L2-3 Disc Disorders/PLID (Prolapse lumbar intervertebral disc) is one of the most common vertebral column diseases of elderly people leading to back pain, radicular pain, and subsequently neurological deficit due to nerve root compression. It is a common condition that frequently affects the spine in young and middle-aged patients.[rx,rx,rx] The lumbar intervertebral disc is a complex structure composed of collagen, proteoglycans, and sparse fibrochondrocytic cells that serve to dissipate forces exerted on the spine. As part of the normal aging process, the disc fibrochondrocytes can undergo senescence, and proteoglycan production diminishes. This leads to a loss of hydration and disc collapse, which increases strain on the fibers of the annulus fibrosus surrounding the disc. Tears and fissures in the annulus can result, facilitating a herniation of disc material, should sufficient forces be placed on the disc. Alternatively, a large biomechanical force placed on a healthy, normal disc may lead to extrusion of disc material in the setting of the catastrophic failure of the annular fibers.[Rx]
PLID (Prolapse lumbar intervertebral disc), also known as a slipped disc, is a medical condivertibral dissection affecting the spine in which a tear in the outer, fibrous ring of an intervertebral disallows the soft, central portion to bulge out beyond the damaged outer rings. Rarely bowel or bladder control is lost, and if this occurs, seek medical attention at once. A common cause of lower back and leg pain is a lumbar ruptured disc or herniated disc. Symptoms of a herniated disc may include dull or sharp pain, muscle spasm or cramping, sciatica, and leg weakness or loss of leg function. Sneezing, coughing, or bending usually intensify the pain.
Sciatica is a symptom frequently associated with a lumbar herniated disc. Pressure on one or several nerves that contribute to the sciatic nerve can cause pain, burning, tingling, and numbness that extends from the buttock into the leg and sometimes into the foot. Usually, one side (left or right) is affected.
Anatomy of PLID/L2-3 Disc Disorders
- First, a brief overview of spinal anatomy so that you can better understand how a lumbar herniated disc can cause lower back pain and leg pain.
- In between each of the 5 lumbar vertebrae (bones) is a disc—a tough fibrous shock-absorbing pad. Endplates line the ends of each vertebra and help hold individual discs in place. Every disc has a tire-like outer band (annulus fibrosus) that encases a gel-like substance (nucleus pulposus).
- Disc herniation occurs when the annulus fibrous breaks open or cracks, allowing the nucleus pulposus to escape. This is called a herniated nucleus pulposus or herniated disc, although you may have also heard it called a ruptured disc or a bulging disc.
- When a disc herniates, it can press on the spinal cord or spinal nerves. All along your spine, nerves are branching off from the spinal cord and traveling to various parts of your body (to help you feel and move). The nerves pass through small passageways between the vertebrae and discs, so if a herniated disc presses into that passageway, it can compress (or “pinch”) the nerve. That can lead to the pain associated with herniated discs.
(In the illustration below, you can see a close-up look at a herniated disc pressing on a spinal nerve.)

www.rxharun.com/causes-a-disc-to-bulge
This article on lumbar herniated discs will cover the symptoms, causes, and (most importantly) treatments.
