
-
Combined modality therapy, including chemotherapy, radiation therapy, and surgery in various combinations.
Current Clinical Trials
Use our advanced clinical trial search to find NCI-supported cancer clinical trials that are now enrolling patients. The search can be narrowed by location of the trial, type of treatment, name of the drug, and other criteria. General information about clinical trials is also available.
Stages IIIB and IIIC NSCLC Treatment
On the basis of the Surveillance, Epidemiology, and End Results (SEER) program registry, the estimated incidence of stage IIIB non-small cell lung cancer (NSCLC) is 17.6%.[1] The anticipated 5-year survival for the vast majority of patients who present with clinical stage IIIB NSCLC is 3% to 7%.[2] In small case series, selected patients with T4, N0-1 disease, solely as the result of satellite tumor nodule(s) within the primary lobe, have been reported to have 5-year survival rates of 20%.[3,4][Level of evidence: 3iiiA]
Standard Treatment Options for Stages IIIB and IIIC NSCLC
Standard treatment options for stages IIIB NSCLC and IIIC NSCLC include the following:
In general, patients with stages IIIB and IIIC NSCLC do not benefit from surgery alone and are best managed by initial chemotherapy, chemotherapy plus radiation therapy, or radiation therapy alone, depending on the following:
-
Sites of tumor involvement.
-
The patient’s performance status (PS).
Most patients with excellent PS are candidates for combined-modality chemotherapy and radiation therapy with the following exceptions:
-
Selected patients with T4, N0 disease may be treated with combined-modality therapy and surgery similar to patients with superior sulcus tumors.
Sequential or concurrent chemotherapy and radiation therapy
Many randomized studies of patients with unresectable stage III NSCLC show that treatment with preoperative or concurrent cisplatin-based chemotherapy and radiation therapy to the chest is associated with improved survival compared with treatment that uses radiation therapy alone. Although patients with unresectable stages IIIB or IIIC disease may benefit from radiation therapy, long-term outcomes have generally been poor, often the result of local and systemic relapse. The addition of sequential and concurrent chemotherapy to radiation therapy has been evaluated in prospective randomized trials.
Evidence (sequential or concurrent chemotherapy and radiation therapy):
-
A meta-analysis of patient data from 11 randomized clinical trials showed the following:[5]
-
Cisplatin-based combinations plus radiation therapy resulted in a 10% reduction in the risk of death compared with radiation therapy alone.[5][Level of evidence: 1iiA]
-
-
A meta-analysis of 13 trials (based on 2,214 evaluable patients) showed the following:[6]
-
The addition of concurrent chemotherapy to radical radiation therapy reduced the risk of death at 2 years (relative risk [RR], 0.93; 95% confidence interval [CI], 0.88–0.98; P = .01).
-
For the 11 trials with platinum-based chemotherapy, RR was 0.93 (95% CI, 0.87–0.99; P = .02).[6]
-
-
A meta-analysis of individual data from 1,764 patients evaluated nine trials.[7]
-
The hazard ratio (HR)death among patients treated with radiation therapy and chemotherapy compared with radiation therapy alone was 0.89 (95% CI, 0.81–0.98; P = .02) corresponding to an absolute benefit of chemotherapy of 4% at 2 years.
-
The combination of platinum with etoposide appeared to be more effective than platinum alone. Concomitant platinum-based chemotherapy and radiation therapy may improve survival of patients with locally advanced NSCLC. However, the available data are insufficient to accurately define the size of such a potential treatment benefit and the optimal schedule of chemotherapy.[7]
-
-
The results from two randomized trials (including RTOG-9410 [NCT01134861]) and a meta-analysis indicate that concurrent chemotherapy and radiation therapy provide greater survival benefit, albeit with more toxic effects, than sequential chemotherapy and radiation therapy.[8–10][Level of evidence: 1iiA]
-
In the first trial, the combination of mitomycin C, vindesine, and cisplatin were given concurrently with split-course daily radiation therapy to 56 Gy compared with chemotherapy followed by continuous daily radiation therapy to 56 Gy.[8]
-
Five-year overall survival (OS) favored concurrent therapy (27% vs. 9%).
-
Myelosuppression was greater among patients in the concurrent arm, but treatment-related mortality was less than 1% in both arms.[8]
-
-
In the second trial, 610 patients were randomly assigned to sequential chemotherapy with cisplatin and vinblastine followed by 60 Gy of radiation therapy, concurrent chemotherapy, or concurrent chemotherapy with cisplatin and vinblastine with twice-daily radiation therapy.[9,10]
-
Median and 5-year survival were superior in the concurrent chemotherapy with daily radiation therapy arm (17 months vs. 14.6 months and 16% vs. 10% for sequential regimen [P = .046]).
-
-
Two smaller studies also reported OS results that favored concurrent over sequential chemotherapy and radiation, although the results did not reach statistical significance.[10][Level of evidence: 1iiA]; [11]
-
-
A meta-analysis of three trials evaluated concurrent versus sequential treatment (711 patients).[6]
-
The analysis indicated a significant benefit of concurrent versus sequential treatment (RR, 0.86; 95% CI, 0.78–0.95; P = .003). All used cisplatin-based regimens and once-daily radiation therapy.[6]
-
More deaths (3% overall) were reported in the concurrent arm, but this did not reach statistical significance (RR, 1.60; CI, 0.75–3.44; P = .2).
-
There was more acute esophagitis (grade 3 or worse) with concurrent treatment (range, 17%–26%) compared with sequential treatment (range, 0%–4%; RR, 6.77; P = .001). Overall, the incidence of neutropenia (grade 3 or worse) was similar in both arms.
-
Radiation therapy dose escalation for concurrent chemoradiation
With improvement in radiation therapy–delivery technology in the 1990s, including tumor-motion management and image guidance, phase I/II trials demonstrated the feasibility of dose-escalation radiation therapy to 74 Gy with concurrent chemotherapy.[12–14] However, a phase III trial of a conventional dose of 60 Gy versus dose escalation to 74 Gy with concurrent weekly carboplatin/paclitaxel did not demonstrate improved local control or progression-free survival (PFS), and OS was worse with dose escalation (HR, 1.38 [1.09–1.76]; P = .004). There was a nonsignificant increase in grade 5 events with dose escalation (10% vs. 2%) and higher incidence of grade 3 esophagitis (21% vs. 7%; P = .0003).[15][Level of evidence: 1iiA]
Additional systemic therapy before or after concurrent chemotherapy and radiation therapy
The addition of induction chemotherapy before concurrent chemotherapy and radiation therapy has not been shown to improve survival.[16][Level of evidence: 1iiA]
Consolidation Immunotherapy
Durvalumab
Durvalumab is a selective human IgG1 monoclonal antibody that blocks programmed death ligand 1 (PD-L1) binding to programmed death 1 (PD-1) and CD80, allowing T cells to recognize and kill tumor cells.[17]
Evidence (durvalumab):
-
The phase III PACIFIC trial (NCT02125461) enrolled 713 patients with stage III NSCLC whose disease had not progressed after two or more cycles of platinum-based chemoradiation therapy. Patients were randomly assigned in a 2:1 ratio to receive durvalumab (10 mg/kg intravenously) or placebo (every 2 weeks for up to 12 months).[17] The coprimary endpoints were PFS assessed by blinded independent central review and OS (unplanned for the interim analysis).
-
At the interim analysis, the coprimary endpoint of PFS was met. The median PFS was 16.8 months with durvalumab versus 5.6 months with placebo (HR, 0.52; 95% CI, 0.42–0.65; P < .001).[17][Level of evidence:1iiDiii] The 18-month PFS rate was 44.2% with durvalumab versus 27% with placebo.
-
PFS benefit was seen across all prespecified subgroups and was irrespective of PD-L1 expression before chemoradiation therapy or smoking status. Epidermal growth factor receptor (EGFR) mutations were observed in 6% of patients (29 treated with durvalumab vs. 14 treated with placebo). The unstratified HR for the EGFR-mutated subgroup was 0.76 (95% CI, 0.35–1.64).
-
Grade 3 or 4 adverse events occurred in 29.9% of patients treated with durvalumab and in 26.1% of patients treated with placebo. The most common adverse event of grade 3 or 4 was pneumonia in 4.4% of patients treated with durvalumab and in 3.8% of patients treated with placebo.
-
OS was not assessed at the interim analysis.
-
Other systemic consolidation therapies
Randomized trials of other consolidation systemic therapies, including docetaxel,[18] gefitinib,[19] and tecemotide (MUC1 antigen-specific immunotherapy) [20] have not shown an improvement in OS.[Level of evidence: 1iiA]
The role of consolidation systemic therapy after concurrent chemotherapy and radiation therapy for unresectable NSCLC remains unclear. Phase III trials of consolidation systemic therapy including conventional chemotherapy (docetaxel),[18] tyrosine kinase inhibitors (gefitinib),[19] and immunotherapy (tecemotide: MUC1 antigen-specific immunotherapy) [20] have not shown an improvement in OS.[Level of evidence: 1iiA]
Radiation therapy alone
For treatment of locally advanced unresectable tumor in patients who are not candidates for chemotherapy
Radiation therapy alone, administered sequentially or concurrently with chemotherapy, may provide benefit to patients with locally advanced unresectable stage III NSCLC. However, combination chemoradiation therapy delivered concurrently provides the greatest benefit in survival with an increase in toxic effects.
Prognosis:
Radiation therapy with traditional dose and fractionation schedules (1.8–2.0 Gy per fraction per day to 60–70 Gy in 6–7 weeks) results in reproducible long-term survival benefit in 5% to 10% of patients and significant palliation of symptoms.[21]
Evidence (radiation therapy for locally advanced unresectable tumor):
-
One prospective randomized clinical study showed the following:
-
Radiation therapy given as three daily fractions improved OS compared with radiation therapy given as one daily fraction.[22][Level of evidence: 1iiA]
-
Patterns of failure for patients treated with radiation therapy alone included both locoregional and distant failures.
-
For patients requiring palliative treatment
Radiation therapy may be effective in palliating symptomatic local involvement with NSCLC, such as the following:
-
Tracheal, esophageal, or bronchial compression.
-
Pain.
-
Vocal cord paralysis.
-
Hemoptysis.
-
Superior vena cava syndrome.
In some cases, endobronchial laser therapy and/or brachytherapy has been used to alleviate proximal obstructing lesions.[23]
Evidence (radiation therapy for palliative treatment):
-
A systematic review identified six randomized trials of high-dose rate endobronchial brachytherapy (HDREB) alone or with external-beam radiation therapy (EBRT) or laser therapy.[24]
-
Better overall symptom palliation and fewer re-treatments were required in previously untreated patients using EBRT alone.[24][Level of evidence: 1iiC]
-
HDREB provided palliation of symptomatic patients with recurrent endobronchial obstruction previously treated by EBRT, when it was technically feasible.
-
Although EBRT is frequently prescribed for symptom palliation, there is no consensus about when the fractionation scheme should be used.
-
Although different multifraction regimens appear to provide similar symptom relief,[25–30] single-fraction radiation may be insufficient for symptom relief compared with hypofractionated or standard regimens, as shown in the National Cancer Institute of Canada Clinical Trials Group trial (NCT00003685).[27][Level of evidence: 1iiC]
-
Evidence of a modest increase in survival in patients with better PS given high-dose radiation therapy is available.[25,26][Level of evidence: 1iiA]
-
Patients with stages IIIB or IIIC disease with poor PS are candidates for chest radiation therapy to palliate pulmonary symptoms (e.g., cough, shortness of breath, hemoptysis, or pain).[21][Level of evidence: 3iiiC] (Refer to the PDQ summaries on Cardiopulmonary Syndromes and Cancer Pain for more information.)
Treatment Options Under Clinical Evaluation
Because of the poor overall results, patients with stages IIIB or IIIC NSCLC are candidates for clinical trials, which may lead to improvement in the control of disease.
Treatment options under clinical evaluation include the following:
-
New fractionation schedules.
-
Radiosensitizers (NCT02186847).
-
Combined-modality approaches.
-
Incorporation of targeted agents into combined modality therapy in patients with EGFR-mutant or ALK-translocated tumors (RTOG-1306 [NCT01822496]; 11-464 [NCT01553942]).
-
Adaptive radiation therapy using positron emission tomography–based response assessment during treatment (RTOG-1106/ACRIN-6697 ).
Current Clinical Trials
Use our advanced clinical trial search to find NCI-supported cancer clinical trials that are now enrolling patients. The search can be narrowed by location of the trial, type of treatment, name of the drug, and other criteria. General information about clinical trials is also available.
Newly Diagnosed Stage IV, Relapsed, and Recurrent NSCLC Treatment
Forty percent of patients with newly diagnosed non-small cell lung cancer (NSCLC) have stage IV disease. Treatment goals are to prolong survival and control disease-related symptoms. Treatment options include cytotoxic chemotherapy, targeted agents, and immunotherapy. Factors influencing treatment selection include comorbidity, performance status (PS), histology, and molecular and immunologic features of the cancer. Therefore, assessment of tumor-genomic changes and programmed death-ligand 1 (PD-L1) expression is critical before initiating therapy. Radiation therapy and surgery are generally used in selective cases for symptom palliation.