Anatomy of Spine/L2-3 Disc Disorders
Complete intervertebral disc anatomy and biomechanics
Disc composition
Annulus fibrosis
- Composed of type I collagen, water, and proteoglycans
- Characterized by extensibility and tensile strength
- High collagen / low proteoglycan ratio (low % dry weight of proteoglycans)
Nucleus pulposus
- Composed of type II collagen, water, and proteoglycans
- Characterized by compressibility
- Low collagen / high proteoglycan ratio (high % dry weight of proteoglycans)
- Proteoglycans interact with water and resist compression
- A hydrated gel due to high polysaccharide content and high water content (88%)
Nerve Root Anatomy of PLID/L2-3 Disc Disorders
The key difference between the cervical and lumbar spine is
Pedicle/nerve root mismatch
- Cervical spine C6 nerve root travels under C5 pedicle (mismatch)
- Lumbar spine L5 nerve root travels under L5 pedicle (match)
- Extra C8 nerve root (no C8 pedicle) allows the transition
Horizontal (cervical) vs. vertical (lumbar) anatomy of nerve root
- Because of the vertical anatomy of the lumbar nerve root, a paracentral and foraminal disc will affect different nerve roots
- Because of horizontal anatomy of the cervical nerve root, a central and foraminal disc will affect the same nerve root
Location Classification
Central Prolapse
- Often associated with back pain only
- May present with cauda equina syndrome which is a surgical emergency
Posterolateral (paracentral)
- Most common (90-95%)
- PLL is weakest here
- Affects the traversing/descending/lower nerve root
- At L4/5 affects L5 nerve root
Foraminal (far lateral, extraforaminal)
- Less common (5-10%)
- Affects exiting/upper nerve root
- At L4/5 affects the L4 nerve root
Axillary
- Can affect both exiting and descending nerve roots
Anatomic classification
- Protrusion > eccentric bulging with an intact annulus
- Extrusion > disc material herniates through annulus but remains continuous with disc space sequestered fragment (free)disc material herniates through the annulus and is no longer continuous with disc space. Axial back pain (low back pain)
- This may be discogenic or mechanical in nature
Radicular pain (buttock and leg pain)
- Often worse with sitting, improves with standing
- Symptoms worsened by coughing, Valsalva, sneezing
Cauda equina syndrome (present in 1-10%)
- bilateral leg pain
- LE weakness
- saddle anesthesia
- bowel/bladder symptoms
Physical exam
- See lower extremity neuro exam
- Motor exam
- Ankle dorsiflexion (L4 or L5)
- Test by having the patient walk on heels
- EHL weakness (L5)
- Manual testing
- Hip abduction weakness (L5)
- Have the patient lie on the side on the exam table and abduct leg against resistance
- Ankle plantarflexion (S1)
- Have the patient do 10 single leg toes stand
Types of PLID/L2-3 Disc Disorders
According to the position of spine disc herniation are 3 types
Herniation may develop suddenly or gradually over weeks or months. The 4 stages to a herniated disc are:
- 1) Disc Degeneration or Bulsing Disc – Chemical changes associated with aging causes discs to weaken, but without a herniation.
- 2) Prolapse – The form or position of the disc changes with some slight impingement into the spinal canal and/or spinal nerves. This stage is also called a bulging disc or a protruding disc.
- 3) Extrusion – The gel-like nucleus pulposus breaks through the tire-like wall (annulus fibrosus) but remains within the disc.
- 4) Sequestration or Sequestered Disc – The nucleus pulposus breaks through the annulus fibrosus and can then go outside the intervertebral disc.
Causes of PLID/L2-3 Disc Disorders
- Piriformis syndrome – This develops when the piriformis muscle, a small muscle that lies deep in the buttocks, becomes tight or spasms, which can put pressure on and irritate the sciatic nerve & causes PLID.
- Spinal stenosis – This condition results from the narrowing of the spinal canal with pressure on the nerves.
- Spondylolisthesis – This is a slippage of one vertebra so that it is out of line with the one above it, narrowing the opening through which the nerve exits.
- Cauda equina syndrome – A rare but serious condition that affects the nerves in the lower part of the spinal cord; it requires immediate medical attention. Cauda equina syndrome may permanently damage the nervous system and even lead to paralysis.
- Bony growths (osteophytes) – Osteophytes are bony lumps (bone spurs) that grow on the bones of the spine or around the joints. They often form next to joints affected by osteoarthritis, a condition that causes joints to become painful and stiff.

- Bone spurs – are bony outgrowths on the edges of joints. Bone spurs form where cartilage is worn away (for example in arthritis) and bone is rubbing on bone. In an effort to protect the body, new bone forms on the edge of joints. This is called a bone spur. Bone spurs are not painful in themselves, but unfortunately, the bone spurs can rub on nearby bone or nerves, causing problems. In the spine, bone spurs can intrude into space normally reserved for the nerves, thus causing sciatica.
- Sudden injury or accident – Some unexpected traumatic events, such as a car accident, can lead to sciatica. Injuries sustained and new scar tissue can place stress on the sciatic nerve.
- Pregnancy – During pregnancy, pain in the back of the thighs spurred by shifts in the pelvic region can be misdiagnosed as sciatica. However, there are situations in which the sciatic nerve is actually being pressed as a result of these changes. Speak to your doctor if you think you are suffering from sciatica or pelvic groin pain.
- Tumors – within the spine may compress the root of the sciatic nerve.
- Infection within the spine.
- Injury within the spine.