Determinants of treatment
Randomized controlled trials of patients with stage IV disease and good PS have shown that cisplatin-based chemotherapy improves survival and palliates disease-related symptoms.[1][Level of evidence: 1iiA] Patients with nonsquamous cell histology, good PS, no history of hemoptysis or other bleeding, or recent history of cardiovascular events may benefit from the addition of bevacizumab to paclitaxel and carboplatin. Patients with tumors harboring sensitizing mutations in exons 19 or 21 of EGFR, particularly those from East Asia, never smokers, and those with adenocarcinoma may benefit from EGFR tyrosine kinase inhibitors (TKI) as an alternative to first- or second-line chemotherapy. Patients with tumors harboring anaplastic lymphoma kinase (ALK) translocations or ROS1rearrangements may benefit from ALK or ROS1 inhibitors as an alternative to first- or second-line chemotherapy. Patients with tumors expressing PD-L1 (>50% by immunohistochemistry) have improved survival with pembrolizumab. The addition of pembrolizumab to carboplatin plus pemetrexed chemotherapy for nonsquamous advanced lung cancer improves survival irrespective of PD-L1 expression.[2][Level of evidence: 1iiA] Second-line systemic therapy with nivolumab, docetaxel, pemetrexed, or pembrolizumab for PD-L1-positive tumors also improves survival in patients with good PS (who have not received the same or a similar agent in the first-line setting).[1][Level of evidence: 1iiA]
The role of systemic therapy in patients with an Eastern Cooperative Oncology Group PS below 2 is less certain.
Histology
Patients with adenocarcinoma may benefit from pemetrexed [3] and bevacizumab as well as from combination chemotherapy with pembrolizumab.
Age versus comorbidity
Evidence supports the concept that elderly patients with good PS and limited comorbidity may benefit from combination chemotherapy. Age alone should not dictate treatment-related decisions in patients with advanced NSCLC. Elderly patients with a good PS enjoy longer survival and a better quality of life when treated with chemotherapy compared with supportive care alone. Caution should be exercised when extrapolating data for elderly patients (aged 70–79 years) to patients aged 80 years or older because only a very small number of patients aged 80 years or older have been enrolled on clinical trials, and the benefit in this group is uncertain.[4,5]
Evidence (age vs. comorbidity):
-
Platinum-containing combination chemotherapy regimens provide clinical benefit when compared with supportive care or single-agent therapy; however, such treatment may be contraindicated in some older patients because of the age-related reduction in the functional reserve of many organs and/or comorbid conditions. Approximately two-thirds of patients with NSCLC are aged 65 years or older, and approximately 40% are aged 70 years or older.[6] Surveillance, Epidemiology, and End Results (SEER) data suggest that the percentage of patients aged older than 70 years is closer to 50%.
-
A review of the SEER Medicare data from 1994 to 1999 found a much lower rate of chemotherapy use than expected for the overall population.[7] The same data suggested that elderly patients may have more comorbidities or a higher rate of functional compromise that would make study participation difficult, if not contraindicated; lack of clinical trial data may influence decisions to treat individual patients with standard chemotherapy.
-
Single-agent chemotherapy and combination chemotherapy clearly benefit at least some elderly patients. In the Elderly Lung Cancer Vinorelbine Italian Study, 154 patients who were older than 70 years were randomly assigned to vinorelbine or supportive care.[8]
-
Patients who were treated with vinorelbine had a 1-year survival rate of 32%, compared with 14% for those who were treated with supportive care alone. Quality-of-life parameters were also significantly improved in the chemotherapy arm, and toxic effects were acceptable.
-
-
A trial from Japan compared single-agent docetaxel with vinorelbine in 180 elderly patients with good PS.[9]
-
Response rates (22% vs. 10%) and progression-free survival (PFS) rates (5.4 months vs. 3.1 months) were significantly better with docetaxel, but median survival rates (14.3 months vs. 9.9 months) and 1-year survival rates (59% vs. 37%) did not reach statistical significance.
-
-
Retrospective data analyzing and comparing younger (age <70 years) patients with older (age ≥70 years) patients who participated in large randomized trials of doublet combinations have also shown that elderly patients may derive the same survival benefit, but with a higher risk of toxic effects in the bone marrow.[4,5,10–13]
Performance status
PS is among the most important prognostic factors for survival of patients with NSCLC.[14] The benefit of therapy for this group of patients has been evaluated through retrospective analyses and prospective clinical trials.
The results support further evaluation of chemotherapeutic approaches for both metastatic and locally advanced NSCLC; however, the efficacy of current platinum-based chemotherapy combinations is such that no specific regimen can be regarded as standard therapy. Outside of a clinical trial setting, chemotherapy should be given only to patients with good PS and evaluable tumor lesions, who desire this treatment after being fully informed of its anticipated risks and limited benefits.
Evidence (PS):
-
The Cancer and Leukemia Group B trial (CLB-9730 [NCT00003117]), which compared carboplatin and paclitaxel with single-agent paclitaxel, enrolled 99 patients with a PS of 2 (18% of the study’s population).[12]
-
When compared with patients with a PS of 0 to 1, who had a median survival of 8.8 months and a 1-year survival rate of 38%, the corresponding median survival figures for patients with a PS of 2 were 3.0 months and a 1-year survival rate of 14%; this demonstrates the poor prognosis conferred by a lower PS. These differences were statistically significant.
-
When patients with a PS of 2 were analyzed by treatment arm, those who received combination chemotherapy had a significantly higher response rate (24% vs. 10%), longer median survival (4.7 months vs. 2.4 months), and a superior 1-year survival rate (18% vs. 10%), compared with those who were treated with single-agent paclitaxel.[12]
-
-
A phase III trial compared single-agent pemetrexed with the combination of carboplatin and pemetrexed in 205 patients with a PS of 2 who had not had any previous chemotherapy.[15][Level of evidence: 1iiA]
-
Median overall survival (OS) was 5.3 months for the pemetrexed-alone group and 9.3 months for the carboplatin-and-pemetrexed group (hazard ratio [HR], 0.62; 95% confidence interval [CI], 0.46–0.83; P= .001).
-
Median PFS was 2.8 months for the pemetrexed-alone group and 5.8 months for the carboplatin-and-pemetrexed group (P < .001).
-
The response rates were 10.3% for the pemetrexed-alone group and 23.8% for the carboplatin-and-pemetrexed group (P = .032).
-
Side effects were more frequent in the combination arm, as expected.
This study, which was performed in eight centers in Brazil and one center in the United States, reported rates of OS and PFS that were higher than has historically been noted in most, although not all, other published studies. This may indicate differences in patient selection. -
-
A subset analysis of 68 patients with a PS of 2 from a trial that randomly assigned more than 1,200 patients to four platinum-based regimens has been published.
-
Despite a high incidence of adverse events, including five deaths, the final analysis showed that the overall toxic effects experienced by patients with a PS of 2 was not significantly different from that experienced by patients with a PS of 0 to 1.
-
An efficacy analysis demonstrated an overall response rate of 14%, median survival time of 4.1 months, and a 1-year survival rate of 19%; all were substantially inferior to the patients with PS of 0 to 1.
-
-
A phase II randomized trial (E-1599 [NCT00006004]) of attenuated dosages of cisplatin plus gemcitabine and carboplatin plus paclitaxel included 102 patients with a PS of 2.[16]
-
Response rates were 25% in the cisplatin-plus-gemcitabine arm and 16% in the carboplatin-plus-paclitaxel arm; median survival times were 6.8 months in the cisplatin-plus-gemcitabine arm and 6.1 months in the carboplatin-plus-paclitaxel arm; 1-year survival rates were 25% in the cisplatin-plus-gemcitabine arm and 19% in the carboplatin-plus-paclitaxel arm. None of these differences was statistically significant, but the survival figures were longer than expected, based on historical controls.
-
Standard Treatment Options for Newly Diagnosed Stage IV, Relapsed, and Recurrent NSCLC (First-line Therapy)
Standard treatment options for patients with newly diagnosed stage IV, relapsed, and recurrent disease include the following:
-
Cytotoxic combination chemotherapy with platinum (cisplatin or carboplatin) and paclitaxel, gemcitabine, docetaxel, vinorelbine, irinotecan, protein-bound paclitaxel, and pemetrexed.
-
Maintenance therapy following first-line chemotherapy (for patients with stable or responding disease after four cycles of platinum-based combination chemotherapy).
-
Maintenance therapy following first-line chemotherapy.
-
Pemetrexed following first-line platinum-based combination chemotherapy.
-
Maintenance erlotinib following platinum-based doublet chemotherapy.
-
-
Epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKI) (for patients with EGFR mutations).
-
Osimertinib.
-
-
Anaplastic lymphoma kinase (ALK) inhibitors (for patients with ALK translocations).
-
Alectinib.
-
-
ROS1 inhibitors (for patients with ROS1 rearrangements).
-
Immune checkpoint inhibitors with or without chemotherapy.
-
Pembrolizumab plus chemotherapy.
-
-
Local therapies and special considerations.
-
Endobronchial laser therapy and/or brachytherapy (for obstructing lesions).[19]
-
External-beam radiation therapy (EBRT) (primarily for palliation of local symptomatic tumor growth).[20–22]
-
Cytotoxic combination chemotherapy
Combination chemotherapy
The type and number of chemotherapy drugs to be used for the treatment of patients with advanced NSCLC has been extensively evaluated in randomized controlled trials and meta-analyses.
Several randomized trials have evaluated various drugs combined with either cisplatin or carboplatin in previously untreated patients with advanced NSCLC. On the basis of meta-analyses of the trials, the following conclusions can be drawn:
-
Certain three-drug combinations that add so-called targeted agents may result in superior survival.
-
EGFR inhibitors may benefit selected patients with EGFR mutations.
-
Maintenance chemotherapy after four cycles of platinum combination chemotherapy may improve PFS and OS.
-
Platinum combinations with vinorelbine, paclitaxel, docetaxel, gemcitabine, irinotecan, protein-bound paclitaxel, and pemetrexed yield similar improvements in survival. Types and frequencies of toxic effects differ, and these may determine the preferred regimen for an individual patient. Patients with adenocarcinoma may benefit from pemetrexed.
-
Cisplatin and carboplatin yield similar improvements in outcome with different toxic effects. Some, but not all, trials and meta-analyses of trials suggest that outcomes with cisplatin may be superior, although with a higher risk of certain toxicities such as nausea and vomiting.
-
Nonplatinum combinations offer no advantage to platinum-based chemotherapy, and some studies demonstrate inferiority.
-
Three-drug combinations of the commonly used chemotherapy drugs do not result in superior survival and are more toxic than two-drug combinations.
Evidence (combination chemotherapy):
-
The Cochrane Collaboration reviewed data from all randomized controlled trials published between January 1980 and June 2006, comparing a doublet regimen with a single-agent regimen or comparing a triplet regimen with a doublet regimen in patients with advanced NSCLC.[23] Sixty-five trials (13,601 patients) were identified.
-
In the trials that compared a doublet regimen with a single-agent regimen, a significant increase was observed in tumor response (odds ratio [OR], 0.42; 95% CI, 0.37–0.47; P < .001) and 1-year survival (OR, 0.80; 95% CI, 0.70–0.91; P < .001) in favor of the doublet regimen. The absolute benefit in 1-year survival was 5%, which corresponds to an increase in 1-year survival from 30% with a single-agent regimen to 35% with a doublet regimen. The rates of grades 3 and 4 toxic effects caused by doublet regimens were statistically increased compared with rates after single-agent therapy, with ORs ranging from 1.2 to 6.2. Infection rates did not increase in doublet regimens.
-
There was no increase in 1-year survival (OR, 1.01; 95% CI, 0.85–1.21; P = .88) for triplet regimens versus doublet regimens. The median survival ratio was 1.00 (95% CI, 0.94–1.06; P = .97).
-
-
Several meta-analyses have evaluated whether cisplatin or carboplatin regimens are superior, with variable results.[24–26] One meta-analysis reported individual patient data for 2,968 patients entered in nine randomized trials.[24]
-
The objective response rate (ORR) was higher for patients treated with cisplatin (30%) than for patients treated with carboplatin (24%); (OR, 1.37; 95% CI, 1.16–1.61; P < .001).
-
Carboplatin treatment was associated with a nonstatistically significant increase in the hazard of mortality relative to treatment with cisplatin (HR, 1.07; 95% CI, 0.99–1.15; P = .100).
-
In patients with nonsquamous cell tumors and in patients treated with third-generation chemotherapy, carboplatin-based chemotherapy was associated with a statistically significant increase in mortality (HR, 1.12; 95% CI, 1.01–1.23 in patients with nonsquamous cell tumors and HR, 1.11; 95% CI, 1.01–1.21 in patients treated with third-generation chemotherapy).
-
Treatment-related toxic effects were also assessed in the meta-analysis. More thrombocytopenia was seen with carboplatin than with cisplatin (12% vs. 6%; OR, 2.27; 95% CI, 1.71–3.01; P < .001), but cisplatin caused more nausea and vomiting (8% vs. 18%; OR, 0.42; 95% CI, 0.33–0.53; P < .001) and renal toxic effects (0.5% vs. 1.5%; OR, 0.37; 95% CI, 0.15–0.88; P = .018).
-
The authors concluded that treatment with cisplatin was not associated with a substantial increase in the overall risk of severe toxic effects. This comprehensive individual-patient meta-analysis is consistent with the conclusions of other meta-analyses that were based on essentially the same clinical trials but which used only published data.
-
-
Three literature-based meta-analyses have trials that compared platinum with nonplatinum combinations.[27–29]
-
The first meta-analysis identified 37 assessable trials that included 7,633 patients.[27]
-
A 62% increase in the OR for response was attributable to platinum-based therapy (OR, 1.62; 95% CI, 1.46–1.8; P < .001). The 1-year survival rate was increased by 5% with platinum-based regimens (34% vs. 29%; OR, 1.21; 95% CI, 1.09–1.35; P = .003).
-
No statistically significant increase in 1-year survival was found when platinum therapies were compared with third-generation-based combination regimens (OR, 1.11; 95% CI, 0.96–1.28; P = .17).
-
The toxic effects of platinum-based regimens was significantly higher for hematologic toxic effects, nephrotoxic effects, and nausea and vomiting but not for neurologic toxic effects, febrile neutropenia rate, or toxic death rate. These results are consistent with the second literature-based meta-analysis.
-
-
The second meta-analysis identified 17 trials that included 4,920 patients.[28]
-
The use of platinum-based doublet regimens was associated with a slightly higher survival at 1 year (relative risk [RR], 1.08; 95% CI, 1.01%–1.16%; P = .03) and a better partial response (RR, 1.11; 95% CI, 1.02–1.21; P = .02), with a higher risk of anemia, nausea, and neurologic toxic effects.
-
In subanalyses, cisplatin-based doublet regimens improved survival at 1 year (RR, 1.16%; 95% CI, 1.06–1.27; P = .001), complete response (RR, 2.29; 95% CI, 1.08–4.88; P = .03), and partial response (RR, 1.19; 95% CI, 1.07–1.32; P = .002), with an increased risk of anemia, neutropenia, neurologic toxic effects, and nausea.
-
Conversely, carboplatin-based doublet regimens did not increase survival at 1 year (RR, 0.95; 95% CI, 0.85–1.07; P = .43).
-
-
The third meta-analysis of phase III trials randomizing platinum-based versus nonplatinum combinations as first-line chemotherapy identified 14 trials.[29] Experimental arms were gemcitabine and vinorelbine (n = 4), gemcitabine and taxane (n = 7), gemcitabine and epirubicin (n = 1), paclitaxel and vinorelbine (n = 1), and gemcitabine and ifosfamide (n = 1). This meta-analysis was limited to the set of 11 phase III studies that used a platinum-based doublet (2,298 patients in the platinum-based arm and 2,304 patients in the nonplatinum arm).
-
Patients treated with a platinum-based regimen benefited from a statistically significant reduction in the risk of death at 1 year (OR, 0.88; 95% CI, 0.78–0.99; P = .044) and a lower risk of being refractory to chemotherapy (OR, 0.87; CI, 0.73–0.99; P = .049).
-
Forty-four (1.9%) toxic-related deaths were reported for platinum-based regimens and 29 (1.3%) toxic-related deaths were reported for nonplatinum regimens (OR, 1.53; CI, 0.96–2.49; P = 0.08). An increased risk of grade 3 to 4 gastrointestinal and hematologic toxic effects for patients treated with platinum-based chemotherapy was statistically demonstrated. There was no statistically significant increase in the risk of febrile neutropenia (OR, 1.23; CI, 0.94–1.60; P = .063).
-
-
Drug and dose schedule
Among the active combinations, definitive recommendations regarding drug dose and schedule cannot be made, with the exception of carboplatin, pemetrexed, and pembrolizumab for patients with nonsquamous tumor histology.
Evidence (drug and dose schedule):
-
One meta-analysis of seven trials that included 2,867 patients assessed the benefit of docetaxel versus vinorelbine.[30] Docetaxel was administered with a platinum agent in three trials, with gemcitabine in two trials, or as monotherapy in two trials. Vinca alkaloid (vinorelbine in six trials and vindesine in one trial) was administered with cisplatin in six trials or alone in one trial.
-
The pooled estimate for OS showed an 11% improvement in favor of docetaxel (HR, 0.89; 95% CI, 0.82–0.96; P = .004). Sensitivity analyses that considered only vinorelbine as a comparator or only the doublet regimens showed similar improvements.
-
Grade 3 to 4 neutropenia and grade 3 to 4 serious adverse events were less frequent with docetaxel-based regimens (OR, 0.59; 95% CI, 0.38–0.89; P = .013) versus vinca alkaloid-based regimens (OR, 0.68; 95% CI, 0.55–0.84; P < .001).
-
-
Two randomized trials compared weekly versus every 3 weeks’ dosing of paclitaxel and carboplatin, which reported no significant difference in efficacy and better tolerability for weekly administration.[31,32] Although meta-analyses of randomized controlled trials suggest that cisplatin combinations may be superior to carboplatin or nonplatinum combinations, the clinical relevance of the differences in efficacy must be balanced against the anticipated tolerability, logistics of administration, and familiarity of the medical staff in making treatment decisions for individual patients.
-
A large, noninferiority, phase III randomized study compared the OS in 1,725 chemotherapy-naïve patients with stage IIIB/IV NSCLC and a PS of 0 to 1.[3] Patients received cisplatin 75 mg/m2 on day 1 and gemcitabine 1,250 mg/m2 on days 1 and 8 (n = 863) or cisplatin 75 mg/m2 and pemetrexed 500 mg/m2 on day 1 (n = 862) every 3 weeks for up to six cycles.
-
OS for cisplatin and pemetrexed (median survival, 10.3 months) was noninferior to cisplatin and gemcitabine (median survival, 10.3 months; HR, 0.94; 95% CI, 0.84%–1.05%).
-
In patients with adenocarcinoma (n = 847), OS was statistically superior for cisplatin and pemetrexed (12.6 months) versus cisplatin and gemcitabine (10.9 months); in patients with large cell carcinoma (n = 153), OS was statistically superior for cisplatin and pemetrexed (10.4 months) versus cisplatin and gemcitabine (6.7 months).
-
In contrast, in patients with squamous cell histology (n = 473), there was a significant improvement in survival with cisplatin and gemcitabine (10.8 months) versus cisplatin and pemetrexed (9.4 months). For cisplatin and pemetrexed, rates of grade 3 or 4 neutropenia, anemia, and thrombocytopenia (P ≤ .001); febrile neutropenia (P = .002); and alopecia (P < .001) were significantly lower, whereas grade 3 or 4 nausea (P = .004) was more common.
-
The results of this study suggested that the cisplatin and pemetrexed doublet is another alternative doublet for first-line chemotherapy for advanced NSCLC and also suggested that there may be differences in outcome depending on histology.
-
Combination chemotherapy with monoclonal antibodies
Bevacizumab
Evidence (bevacizumab):
-
Two randomized trials have evaluated the addition of bevacizumab, an antibody targeting vascular endothelial growth factor, to standard first-line combination chemotherapy.
-
In a randomized study of 878 patients with recurrent or advanced stage IIIB/IV NSCLC, 444 patients received paclitaxel and carboplatin alone, and 434 patients received paclitaxel and carboplatin plus bevacizumab.[33] Chemotherapy was administered every 3 weeks for six cycles, and bevacizumab was administered every 3 weeks until disease progression was evident or toxic effects were intolerable. Patients with squamous cell tumors, brain metastases, clinically significant hemoptysis, or inadequate organ function or PS (Eastern Cooperative Oncology Group PS >1) were excluded.
-
Median survival was 12.3 months in the group assigned to chemotherapy plus bevacizumab, as compared with 10.3 months in the chemotherapy-alone group (HRdeath, 0.79; P = .003).
-
Median PFS was 6.2 months in the group assigned to chemotherapy plus bevacizumab (HR for disease progression, 0.66; P < .001), with a 35% response rate (P < .001), and 4.5 months in the chemotherapy-alone group (HR for disease progression, 0.66; P < .001), with a 15% response rate (P < .001).
-
Rates of clinically significant bleeding were 4.4% in the group assigned to chemotherapy plus bevacizumab and 0.7% in the chemotherapy-alone group (P < .001). There were 15 treatment-related deaths in the chemotherapy-plus-bevacizumab group, including five from pulmonary hemorrhage.
-
For this subgroup of patients with NSCLC, the addition of bevacizumab to paclitaxel and carboplatin may provide survival benefit.[33][Level of evidence: 1iiA]
-
-
Another randomized, phase III trial investigated the efficacy and safety of cisplatin-gemcitabine plus bevacizumab.[34] Patients were randomly assigned to receive cisplatin (80 mg/m2) and gemcitabine (1,250 mg/m2) for up to six cycles, plus low-dose bevacizumab (7.5 mg/kg), high-dose bevacizumab (15 mg/kg), or placebo every 3 weeks until disease progression. The primary endpoint was amended from OS to PFS during the course of the study. A total of 1,043 patients were accrued (placebo group, n = 347; low-dose group, n = 345; high-dose group, n = 351).
-
PFS was significantly prolonged with the addition of bevacizumab; the HRs for PFS were 0.75 in the low-dose group (median PFS, 6.7 months vs. 6.1 months for placebo group; P = .03) and 0.82 in the high-dose group compared with the placebo group (median PFS, 6.5 months vs. 6.1 months for placebo group; P = .03).[34][Level of evidence: 1iiB]
-
ORRs were also improved with the addition of bevacizumab, and they were 20.1% for placebo, 34.1% for low-dose bevacizumab, and 30.4% for high-dose bevacizumab plus cisplatin/gemcitabine.
-
Incidence of grade 3 or greater adverse events was similar across arms.
-
Grade 3 or greater pulmonary hemorrhage rates were 1.5% or less for all arms, despite 9% of patients receiving therapeutic anticoagulation.
-
These results support the addition of bevacizumab to platinum-containing chemotherapy, but the results are far less impressive than when the carboplatin-paclitaxel combination was used.
-
Furthermore, no significant difference in survival was shown in this study, as reported in abstract form.
-
Altogether, these findings may suggest that the backbone of chemotherapy may be important when bevacizumab is added.
-
-
Cetuximab
Evidence (cetuximab):
-
Two trials have evaluated the addition of cetuximab to first-line combination chemotherapy.[35,36]
-
In the first trial, 676 chemotherapy-naïve patients with stage IIIB (pleural effusion) or stage IV NSCLC, without restrictions by histology or EGFR expression, received cetuximab with taxane (paclitaxel or docetaxel with carboplatin) or combination chemotherapy.[35]
-
The addition of cetuximab did not result in a statistically significant improvement in PFS, the primary study endpoint, or OS.
-
Median PFS was 4.40 months for patients in the cetuximab-chemotherapy arm versus 4.24 months for patients in the taxane-carboplatin arm (HR, 0.902; 95% CI, 0.761–1.069; P = .236).
-
Median OS was 9.69 months for patients in the cetuximab-chemotherapy arm versus 8.38 months for patients in the chemotherapy-alone arm (HR, 0.890; 95% CI, 0.754–1.051; P = .169).
-
No significant associations were found between EGFR expression, EGFR mutation, EGFR copy number, or KRAS mutations and PFS, OS, and response in the treatment-specific analyses.[37]
-
-
The second trial was composed of 1,125 chemotherapy-naïve patients with advanced EGFR-expressing stage IIIB/IV NSCLC treated with cisplatin-vinorelbine chemotherapy plus cetuximab or chemotherapy alone.[36]
-
The primary study endpoint, OS, was longer for patients treated with cetuximab and chemotherapy (median 11.3 months vs. 10.1 months; HRdeath, 0.871; 95% CI, 0.762–0.996; P = .044).
-
A survival benefit was seen in all histological subgroups; however, survival benefit was not seen in nonwhite or Asian patients. Only the interaction between the treatment and the ethnic origin was significant (P = .011).
-
The main cetuximab-related adverse event was acne-like rash (grade 3, 10%).
-
-
It is not clear whether the differences in outcome in these two studies are the result of differences in the study populations, tumor characterization for EGFR expression, or chemotherapy regimens.
-
Necitumumab
Evidence (necitumumab):
-
Two phase III trials have evaluated the addition of the second-generation, recombinant, human immunoglobulin G1 EGFR antibody, necitumumab, to platinum-doublet chemotherapy in the first-line treatment of patients with advanced nonsquamous cell and squamous cell NSCLC.[38,39]
-
The SQUIRE trial (NCT00981058) randomly assigned 1,093 patients with advanced squamous NSCLC to receive either first-line chemotherapy with cisplatin and gemcitabine or the same regimen with the addition of necitumumab (800 mg on day 1 and day 8 of each cycle).[39]
-
Median OS was prolonged with the addition of necitumumab (11.5 months vs. 9.9 months; P = .01).
-
PFS was also prolonged with the addition of necitumumab (5.7 months vs. 5.5 months); however, ORR was similar in both groups (31% vs. 28%).
-
Grades 3 and 4 adverse events were higher in the necitumumab-containing arm (72% vs. 62%).
-
Necitumumab is associated with higher toxicity and relatively modest benefit.
-
-
The INSPIRE trial (NCT00982111) randomly assigned 633 patients with advanced nonsquamous NSCLC to receive either first-line chemotherapy with cisplatin and pemetrexed or to cisplatin and pemetrexed with the addition of necitumumab (800 mg on day 1 and day 8 of each cycle).[38]
-
This study showed no benefit from the addition of necitumumab to standard first-line chemotherapy for advanced nonsquamous NSCLC.
-
OS was 11.3 months (95% CI, 9.5–13.4) for patients in the necitumumab-containing arm versus 11.5 months (95% CI, 10.1–13.1) for patients in the chemotherapy alone arm; P = .96. Similarly, there was no difference between the arms in terms of ORR or PFS.
-
Serious adverse events and rates of grades 3 and 4 adverse events, including thromboembolic events, were higher in patients in the necitumumab-containing arm; the incidence of treatment-related deaths was also higher (5% vs. 3%).
-
On the basis of these results, necitumumab is not recommended as combination therapy with standard first-line chemotherapy for patients with advanced nonsquamous NSCLC.
-
-
Maintenance therapy after first-line chemotherapy (for patients with stable or responding disease after four cycles of platinum-based combination chemotherapy)
One extensively investigated treatment strategy in NSCLC is maintenance therapy after initial response to chemotherapy. Options for maintenance therapy that have been investigated include the following:
-
Continuing the initial combination chemotherapy regimen.
-
Continuing only single-agent chemotherapy.
-
Introducing a new agent as maintenance.
Multiple randomized trials have evaluated the efficacy of continuing first-line combination cytotoxic chemotherapy beyond three to four cycles.
Evidence (maintenance therapy following first-line chemotherapy):
-
None of the trials of continued cytotoxic combinations showed a significant OS advantage with additional or longer durations beyond four cycles. For patients with nonsquamous NSCLC, two studies have demonstrated improved PFS and OS with either switch or continuous maintenance chemotherapy (e.g., maintenance pemetrexed after initial cisplatin and gemcitabine or maintenance pemetrexed after initial cisplatin and pemetrexed).[40]
These data suggest that PFS and OS for patients with nonsquamous NSCLC may be improved either by continuing an effective chemotherapy beyond four cycles or by immediate initiation of alternative chemotherapy. The improvement in PFS, however, is tempered by an increase in adverse events including additional cytotoxic chemotherapy and no consistent improvement in quality of life. For patients who have stable disease or who respond to first-line therapy, evidence does not support the continuation of combination cytotoxic chemotherapy until disease progression or the initiation of a different chemotherapy before disease progression. Collectively, these trials suggest that first-line cytotoxic combination chemotherapy should be stopped at disease progression or after four cycles in patients whose disease is not responding to treatment; it can be administered for no more than six cycles.[41,42,44,45] For patients with nonsquamous NSCLC who have a response or stable disease after four to six cycles of platinum combination chemotherapy, maintenance chemotherapy with pemetrexed should be considered.
[40]
EGFR tyrosine kinase inhibitors
Selective patients may benefit from single-agent EGFR TKIs. Randomized controlled trials of patients with chemotherapy-naïve NSCLC and EGFR mutations have shown that EGFR inhibitors improved PFS but not OS and have favorable toxicity profiles compared with combination chemotherapy.
Osimertinib
Evidence (osimertinib):
-
A phase III, multicenter, randomized, double-blind, controlled trial (FLAURA [NCT02296125]) compared osimertinib with standard of care EGFR TKIs (gefitinib or erlotinib) as first-line treatment of patients with previously untreated, EGFR mutation-positive (exon 19 deletion or L858R), advanced NSCLC, as detected by a U.S. Food and Drug Administration (FDA)-approved test.[51] The 556 patients were randomly assigned in a 1:1 ratio.
-
Investigator-assessed PFS, the primary endpoint, was significantly longer with osimertinib (18.9 months vs. 10.2 months; HR, 0.46; 95% CI, 0.37–0.57, P < .0001).[51][Level of evidence: 1iDiii]
-
The objective response rate was similar for both groups (80% for the osimertinib group vs. 76% for the standard EGFR TKI group).
-
The median duration of response was 17.2 months (95% CI, 13.8–22.0) with osimertinib versus 8.5 months (95% CI, 7.3–9.8) with standard EGFR TKIs.
-
Data on OS are immature.
-
Adverse events of grade 3 or higher were less frequent with osimertinib (34%) than with standard TKIs (45%).
-
Osimertinib was approved by the FDA for first-line treatment of EGFR-mutant NSCLC (exon 19 deletion or L858R).
Gefitinib
Evidence (gefinitib):
-
A phase III, multicenter, randomized trial compared gefitinib with carboplatin plus paclitaxel as first-line treatment in clinically selected patients in East Asia who had advanced adenocarcinoma of the lung and had never smoked or were former light smokers.[52]
-
The study met its primary objective of demonstrating the superiority of gefitinib compared with the carboplatin-paclitaxel combination for PFS (HR for progression or death, 0.74; 95% CI, 0.65–0.85; P < .001).
-
The median PFS was 5.7 months in the gefitinib group and 5.8 months in the carboplatin-paclitaxel group.[52][Level of evidence: 1iDiii]
-
Following the time that chemotherapy was discontinued and while gefitinib was continued, the PFS curves clearly separated and favored gefitinib.
-
The 12-month PFS rates were 24.9% with the gefitinib group and 6.7% with the carboplatin-paclitaxel group.
-
-
More than 90% of the patients in the trial with mutations had either del19 or exon 21 L858R mutations, which have been shown to be sensitive to EGFR inhibitors. In the subgroup of patients with a mutation, PFS was significantly longer among those who received gefitinib (HR, 0.48; 95% CI, 0.36–0.64; P < .001); however, in the subgroup of patients who were negative for a mutation, PFS was significantly longer in those who received the carboplatin-paclitaxel combination (HR with gefitinib, 2.85; 95% CI, 2.05–3.98; P < .001). There was a significant interaction between treatment and EGFR mutation with respect to PFS (P < .001).[52]
-
OS was similar for patients who received gefitinib and carboplatin-paclitaxel, with no significant difference between treatments overall (HR, 0.90; 95% CI, 0.79–1.02; P = .109) or in EGFR mutation–positive (HR, 1.00; 95% CI, 0.76–1.33; P = .990) or EGFR mutation–negative (HR, 1.18; 95% CI, 0.86–1.63; P = .309; treatment by EGFR mutation interaction P = .480) subgroups. A high proportion (64.3%) of EGFR mutation–positive patients randomly assigned to the carboplatin-paclitaxel regimen received subsequent EGFR TKIs. PFS was significantly longer with gefitinib for patients whose tumors had both high EGFR gene copy number and EGFR mutation (HR, 0.48; 95% CI, 0.34–0.67) but significantly shorter when high EGFR gene copy number was not accompanied by EGFR mutation (HR, 3.85; 95% CI, 2.09–7.09).
-
-
Two phase III trials from Japan prospectively confirmed that patients with NSCLC and EGFR mutations have improved PFS but not OS when treated with gefitinib.[53,54]
-
In the first trial, 230 chemotherapy-naïve patients with metastatic NSCLC and EGFR mutations were randomly assigned to receive gefitinib or carboplatin-paclitaxel.[53]
-
In the planned interim analysis of data for the first 200 patients, PFS was significantly longer in the gefitinib group than in the standard-chemotherapy group (HRdeath or disease progression with gefitinib, 0.36; P < .001), resulting in early termination of the study.
-
The gefitinib group had a significantly longer median PFS (10.8 months vs. 5.4 months in the chemotherapy group; HR, 0.30; 95% CI, 0.22–0.41; P < .001).[53][Level of evidence: 1iiDiii] The median OS was 30.5 months in the gefitinib group and 23.6 months in the standard chemotherapy group (P = .31).
-
-
In the second trial, the West Japanese Oncology Group conducted a phase III study (WJTOG3405) in 177 chemotherapy-naïve patients aged 75 years or younger and diagnosed with stage IIIB/IV NSCLC or postoperative recurrence harboring EGFR mutations (either the exon 19 deletion or L858R-point mutation).[54]
-
Patients were randomly assigned to receive either gefitinib or cisplatin plus docetaxel (administered every 21 days for three to six cycles). The primary endpoint was PFS.
-
The gefitinib group had significantly longer PFS than the cisplatin-plus-docetaxel group, with a median PFS of 9.2 months (95% CI, 8.0–13.9) versus 6.3 months (range, 5.8–7.8 months; HR, 0.489; 95% CI, 0.336–0.710, log-rank; P < .0001).[54][Level of evidence: 1iiDiii]
-
-
Erlotinib
Evidence (erlotinib):
-
In an open-label, randomized, phase III trial (NCT00874419) from China, 165 patients older than 18 years with histologically confirmed stage IIIB/IV NSCLC and a confirmed activating mutation of EGFR (i.e., exon 19 deletion or exon 21 L858R-point mutation) received either oral erlotinib (150 mg/day) until they experienced disease progression or unacceptable toxic effects, or up to four cycles of gemcitabine plus carboplatin.[55]
-
Median PFS was significantly longer in erlotinib-treated patients than in patients treated with chemotherapy (13.1 months [95% CI, 10.58–16.53] vs. 4.6 months [range, 4.21–5.42 months]; HR, 0.16; 95% CI, 0.10–0.26; P < .0001).[55][Level of evidence: 1iiDiii]
-
-
In a European study (EURTAC [NCT00446225]), 1,227 patients with advanced NSCLC were screened for EGFR mutations. Of these, 174 patients with EGFR mutations were randomly assigned to receive erlotinib or platinum-based chemotherapy.[56] The primary endpoint was PFS.
-
In an interim analysis of the first 153 patients, PFS in the chemotherapy arm was 5.2 months (95% CI, 4.5–5.8) compared with 9.7 months (95% CI, 8.4–12.3) in the erlotinib arm (HR, 0.37; P < .0001). Median survival was 19.3 months in patients in the chemotherapy arm and 19.5 months in patients in the erlotinib arm (HR, 0.80; P = .42).[57][Level of evidence: 1iiDiii]
-
Afatinib
Evidence (afatinib):
-
In an open-label, randomized, phase III study (LUX-Lung 3 [NCT00949650]), 345 Asian (72%) and white (26%) patients with stage IIIB/IV NSCLC and confirmed EGFR mutations (i.e., exon 19 deletion, L858R, or other [38 of 345 patients had other less-common mutations]) were screened, and 340 patients received at least one dose of study medication, which was either 40 mg of oral afatinib, an irreversible EGFR/human epidermal receptor (HER) TKI, daily or up to six cycles of cisplatin and pemetrexed for first-line treatment.[58]
-
The primary endpoint was PFS. In this study, the afatinib group had significantly longer PFS than the cisplatin-plus-pemetrexed group, with a median PFS of 11.1 months for afatinib and 6.9 months for chemotherapy (HR, 0.58; 95% CI, 0.43–0.78; P = .001).[58][Level of evidence: 1iiDiii]
-
Assessment of OS was a secondary endpoint and was reported separately.[59] Similar to the PFS analysis, OS was stratified based on EGFR-mutation type and ethnic origin.
-
With a median follow-up of 41 months, median OS was 28.2 months in patients in both arms (HR, 0.88; 95% CI, 0.66–1.17; P = .39).
-
In patients harboring common EGFR mutations (i.e., exon 19 deletion and L858R), survival did not differ significantly between treatment arms (HR, 0.78; 95% CI, 0.58–1.06; P = .11). However, prespecified subgroup analyses demonstrated a survival advantage with afatinib compared with chemotherapy in patients with tumors harboring the EGFR del19 mutation (median OS, 33.3 months vs. 21.1 months; HR, 0.54; 95% CI, 0.36–0.79; P = .0015) but no significant difference between treatment arms in patients with tumors harboring the L858R mutation (median OS, 27.6 months vs. 40.3 months; HR, 1.30; 95% CI, 0.80–2.11; P = .29).
-
First-line afatinib was associated with a significant survival advantage compared with chemotherapy in patients with NSCLC-harboring EGFR del19 mutations but not in patients with EGFR L858R mutations or in the overall EGFR–mutation-positive patient population.[59][Level of evidence: 1iiA]
-
-
-
In an open-label, randomized, phase III study (LUX-Lung 6 [NCT01121393]), 364 East Asian patients with stage IIIB/IV NSCLC and confirmed EGFR mutations (i.e., exon 19 deletion, L858R, or other) were randomly assigned (2:1 ratio) to 40 mg of afatinib daily or gemcitabine and cisplatin for up to six cycles for first-line treatment.[60]
-
The primary endpoint was PFS. Median PFS was significantly longer in the afatinib group (11.0 months; 95% CI, 9.7–13.7) than in the gemcitabine and cisplatin group (5.6 months, [range, 5.1–6.7 months]; HR, 0.28; 95% CI, 0.20–0.39; P < .0001).[60][Level of evidence: 1iiDiii]
-
Assessment of OS was a prespecified secondary endpoint and was reported separately.[59] Similar to the PFS analysis, OS was stratified based on EGFR-mutation type and ethnic origin.
-
With a median follow-up of 33 months, median OS was 23.1 months in patients in the afatinib arm and 23.5 months in patients in the chemotherapy arm (HR, 0.93; 95% CI, 0.72–1.22; P = .61).
-
In patients harboring common EGFR mutations (i.e., exon 19 deletion and L858R), survival did not differ significantly between treatment arms (HR, 0.83; 95% CI, 0.62–1.09; P = .18). However, prespecified subgroup analyses demonstrated a survival advantage with afatinib compared with chemotherapy in patients with tumors harboring the EGFR del19 mutation (median OS, 31.4 months vs. 18.4 months; HR, 0.64; 95% CI, 0.44–0.94; P = .023), but no significant difference between treatment arms was seen in patients with tumors harboring the L858R mutation (median OS, 19.6 months vs. 24.3 months; HR, 1.22; 95% CI, 0.81–1.83; P = .34).
-
First-line afatinib was associated with a significant survival advantage compared with chemotherapy in patients with NSCLC-harboring EGFR del19 mutations but not in patients with EGFR L858R mutations or in the overall EGFR-mutation-positive patient population.[59][Level of evidence: 1iiA]
-
-
ALK inhibitors (for patients with ALK translocations)
Alectinib
Evidence (alectinib):
-
In an open-label, randomized, phase III study (the ALEX trial [NCT02075840]), 303 patients with previously untreated, advanced ALK-rearranged NSCLC received either alectinib (600 mg bid) or crizotinib (250 mg bid).[61] The primary endpoint was investigator-assessed PFS.
-
The rate of PFS was significantly higher with alectinib than crizotinib; the 12-month event-free survival was 68.4% for the alectinib group (95% CI, 40.4–56.9) compared with 48.7% for the crizotinib group (95% CI, 40.4–56.9) (HR, 0.47; 95% CI, 0.34–0.65; P < .001). The median PFS was not reached with alectinib. The results of independent review committee-assessed PFS were consistent.[61][Level of evidence: 1iiDiii]
-
Central nervous system progression events were less frequent with alectinib (12%) than with crizotinib (45%) (HR, 0.16; 95% CI, 0.10–0.28; P <.001).
-
The response rate was similar for both groups, 82.9% for the alectinib group compared with 75.5% for the crizotinib group (P = .09).
-
Grade 3 to 5 adverse events were less frequent with alectinib (41%) than with crizotinib (50%).
-
-
A second, open-label, randomized, phase III trial (J-ALEX) recruited 207 ALK-inhibitor–naïve Japanese patients with ALK-positive NSCLC who were chemotherapy-naïve or had received one previous chemotherapy regimen. Patients were randomly assigned in a 1:1 ratio to receive alectinib (300 mg bid, which is the dose approved in Japan and is lower than the 600 mg twice daily dose approved elsewhere) versus crizotinib (250 mg bid).[62] The primary endpoint was PFS-assessed by an independent review committee.
-
At data cutoff for the second primary interim analysis, the independent data monitoring committee determined that the primary endpoint was met (HR, 0.34; 99.7% CI, 0.17–0.71; P <.0001) and recommended immediate release of the data. Median PFS had not been reached with alectinib but was reached at 10.2 months with crizotinib.
-
Grade 3 or 4 adverse events occurred less frequently with alectinib (26% occurrence rate) than with crizotinib (52% occurrence rate).
-
Crizotinib
Evidence (crizotinib):
-
In an open-label, randomized, phase III study, 343 patients with stage IIIB/IV NSCLC harboring translocations in ALK received either 250 mg of crizotinib orally twice a day or the combination of pemetrexed and cisplatin or carboplatin for up to six cycles.[63] At the time of disease progression, patients on the chemotherapy arm were allowed to cross over to crizotinib; 60% of patients in the chemotherapy arm subsequently received crizotinib. The primary endpoint of this study was PFS.
-
The study met its primary endpoint and demonstrated that crizotinib is superior to chemotherapy in prolonging PFS (median, 10.9 months vs. 7.0 months; HR, 0.454; 95% CI, 0.346–0.596; P < .0001).[64][Level of evidence: 1iiDiii]
-
Ceritinib
Evidence (ceritinib):
-
In an open-label, randomized, phase III study, 376 patients with stage IIIB/IV ALK-rearranged nonsquamous NSCLC received either oral ceritinib 750 mg daily or platinum-based chemotherapy (cisplatin or carboplatin and pemetrexed) every 3 weeks for four cycles, followed by maintenance pemetrexed.[65] The primary endpoint was PFS and crossover from chemotherapy to ceritinib was allowed upon documented progression.
-
Median PFS, assessed by blinded independent review, was 16.6 months in the ceritinib group and 8.1 months in the chemotherapy group (HR, 0.55; 95% CI, 0.42–0.73; P < .00001).
-
The median OS was not reached with ceritinib, and it was 26.2 months with chemotherapy (HR, 0.73; 95% CI, 0.50–1.08; P = .056).[65][Level of evidence: 1iiDiii]
-
ROS1 inhibitors (for patients with ROS1 rearrangements)
ROS1 rearrangements occur in approximately 1% of patients with NSCLC.[66]
Crizotinib
Evidence (crizotinib):
-
In an expansion cohort of a phase I study of crizotinib, 50 patients with advanced NSCLC who tested positive for ROS1 rearrangement were treated with oral crizotinib 250 mg twice daily.[67] ROS1 rearrangements were identified using break-apart fluorescence in situ hybridization or reverse-transcriptase-polymerase-chain-reaction assay. Seven patients (14%) had not had any previous treatment for advanced disease, 21 patients (42%) had one prior treatment, and 22 patients (44%) had more than one prior treatment. The primary endpoint was response rate.
-
The overall response rate was 72% (95% CI, 58–84). Six percent of patients had a complete response, 66% had a partial response, and 18% had stable disease as their best response.
-
Median PFS was 19.2 months (95% CI, 14.4–not reached). The estimated duration of response was 17.6 months (95% CI, 14.5–not reached).[67][Level of evidence: 3iiiDiv]
-
-
In a phase II, open-label, single-arm trial, 127 East Asian patients with ROS1-positive NSCLC were treated with crizotinib 250 mg twice daily.[68] Twenty-four patients (18.9%) had not had any previous treatment for advanced disease, 53 patients (41.7%) had one previous treatment, and 50 patients (39%) had two or three previous treatments. The primary endpoint was objective response rate by independent review.
-
The objective response rate was 71.7% (95% CI, 63.0–79.3). Response rates were similar, irrespective of the number of previous therapies. Complete responses occurred in 13.4% of patients, while 58.3% of patients had partial responses, and 16.5% of patients had stable disease as their best response.[68][Level of evidence: 3iiiDiv]
-
Median PFS was 15.9 months (95% CI, 12.9–24). The duration of response was 19.7 months (95% CI, 14.1–not reached).
-
OS was 32.5 months (95% CI, 32.5–not reached).
-
Crizotinib was approved for patients with metastatic NSCLC whose tumors are ROS1-positive, regardless of the number of previous systemic therapies.
BRAFV600E and MEK inhibitors (for patients with BRAFV600E mutations)
BRAFV600E mutations occur in 1% to 2% of lung adenocarcinomas.
Dabrafenib and trametinib
Evidence (dabrafenib and trametinib):
-
In a phase II multi-center, non-randomized, open-label study (NCT01336634), 36 patients with previously untreated metastatic NSCLC who tested positive for BRAFV600E mutations were treated with dabrafenib (a BRAF inhibitor) 150 mg bid and trametinib (a MEK inhibitor) 2 mg qd.[69] BRAFV600E mutations were identified by the Oncomine Dx Target Test (ThermoFisher Scientific). The primary endpoint was investigator-assessed overall response.
-
The overall response rate was 64% (95% CI, 46–79). Six percent of patients had a complete response, and 58% of patients had a partial response.
-
The median investigator-assessed PFS was 10.9 months (95% CI, 7.0–16.6 months). The estimated median duration of response was 10.4 months (95% CI, 8.3–17.9). At data cutoff, 47% of patients had died, and the median OS was 24.6 months (95% CI, 12.3–not estimable).
-
Sixty-nine percent of patients had at least one grade 3 or 4 adverse event, of which the most common were pyrexia, alanine aminotransferase increase, hypertension, or vomiting. Adverse events led to permanent discontinuation in 22% of patients, dose interruption or delay in 75% of patients, and dose reduction in 39% of patients.[69][Level of evidence: 3iiiDiv]
-
The combination of dabrafenib and trametinib received approval in the treatment of patients with NSCLC whose tumors harbor BRAFV600E mutations as detected by a U.S. Food and Drug Administration (FDA)-approved test.
Immune checkpoint inhibitors with or without chemotherapy
Pembrolizumab
Pembrolizumab is a humanized monoclonal antibody that inhibits the interaction between the PD-1 coinhibitory immune checkpoint expressed on tumor cells and infiltrating immune cells and its ligands, PD-L1 and PD-L2.[70]
Evidence (pembrolizumab plus chemotherapy):
-
A phase III double-blind trial (KEYNOTE-189 [NCT02578680]) randomly assigned, in a 2:1 ratio, 616 patients with metastatic nonsquamous NSCLC without sensitizing EGFR mutations or ALK rearrangements who had received no previous treatment for metastatic disease. Patients received pemetrexed and a platinum-based drug plus either 200 mg of pembrolizumab or placebo every 3 weeks for 4 cycles, followed by pembrolizumab or placebo for up to a total of 35 cycles plus pemetrexed maintenance.[2] Crossover to pembrolizumab monotherapy was permitted after verified progression among patients in the placebo-containing combination group. The primary endpoints were OS and PFS as assessed by blinded independent central committee radiologic review.
-
After a median follow-up of 10.5 months, the estimated rate of OS at 12 months was 69.2% (95% CI, 64.1–73.8) in the pembrolizumab combination group compared with 49.4% (95% CI, 42.1–56.2) in the placebo combination group (HR, 0.49; 95% CI, 0.38–0.64; P < .001).[2][Level of evidence: 1iA]
-
Improvement in survival was seen across all PD-L1 categories.
-
Median PFS was 8.8 months in the pembrolizumab combination group compared with 4.9 months in the placebo combination group (HR, 0.52; 95% CI, 0.43–0.64; P < .001).
-
Adverse events of grade 3 or higher occurred with similar frequency in both treatment groups (67.2% in the pembrolizumab combination group vs. 65.8% in the placebo combination group).
-
Evidence (pembrolizumab alone):
-
A phase III, open-label study (KEYNOTE-024) randomly assigned 305 patients with previously untreated, advanced NSCLC with PD-L1 expression on 50% or more tumor cells and no sensitizing EGFR mutations or ALK translocations to either intravenous pembrolizumab (200 mg every 3 weeks for up to 35 cycles) or platinum-based chemotherapy (4–6 cycles, investigator’s choice; pemetrexed maintenance was allowed for nonsquamous tumors).[70] The primary endpoint was PFS.
-
PD-L1 expression was centrally assessed using the PD-L1 immunohistochemistry 22C3 pharmDx assay (Dako North America). PD-L1 tumor expression of 50% or more was found in 30.2% of 1,653 patient samples that were examined.
-
Pembrolizumab demonstrated significant improvement in median PFS (10.3 months vs. 6.0 months; HR, 0.50; 95% CI, 0.37–0.68; P < .001). The overall response rate (44.8% vs. 27.8%), the median duration of response (not reached, [range 1.9+–14.5+ months] vs. 6.3 months [range, 2.1+–12.6+ months]), and the estimated rate of OS at 6 months (80.2% vs. 72.4%; HR, 0.60; 95% CI, 0.41–0.89; P = .005) were all higher with pembrolizumab than with chemotherapy.
-
Adverse events (any grade) were less frequent with pembrolizumab than with chemotherapy (73.4% vs. 90.0%).
-
Grade 3–5 adverse events occurred in 26.6% of patients treated with pembrolizumab and 53.3% of patients treated with chemotherapy.
-
Grade 3 or 4 immune-related events occurred in 9.7% of patients treated with pembrolizumab and 0.7% of patients treated with chemotherapy.
-
The most common grade 3 or 4 immune-related events associated with pembrolizumab were severe skin reactions (3.9%), pneumonitis (2.6%), and colitis (1.3%).
-
There were no grade 5 immune-related events.
-
-
Pembrolizumab treatment demonstrated significant improvement in PFS, OS, and duration of response with less frequent adverse events compared with chemotherapy treatment.[70][Level of evidence: 1iiDiii]
-
Pembrolizumab in combination with pemetrexed and carboplatin received FDA approval as first-line treatment of patients with metastatic nonsquamous NSCLC, regardless of PD-L1 expression. Pembrolizumab also received approval as a first-line monotherapy for patients with NSCLC whose tumors express PD-L1 (≥50% staining as determined by a test approved by the FDA). Patients with EGFR or ALK genomic tumor aberrations should have disease progression on FDA-approved therapies before receiving pembrolizumab (refer to the FDA label for pembrolizumab).
Local therapies and special considerations
Endobronchial laser therapy and/or brachytherapy (for obstruction lesions)
Radiation therapy may be effective in palliating symptomatic patients with local involvement of NSCLC with any of the following:
-
Tracheal, esophageal, or bronchial compression.
-
Pain.
-
Vocal cord paralysis.
-
Hemoptysis.
-
Superior vena cava syndrome.
In some cases, endobronchial laser therapy and/or brachytherapy have been used to alleviate proximal obstructing lesions.[19]
EBRT (primarily for palliation of local symptomatic tumor growth)
Although EBRT is frequently prescribed for symptom palliation, there is no consensus on which fractionation scheme should be used. Although different multifraction regimens appear to provide similar symptom relief,[71–76] single-fraction radiation may be insufficient for symptom relief compared with hypofractionated or standard regimens, as evidenced in the NCT00003685 trial.[20][Level of evidence: 1iiC] Evidence of a modest increase in survival in patients with a better PS given high-dose radiation therapy is available.[22,77][Level of evidence: 1iiA] In closely observed asymptomatic patients, treatment may often be appropriately deferred until symptoms or signs of a progressive tumor develop.
Evidence (radiation therapy):
-
A systematic review identified six randomized trials of high-dose rate endobronchial brachytherapy (HDREB) alone or with EBRT or laser therapy.[78]
-
Better overall symptom palliation and fewer re-treatments were required in previously untreated patients using EBRT alone.[78][Level of evidence: 1iiC]
-
HDREB provided palliation of symptomatic patients with recurrent endobronchial obstruction previously treated by EBRT, when it was technically feasible.
-
Treatment of second primary tumor
A solitary pulmonary metastasis from an initially resected bronchogenic carcinoma is unusual. The lung is frequently the site of second primary malignancies in patients with primary lung cancers. Whether the new lesion is a new primary cancer or a metastasis may be difficult to determine. Studies have indicated that in most patients the new lesion is a second primary tumor, and after its resection, some patients may achieve long-term survival. Thus, if the first primary tumor has been controlled, the second primary tumor should be resected, if possible.[79,80]
Treatment of brain metastases
Patients who present with a solitary cerebral metastasis after resection of a primary NSCLC lesion and who have no evidence of extracranial tumor can achieve prolonged disease-free survival with surgical excision of the brain metastasis and postoperative whole-brain radiation therapy.[81,82] Unresectable brain metastases in this setting may be treated with stereotactic radiosurgery.[83]
Approximately 50% of patients treated with resection and postoperative radiation therapy will develop recurrence in the brain; some of these patients will be suitable for additional treatment.[84] In those selected patients with good PS and without progressive metastases outside of the brain, treatment options include reoperation or stereotactic radiation surgery.[83,84] For most patients, additional radiation therapy can be considered; however, the palliative benefit of this treatment is limited.[85][Level of evidence: 3iiiDiii]
Treatment Options Under Clinical Evaluation for Newly Diagnosed Stage IV, Relapsed, and Recurrent NSCLC (First-line Therapy)
Treatment options under clinical evaluation for newly diagnosed stage IV, recurrent, and relapsed NSCLC (first-line therapy) include the following:
-
Clinical trials can be considered as first-line therapy.
Current Clinical Trials
Use our advanced clinical trial search to find NCI-supported cancer clinical trials that are now enrolling patients. The search can be narrowed by location of the trial, type of treatment, name of the drug, and other criteria. General information about clinical trials is also available
Progressive Stage IV, Relapsed, and Recurrent NSCLC Treatment
Standard Treatment Options for Progressive Stage IV, Relapsed, and Recurrent NSCLC (Second-line Therapy)
Standard treatment options for patients with progressive stage IV, relapsed, and recurrent non-small cell lung cancer (NSCLC) (second-line therapy and beyond) include the following:
-
Epidermal growth factor receptor (EGFR)-directed therapy.
-
EGFR-directed therapy for acquired EGFR T790M mutations after prior EGFR-directed therapy.
Chemotherapy
The use of chemotherapy has produced objective responses and small improvement in survival for patients with metastatic disease.[1][Level of evidence: 1iiA] In studies that have examined symptomatic response, improvement in subjective symptoms has been reported to occur more frequently than objective response.[2,3] Informed patients with good performance status (PS) and symptomatic recurrence can be offered treatment with a platinum-based chemotherapy regimen for palliation of symptoms. For patients who have relapsed after platinum-based chemotherapy, second-line therapy can be considered.
Docetaxel
Evidence (docetaxel):
-
A meta-analysis of five trials of 865 patients assessing the efficacy and safety of docetaxel administered weekly or every 3 weeks has been reported.[7] In that analysis, the following was shown:
-
Median survival was 27.4 weeks for patients treated every 3 weeks and 26.1 weeks for patients treated weekly (P = .24, log-rank test).
-
Significantly less severe neutropenia and febrile neutropenia were reported with weekly docetaxel (P < .001 for both); however, no significant differences were observed for anemia, thrombocytopenia, and nonhematologic toxic effects.
-
Docetaxel plus ramucirumab
Evidence (docetaxel plus ramucirumab):
-
In a double-blind, placebo-controlled, phase III study, 1,253 patients with an Eastern Cooperative Oncology Group (ECOG) PS of 0 to 1 who had progressive disease after first-line chemotherapy were randomly assigned to receive docetaxel and placebo or docetaxel and ramucirumab.[8][Level of evidence: 1iiA] Ramucirumab is a human immunoglobulin G1 monoclonal antibody that targets the extracellular domain of vascular endothelial growth factor receptor 2. The primary endpoint of the study was overall survival (OS), with secondary endpoints of progression-free survival (PFS) and objective response rate (ORR). The study enrolled patients with either nonsquamous or squamous NSCLC; however, patients with poorly controlled hypertension, gastrointestinal perforation or fistulae, arterial thromboembolic event within 6 months (before random assignment), gross hemoptysis within 2 months, or grade 3 to 4 gastrointestinal bleeding within 3 months were excluded. In addition, the trial did not include patients with tumors that had major blood vessel involvement or intratumor cavitation.
-
The addition of ramucirumab to docetaxel compared with placebo plus docetaxel led to an increase in median OS (10.5 months vs. 9.1 months; hazard ratio [HR], 0.86; 95% confidence interval [CI], 0.75–0.98), ORR (23% vs. 14%), and PFS (4.5 months vs. 3 months). The improvement in OS from the addition of ramucirumab appeared consistent across subgroups including squamous and nonsquamous histologies.
-
Grade 3 to 4 treatment-related adverse events occurred in 79% of patients who received docetaxel and ramucirumab as compared with 71% of patients who received docetaxel and placebo. Febrile neutropenia, fatigue, and hypertension were among the toxicities that were more common with the addition of ramucirumab to docetaxel. There was no significant difference in the incidence of grades 3 to 4 hemorrhage between the groups.
-
On the basis of this study, the addition of ramucirumab to docetaxel chemotherapy can be considered for patients with good PS with advanced NSCLC who have progressive disease after first-line chemotherapy.
-
Pemetrexed
Evidence (pemetrexed):
-
A randomized, phase III trial of 571 patients designed to demonstrate the noninferiority of pemetrexed compared with docetaxel showed no difference in response rates, PFS, or OS.[9][Level of evidence: 1iiA] Of note, patients with squamous histology benefited from docetaxel, and those with nonsquamous histologies appeared to benefit more from pemetrexed.[10]
EGFR-directed therapy
EGFR-directed therapy after first-line chemotherapy
Erlotinib
Evidence (erlotinib):
-
Two randomized, placebo-controlled trials indicated that erlotinib prolongs survival and time to deterioration in symptoms in patients with NSCLC after first-line or second-line chemotherapy compared with placebo [11,12] but does not improve survival compared with standard second-line chemotherapy with docetaxel or pemetrexed.[13]
-
The trial of erlotinib versus best supportive care included 731 patients; 49% had received two previous chemotherapy regimens, and 93% had received platinum-based chemotherapy.
-
OS was 6.7 months among those who had received two previous chemotherapy regimens and 4.7 months among those who had received platinum-based chemotherapy. The HR was 0.70 (P < .001) in favor of erlotinib.[11][Level of evidence: 1iiA]
-
-
In the trial (NCT00556322), which was designed to show the superiority of erlotinib versus standard second-line chemotherapy after disease progression on first-line platinum combination therapy, 424 patients were randomly assigned.
-
There was no difference in the primary endpoint of OS (median OS, 5.3 months vs. 5.5 months; HR, 0.96; 95% CI, 0.78–1.19).[13][Level of evidence: 1iiA]
-
-
Gefitinib
Evidence (gefitinib):
-
A randomized phase III trial evaluated gefitinib versus placebo in 1,692 previously treated NSCLC patients and showed the following:
-
Gefitinib does not improve OS.
-
Median survival did not differ significantly between the groups in the overall population (5.6 months for gefitinib and 5.1 months for placebo; HR, 0.89; 95% CI, 0.77–1.02; P = .087) or among the 812 patients with adenocarcinoma (6.3 months vs. 5.4 months; HR, 0.84; CI, 0.68–1.03; P = .089).
-
Preplanned subgroup analyses showed significantly longer survival in the gefitinib group than in the placebo group for never-smokers (n = 375; 95% CI, 0.67 [0.49–0.92]; P = .012; median survival 8.9 months vs. 6.1 months) and for patients of Asian origin (n = 342; 95% CI, 0.66 [0.48–0.91]; P = .01; median survival 9.5 months vs. 5.5 months).[14][Level of evidence: 1iiA]
-
-
In a large, randomized trial, gefitinib was compared with docetaxel in patients with locally advanced or metastatic NSCLC who had been pretreated with platinum-based chemotherapy.[15] The primary objective was to compare OS between the groups with coprimary analyses to assess noninferiority in the overall population and superiority in patients with high EGFR gene copy number in the intention-to-treat population. The 1,466 patients were randomly assigned to receive gefitinib (250 mg per day PO; n = 733) or docetaxel (75 mg/m2 IV every 3 weeks; n = 733).
-
Noninferiority of gefitinib compared with docetaxel was confirmed for OS (HR, 1.020; 95% CI, 0.905–1.150). However, superiority of gefitinib in patients with high EGFR gene copy number (85 patients vs. 89 patients) was not proven (HR, 1.09; 95% CI, 0.78–1.51; P = .62).
-
In the gefitinib group, the most common adverse events were rash or acne (49% vs. 10%) and diarrhea (35% vs. 25%). In the docetaxel group, neutropenia (5% vs. 74%), asthenia (25% vs. 47%), and alopecia (3% vs. 36%) were most common.
-
This trial established noninferior survival of patients treated with gefitinib compared with docetaxel, suggesting that gefitinib is a valid treatment for pretreated patients with advanced NSCLC.
-
ORR to erlotinib and gefitinib are higher in patients who have never smoked, in females, in East Asians, and in patients with adenocarcinoma and bronchioloalveolar carcinoma.[16–22] Responses may be associated with sensitizing mutations in the tyrosine kinase domain of the EGFR- [17–19,21,22] and, with the absence of, K-RASmutations.[20–22][Level of evidence: 3iiiDiii] Survival benefit may be greater in patients with EGFR protein expression by immunohistochemistry or increased EGFR gene copy number by fluorescence in situ hybridization studies,[21,22] but the clinical utility of EGFR testing by immunohistochemistry has been questioned.[23]
Afatinib
Evidence (afatinib):
-
Afatinib, an irreversible inhibitor of the ErbB-family of receptors, has been compared with erlotinib as second-line treatment in patients with advanced squamous cell carcinoma. In a randomized, controlled, phase III trial (LUX-Lung 8 [NCT01523587]), patients with stage IIIB/IV squamous cell NSCLC with disease progression after frontline platinum-based chemotherapy were randomly assigned in a 1:1 ratio to receive afatinib (398 patients, 40 mg PO qd) or erlotinib (397 patients, 150 mg PO qd).[24][Level of evidence: 1iiDiii] The primary endpoint was PFS. Secondary endpoints included OS and response rate.
-
After a median follow-up of 6.7 months, the PFS was 2.4 months versus 1.9 months (HR, 0.82; 95% CI, 0.68–1.00).
-
After a median follow-up of 18.4 months, the median OS was significantly longer in the afatinib arm (7.9 months vs. 6.8 months; HR, 0.81; 95% CI, 0.69–0.95; P = .007). Survival at 6 months (63.6% vs. 54.6%; P = .009), 12 months (36.4% vs. 28.2%; P = .015), and 18 months (22% vs. 14.4%; P = .013) were all significantly better in patients who received afatinib.
-
There was no significant difference in response rate between the two arms (6% vs. 3%; P = .551).
-
The frequency of adverse events was similar between the two groups with 57% of the patients experiencing a rate of grade 3 or higher adverse events. Grade 3 treatment-related diarrhea and stomatitis occurred more frequently with afatinib; however, grade 3 rash or acne were more common in patients who received erlotinib.
-
Afatinib, as compared with erlotinib, represents another option for the second-line treatment of patients with stage IV squamous cell NSCLC.
-
EGFR-directed therapy for acquired EGFR T790M mutations after prior EGFR-directed therapy
Osimertinib
Evidence (osimertinib):
-
An open-label, phase III trial (AURA 3 [NCT02151981]) studied osimertinib in NSCLC patients with EGFR-sensitizing mutations whose disease had progressed after first-line EGFR inhibitors and who had the T790M EGFR resistance mutation as determined by the Cobas® EGFR Mutation Test.[25] The trial randomly assigned 419 patients (with a 2:1 ratio) to receive either osimertinib 80 mg PO qd or pemetrexed plus carboplatin or cisplatin IV every 3 weeks for up to six cycles; maintenance pemetrexed was allowed for the chemotherapy group. The primary endpoint was PFS.
-
Osimertinib was superior to chemotherapy in prolonging median PFS (10.1 months vs. 4.4 months; HR, 0.30; 95% CI, 0.23–0.41; P < .001).
-
The ORR was 71% with osimertinib versus 31% with platinum therapy (odds ratio for objective response, 5.39; 95% CI, 3.47–8.48; P < .001).
-
Among 144 patients with central nervous system (CNS) metastases, median PFS duration was 8.5 months with osimertinib versus 4.2 months with platinum therapy (HR, 0.32; 95% CI, 0.21–0.49).
-
Adverse events of grade 3 or greater occurred in 23% of osimertinib-treated patients versus 47% of platinum-treated patients.[25][Level of evidence: 1iiDiii]
-
ALK-directed tyrosine kinase inhibitors (TKI)
ALK-directed TKI after first-line chemotherapy
Crizotinib
Evidence (crizotinib):
-
A study (NCT00585195) that screened 1,500 patients with NSCLC for ALK rearrangements identified 82 patients with advanced ALK-positive disease who were enrolled in a clinical trial that was an expanded cohort study instituted after phase I dose escalation had established a recommended dose of crizotinib dual and ALK inhibitor of 250 mg bid in 28-day cycles.[26] Most of the patients had received previous treatment.
-
At a mean treatment duration of 6.4 months, the overall response rate was 57% (47 of 82 patients, with 46 confirmed partial responses, and one confirmed complete response); 27 patients (33%) had stable disease.[26][Level of evidence: 3iiiD]
-
The estimated probability of 6-month PFS was 72%.
-
1-year OS was 74% (95% CI, 63–82), and 2-year OS was 54% (40–66).
-
Survival in 30 ALK-positive patients who were given crizotinib in the second-line or third-line setting was significantly longer than in 23 ALK-positive controls identified from a different cohort given any second-line therapy (median OS not reached [95% CI, 14 months–not reached] vs. 6 months [95% CI, 4–17], 1-year OS, 70% [95% CI, 50–83] vs. 44% [95% CI, 23–64], and 2-year OS, 55% [33–72] vs. 12% [2–30]; HR, 0.36; 95% CI, 0.17–0.75; P = .004).[27][Level of evidence: 3iiiD]
-
Common toxicities were grade 1 or 2 (mild) gastrointestinal side effects.
-
Patients with ALK rearrangements tended to be younger than those without the rearrangements; most of the patients had little or no exposure to tobacco; and the patients had adenocarcinomas.
-
-
In an open-label, randomized, phase III study, 347 patients with stage IIIB/IV NSCLC-harboring translocations in ALK, who had received one previous regimen of platinum-based chemotherapy, received either crizotinib (250 mg PO twice a day) or chemotherapy (pemetrexed 500 mg/m2 if pemetrexed-naïve or docetaxel 75mg/m2IV every 21 days).[28]
-
The primary endpoint was PFS. Median PFS was significantly longer in favor of crizotinib (7.7 months vs. 3.0 months, P < .001).[28][Level of evidence: 1iiDiii]
-
OS, a secondary endpoint, was not significantly different, but there was significant crossover in the design.
-
ALK-directed TKI after prior ALK TKI therapy
Ceritinib
Evidence (ceritinib):
-
A single-arm, open-label trial enrolled 163 patients with ALK-translocated stage IIIB/IV NSCLC who had disease progression while receiving crizotinib or were intolerant to the drug.[29]
-
The primary endpoint was ORR according to Response Evaluation Criteria In Solid Tumors (RECIST, version 1.0) with a secondary endpoint of duration of response (DOR). The ORR by blinded independent review was 43.6% (95% CI, 36–52), and the median DOR was 7.1 months (range, 5.6–not estimable).[29][Level of evidence: 3iiiDiv]
-
Of note, 38% of patients required dose modification because of gastrointestinal toxicity; elevation of alanine transaminase to more than five times the upper limit of normal occurred in 27% of patients.
-
Alectinib
Evidence (alectinib):
-
A phase II, open-label trial (NCT01871805) enrolled 87 patients with ALK-translocated stage IIIB/IV NSCLC who had disease progression after crizotinib treatment.[30]
-
The primary endpoint was objective response according to RECIST (version 1.1). At the time of primary endpoint analysis of this ongoing study, 48% of patients (95% CI, 36–60) had a confirmed partial response, and 32% had stable disease by blinded independent review. The median DOR was 13.5 months (95% CI, 6.7–not estimable). The estimated median PFS was 8.1 months (95% CI, 6.2–12.6).[30][Level of evidence: 3iiiDiv]
-
Sixteen patients had measurable CNS disease at baseline, of whom 11 had received prior radiation therapy. The CNS ORR was 75% (95% CI, 48–93), with 25% of the patients attaining complete response and 50% of the patients attaining partial response.
-
The most common side effects were grade 1 or 2 in severity; the most frequent adverse events, occurring in 23% to 36% of patients, were constipation, fatigue, myalgia, and peripheral edema. Dose interruption was needed in 36% of patients, and dose reduction occurred in 16%.
-
-
A second phase II, open-label trial enrolled 138 patients with ALK-positive stage IIIB/IV NSCLC who had disease progression on crizotinib.[31]
-
The primary endpoint was ORR by independent central review. ORR was 50% (95% CI, 41–59). Median DOR was 11.2 months (95% CI, 9.6–not reached). Median PFS was 8.9 months (95% CI, 5.6–11.3).[31][Level of evidence: 3iiiDiv]
-
CNS ORR in 35 patients with measurable CNS lesions was 57% (95% CI, 39–74).
-
Common adverse events that were mainly grade 1 or 2, which occurred in 25% to 33% of patients, were constipation, fatigue, and peripheral edema.
-
Brigatinib
Evidence (brigatinib):
-
A phase II, open-label trial (NCT02094573) enrolled 222 patients with ALK-translocated locally advanced or metastatic NSCLC who had disease progression after crizotinib treatment. Patients were randomly assigned to receive 90 mg qd (n = 112, 109 treated) or 180 mg qd with a 7-day lead-in at 90 mg qd (n = 110).[32]
-
The primary endpoint assessed by the investigators was ORR. ORR was 45% (97.5% CI, 34–56) for patients who received the 90 mg dose and 54% (97.5% CI, 43–65) for patients who received the 180 mg dose.
-
Median PFS was 9.2 months (95% CI, 7.4–15.6) for patients who received the 90 mg dose and 12.9 months (95% CI, 11.1–not reached) for patients who received the 180 mg dose.
-
At data cutoff, the median DOR was 13.8 months (95% CI, 5.6–13.8) for patients who received the 90 mg dose and 11.1 months (95% CI, 9.2–13.8) for patients who received the 180 mg dose.[32][Level of evidence: 1iiDiv]
-
The CNS ORR in patients with measurable CNS lesions was 42% in patients receiving 90 mg qd (n = 26) and 67% in patients receiving 180 mg qd (n = 18).
-
Common adverse events, which were mainly grade 1 or 2 and occurred in 27% to 38% of patients at the higher dose, were nausea, diarrhea, headache, and cough. A subset of pulmonary adverse events with early onset (median onset, day 2) occurred in 14 of 219 treated patients (all grades, 6% ≥ grade >3, 3%); none occurred after escalation to 180 mg. These events included dyspnea, hypoxia, cough, pneumonia, or pneumonitis. They were managed with dose interruption. Seven of the 14 patients were successfully retreated with brigatinib.
-
The U.S. Food and Drug Administration (FDA)-approved dose of brigatinib is 90 mg qd for 7 days; if tolerated, the dose is increased to 180 mg qd.
-
ROS1-directed therapy
ROS1 rearrangements occur in approximately 1% of patients with NSCLC.[33]
Crizotinib
Crizotinib was approved for patients with metastatic NSCLC whose tumors are ROS1-positive, regardless of the number of previous systemic therapies.
Evidence (crizotinib):
-
In an expansion cohort of a phase I study of crizotinib, 50 patients with advanced NSCLC who tested positive for ROS1 rearrangement were treated with oral crizotinib 250 mg twice daily.[34] ROS1 rearrangements were identified using break-apart fluorescence in situ hybridization or reverse-transcriptase-polymerase-chain-reaction assay. Seven patients (14%) had not had any previous treatment for advanced disease, 21 patients (42%) had one prior treatment, and 22 patients (44%) had more than one previous treatment. The primary endpoint was response rate.
-
The overall response rate was 72% (95% CI, 58–84). Six percent of patients had a complete response, 66% had a partial response, and 18% had stable disease as their best response.
-
Median PFS was 19.2 months (95% CI, 14.4–not reached). The estimated DOR was 17.6 months (95% CI, 14.5–not reached).[34][Level of evidence: 3iiiDiv]
-
-
In a phase II, open-label, single-arm trial, 127 East Asian patients with ROS1-positive NSCLC were treated with crizotinib 250 mg twice daily.[35] Twenty-four patients (18.9%) had not had any previous treatment for advanced disease, 53 patients (41.7%) had one previous treatment, and 50 patients (39%) had two or three previous treatments. The primary endpoint was objective response rate by independent review.
-
The objective response rate was 71.7% (95% CI, 63.0–79.3). Response rates were similar, irrespective of the number of previous therapies. Complete responses occurred in 13.4% of patients, while 58.3% of patients had partial responses and 16.5% of patients had stable disease as their best response.[35][Level of evidence: 3iiiDiv]
-
Median PFS was 15.9 months (95% CI, 12.9–24). The duration of response was 19.7 months (95% CI, 14.1–not reached).
-
OS was 32.5 months (95% CI, 32.5–not reached).
-
BRAFV600E and MEK inhibitors (for patients with BRAFV600E mutations)
BRAFV600E mutations occur in 1% to 2% of lung adenocarcinomas.
Dabrafenib and trametinib
Evidence (dabrafenib and trametinib):
-
In a phase II, multicenter, nonrandomized, open-label study (NCT01336634), 57 patients with progression after at least one to three previous platinum-containing regimens for treatment of metastatic NSCLC, who tested positive for BRAFV600E mutations, were treated with dabrafenib (a BRAF inhibitor) 150 mg bid and trametinib (a MEK inhibitor) 2 mg qd.[36] BRAFV600E mutations were ascertained by local testing. The primary endpoint was investigator-assessed overall response.
-
The overall response rate was 63.2% (95% CI, 49.3–75.6), as determined independently by investigator and independent review committee assessments. There were 2 out of 36 complete responses by investigator assessment; all responses were deemed partial by the independent review committee.
-
The median investigator-assessed PFS was 9.7 months (95% CI, 6.9–19.6 months). The estimated median DOR was 9.0 months (95% CI, 6.9–18.3). The OS data are immature.
-
Forty-nine percent of patients had at least one grade 3 or 4 adverse event, the most common of which were neutropenia, hyponatremia, and anemia.[36][Level of evidence: 3iiiDiv]
-
The combination of dabrafenib and trametinib received approval for patients with NSCLC whose tumors harbor BRAFV600E mutations as detected by an FDA-approved test.
Immunotherapy
Nivolumab is a fully human monoclonal antibody that inhibits the programmed death-1 (PD-1) co-inhibitory immune checkpoint expressed on tumor cells and infiltrating immune cells.[37,38] Pembrolizumab is a humanized monoclonal antibody that inhibits the interaction between the PD-1 co-inhibitory immune checkpoint expressed on tumor cells and infiltrating immune cells and its ligands, PD-L1 and PD-L2.[39] Atezolizumab is a PD-L1–blocking antibody.
Nivolumab
Evidence (nivolumab):
-
In two phase III clinical trials, one conducted in patients with advanced platinum-pretreated squamous NSCLC and the other trial conducted in patients with nonsquamous NSCLC, nivolumab demonstrated a significant improvement in OS compared with the previous standard treatment of docetaxel chemotherapy.[37,38][Level of evidence:1iiA] In addition, the rates of grade 3 and 4 treatment-related toxicity in both trials were significantly lower with nivolumab than with docetaxel. Of note, all patients enrolled in phase III studies of nivolumab had an ECOG PS of 0 or 1; patients with autoimmune disease, symptomatic interstitial lung disease, or those receiving systemic immunosuppression were excluded from enrollment.
-
A randomized, open-label, phase III trial randomly assigned 272 advanced squamous cell NSCLC patients who had received one regimen of platinum-containing chemotherapy to receive either nivolumab (3 mg/kg every 2 weeks) or docetaxel (75 mg/m2 every 3 weeks), administered until disease progression.[37] The primary endpoint of this study was OS.
-
Nivolumab demonstrated a significant improvement in median OS compared with docetaxel (9.2 months vs. 6 months; P < .001). In addition, the ORR (20% vs. 9%; P = .008) and median PFS (3.5 months vs. 2.8 months; P < .001) favored nivolumab.
-
Rates of treatment-related toxicity were significantly lower with nivolumab than with docetaxel (all grades, 58% for nivolumab vs. 86% for docetaxel; grades 3–4, 7% for nivolumab vs. 55% for docetaxel).
-
-
A randomized, open-label, phase III trial randomly assigned 582 advanced nonsquamous NSCLC patients who had received one regimen of platinum-containing chemotherapy to receive either nivolumab (3 mg/kg every 2 weeks) or docetaxel (75 mg/m2 every 3 weeks), administered until disease progression.[38] Previous maintenance chemotherapy after first-line platinum-doublet was allowed; patients with EGFR mutations or ALK translocations were allowed to have received an additional regimen of therapy with a TKI. The primary endpoint of this study was OS.
-
Nivolumab demonstrated a significant improvement in patients in median OS compared with docetaxel (12.2 months vs. 9.4 months; HR, 0.73; 96% CI, 0.59–0.89; P = .002). In this study, ORR (19% vs. 12%; P = .02) but not median PFS (2.3 months for nivolumab vs. 4.2 months for docetaxel) favored nivolumab. The median DOR in patients was 17.2 months for nivolumab and 5.6 months for docetaxel.
-
Rates of treatment-related toxicity were significantly lower with nivolumab than with docetaxel (all grades, 69% for nivolumab vs. 88% for docetaxel; grades 3–4, 10% for nivolumab vs. 54% for docetaxel).
-
-
Both of these trials demonstrated long-term clinical benefit at the 2-year outcomes. The OS rates for nivolumab at 2 years compared with docetaxel in squamous NSCLC were 23% (95% CI, 16–30) versus 8% (95% CI, 4–13), and OS rates in nonsquamous NSCLC were 29% (95% CI, 24–34) versus 16% (95% CI, 12–20).[40] Ongoing responses at 2 years were observed in 10 (37%) confirmed responders with squamous NSCLC and 19 (34%) of 56 responders with nonsquamous NSCLC. No patient treated with docetaxel in either study had an ongoing response.
-
Nivolumab is now considered a standard second-line therapy for patients with metastatic NSCLC with progression on or after first-line platinum-based chemotherapy and is associated with improved survival and lower rates of toxicity than docetaxel. However, clinical trials of nivolumab to date have not enrolled patients with a history of autoimmune disease, interstitial lung disease, or an ECOG PS higher than 1. Patients with active autoimmune conditions cannot be treated with nivolumab. Closely monitoring all patients for autoimmune toxicities from treatment is required. Specific algorithms for the management of autoimmune toxicity are included in the FDA label for nivolumab.
Pembrolizumab
Evidence (pembrolizumab):
-
In a phase I study with multiple expansion cohorts, pembrolizumab demonstrated significant activity with respect to response rate and DOR.[39][Level of evidence: 3iiiDiv]
-
In the study, 495 patients received either pembrolizumab 2 mg/kg every 3 weeks, 10 mg/kg every 3 weeks, or 10 mg/kg every 2 weeks. No significant differences were seen among the different treatment schedules. Key exclusion criteria were autoimmune disease, history of pneumonitis, requirement for systemic immunosuppressive therapy, and a PS higher than 1. The ORR was 19.4% (95% CI, 16.0–23.2), which included a response rate of 18.0% (95% CI, 14.4–22.2) in 394 previously treated patients and 24.8% (95% CI, 16.7–34.3) in 101 previously untreated patients. Median PFS was 3.7 months (95% CI, 2.9–4.1) for all patients, 3.0 months (95% CI, 2.2–4.0) for previously treated patients, and 6.0 months (95% CI, 4.1–8.6) for previously untreated patients. The median DOR was 12.5 months (range, 1.0–23.3 months) in all patients.
-
The study evaluated the efficacy of pembrolizumab in patients with high levels of PD-L1, as assessed by the anti-PD-L1 antibody clone 22C3. Using the cutoff of membranous staining in at least 50% of tumor cells in a validation group of 73 patients, the response rate was 45.2% (95% CI, 33.5–57.3), and the median PFS in this group was 6.3 months (95% CI, 2.9–12.5). Median OS was not reached at the time of publication.
-
The estimated prevalence of PD-L1 tumor staining from 1,143 screened patients, of whom 824 had evaluable samples, is as follows: 23.2% had 50% or more tumor cells with staining; 37.6% had between 1% and 49% tumor cells with staining; and 39.2% had less than 1% of tumor cells with staining.
-
The most common adverse events were fatigue, pruritus, and decreased appetite. Grade 3 or higher adverse events were reported in 9.5% of patients. Inflammatory and immune-mediated adverse events that occurred in more than 2% of patients were infusion-related reactions (3.0%), hypothyroidism (6.9%), and pneumonitis (3.6%).
-
-
In a phase II/III randomized clinical trial, patients with previously treated NSCLC with PD-L1 expression on at least 1% of tumor cells were randomly assigned (1:1:1) to receive pembrolizumab (2 mg/kg), pembrolizumab (10 mg/kg), or docetaxel (75 mg/m2) every 3 weeks.[41][Level of evidence: 1iiA] The primary endpoints were OS and PFS in the total population and in patients with PD-L1 expression on at least 50% of tumor cells. This study enrolled 1,034 patients; 345 of them were allocated to pembrolizumab (2 mg/kg); 346 were allocated to pembrolizumab (10 mg/kg); and 343 were allocated to docetaxel.
-
In the total population, median OS was 10.4 months with pembrolizumab (2 mg/kg), 12.7 months with pembrolizumab (10 mg/kg), and 8.5 months with docetaxel. OS was significantly longer for pembrolizumab (2 mg/kg) versus docetaxel (HR 0.71; 95% CI, 0.58–0.88; P = .0008) and for pembrolizumab (10 mg/kg) versus docetaxel (HR, 0.61; CI, 0.49–0.75; P < .0001).
-
In the total population, PFS was not prolonged in the pembrolizumab groups compared with the docetaxel group.
-
Among patients with at least 50% of tumor cells expressing PD-L1, OS was significantly longer with pembrolizumab (2 mg/kg) than with docetaxel (median, 14.9 months vs. 8.2 months; HR, 0.54; 95% CI, 0.38–0.77; P = .0002) and with pembrolizumab (10 mg/kg) than with docetaxel (median, 17.3 months vs. 8.2 months; HR, 0.50; CI, 0.36–0.70; P < .0001).
-
In the group of patients with at least 50% of tumor cells expressing PD-L1, PFS was significantly longer with pembrolizumab (2 mg/kg) than with docetaxel (median, 5.0 months vs. 4.1 months; HR, 0.59; 95% CI, 0.44–0.78; P = .0001) and with pembrolizumab (10 mg/kg) than with docetaxel (median, 5.2 months vs. 4.1 months; HR, 0.59; CI, 0.45–0.78; P < .0001).
-
Grade 3 to 5 treatment-related adverse events were less common with pembrolizumab than with docetaxel (43 [13%] of 339 patients given pembrolizumab (2 mg/kg), 55 [16%] of 343 patients given pembrolizumab (10 mg/kg), and 109 [35%] of 309 patients given docetaxel).
-
Pembrolizumab received accelerated approval as a second-line therapy for patients with NSCLC whose tumors express PD-L1 (>50% staining as determined by an FDA-approved test) with progression on or after first-line chemotherapy. Patients with EGFR or ALK genomic tumor aberrations should have disease progression on FDA-approved therapies before receiving pembrolizumab (refer to the FDA label for pembrolizumab).
Atezolizumab
Evidence (atezolizumab):
-
Two international, randomized, open-label clinical trials (OAK [NCT02008227] and POPLAR[NCT01903993]) demonstrated efficacy and safety in a total of 1,137 patients with NSCLC who previously received platinum chemotherapy.[42,43][Level of evidence: 1iiA] Compared with docetaxel, treatment with atezolizumab in the intended patient population resulted in improved OS rates of 4.2 months in the OAK study and 2.9 months in the POPLAR study.
-
In the OAK trial, the median OS was 13.8 months in the atezolizumab arm (95% CI, 11.8–15.7) compared with 9.6 months in the docetaxel arm (95% CI, 8.6–11.2) (HR = 0.74; 95% CI, 0.63–0.87; P = .0004).
-
The median OS in the POPLAR trial was 12.6 months in the atezolizumab arm (95% CI, 9.7–16.0) and 9.7 months in the docetaxel arm (95% CI, 8.6–12.0) (HR, 0.69; 95% CI, 0.52–0.92).
-
Although the magnitude of improvement correlated with PD-L1 immunohistochemistry expression on tumor cells and tumor-infiltrating immune cells, survival benefit with atezolizumab was seen in patients with tumors with and without PD-L1 expression.
-
In the POPLAR trial, the most common (≥20%) adverse reactions were in patients treated with atezolizumab and included fatigue, decreased appetite, dyspnea, cough, nausea, musculoskeletal pain, and constipation.
-
The most common (≥2%) grade 3 to 4 adverse events in patients treated with atezolizumab were dyspnea, pneumonia, hypoxia, hyponatremia, fatigue, anemia, musculoskeletal pain, aspartate aminotransferase increase, alanine aminotransferase increase, dysphagia, and arthralgia.
-
Clinically significant immune-related adverse events for patients receiving atezolizumab included pneumonitis, hepatitis, colitis, and thyroid disease.
-
Treatment Options under Clinical Evaluation for Progressive Stage IV, Relapsed, and Recurrent NSCLC (Second-line Therapy)
Treatment options under clinical evaluation for progressive stage IV, relapsed, and recurrent NSCLC (second-line therapy) include the following:
-
Clinical trials can be considered as second-line therapy.
Current Clinical Trials
Use our advanced clinical trial search to find NCI-supported cancer clinical trials that are now enrolling patients. The search can be narrowed by location of the trial, type of treatment, name of the drug, and other criteria. General information about clinical trials is also available.
![]()
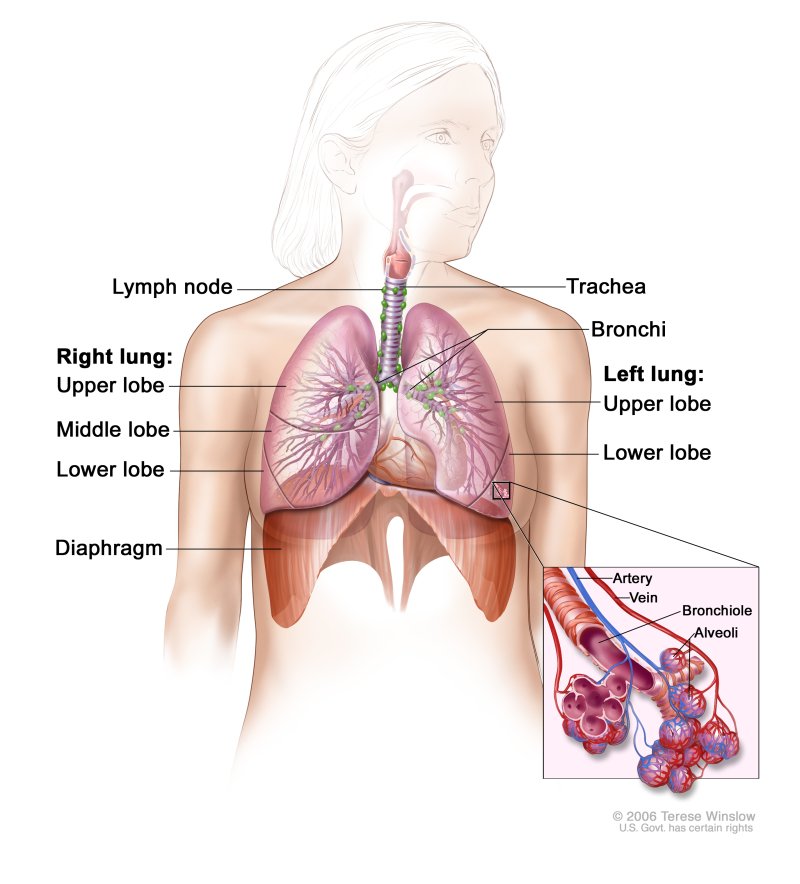






About the author