Associate causes of PLID/L4-5 Slip Disc Disorders
- Spinal lesions and tumors
- Spinal infections or inflammation
- Lumbar spinal stenosis
- Violent injuries to the lower back (gunshots, falls, auto accidents)
- Birth abnormalities
- Spinal arteriovenous malformations (AVMs)
- Spinal hemorrhages (subarachnoid, subdural, epidural)
- Postoperative lumbar spine surgery complications
- Spinal anesthesia
Degenerative
- lumbar disc herniation (most common, especially at L4/5 and L5/S1)
- lumbar spinal canal stenosis
- spondylolisthesis
- Tarlov cysts
- facet joint cysts
Trauma
- Traumatic events leading to fracture or partial dislocation (subluxation) of the low back (lumbar spine) result in compression of the sciatic nerve.
- Spinal fracture or dislocation
- Epidural hematoma (may also be spontaneous, post-operative, post-procedural or post-manipulation)
- A collection of blood surrounding the nerves following trauma (epidural hematoma) in the low back area can lead to compression of sciatica.
- Penetrating trauma (gunshot or stab wounds) can cause damage or compression of the sciatic nerve.
- A rare complication of spinal manipulation is a partial dislocation (subluxation) of the low back (lumbar spine) that can cause sciatica syndrome.
Herniated Disk
- Most disk herniations will improve on their own (are self-limiting) and respond well to conservative treatment, including anti-inflammatory medications, physical therapy, and short periods of rest (one to two days).
- Sciatica syndrome can result from a herniated lumbar disk.
- Of lumbar disk herniations, most occur either at the vertebral levels L4-L5 or L5-S1.
- Seventy percent of cases of herniated disks leading to sciatica syndrome occur in people with a history of chronic low back pain, and some develop sciatica syndrome as the first symptom of lumbar disk herniation.
- Males in their 30s and 40s are most prone to cauda equina syndrome caused by disk herniation.
- Most cases of sciatica syndrome caused by disk herniation involve large particles of disk material that have completely separated from the normal disk and compress the nerves (extruded disk herniations). In most cases, the disk material takes up at least one-third of the canal diameter.
Spinal Stenosis
- Spinal stenosis is any narrowing of the normal front to back distance (diameter) of the spinal canal.
- Narrowing of the spinal canal can be caused by a developmental abnormality or degenerative process.
- The abnormal forward slip of one vertebral body on another is called spondylolisthesis. Severe cases can cause a narrowing of the spinal canal and lead to sciatica syndrome
Tumors (Neoplasms)
Sciatica syndrome can be caused by isolated tumors (primary neoplasms) or from tumors that have spread to the spine from other parts of the body (metastatic spinal neoplasms). Metastatic spine tumors are most commonly from the prostate or lung in males and from the lung and breast in females.
- Malignant – lymphoma, metastases, primary CNS malignancies(e.g. ependymoma, schwannoma, neurofibroma)
- The most common initial symptom of people with cauda equina syndrome caused by a tumor (spinal neoplasm) is severe low back and leg pain.
- Later findings include lower extremity weakness.
- Loss of feeling in the legs (sensory loss) and loss of bowel or bladder control (sphincter dysfunction) are also common.
Inflammatory Conditions
- Both acute and chronic form may be seen in long-standing ankylosing spondylitis (2nd-5th decades; average 35 years)
- Long-lasting inflammatory conditions of the spine, including Paget disease and ankylosing spondylitis, can cause a narrowing of the spinal canal and lead to sciatica syndrome.
Infectious Conditions
- Infections in the spinal canal (spinal epidural abscess) can cause deformity of the nerve roots and spinal column.
- Symptoms generally include severe back pain and rapidly worsening muscle weakness.
- Infective – epidural abscess, tuberculosis (Pott disease)
Accidental Medical Causes (Iatrogenic Causes)
- Poorly positioned screws placed in the spine can compress and injure nerves and cause sciatica syndrome.
- Continuous spinal anesthesia has been linked to cases of sciatica syndrome.
- Lumbar puncture (spinal tap) can cause a collection of blood in the spinal canal (spontaneous spinal epidural hematoma) in patients receiving medication to thin the blood (anticoagulation therapy). This collection of blood can compress the nerves and cause sciatica syndrome.
- Aortic dissection
- Arteriovenous malformation
Symptoms of PLID/L2-3 Disc Disorders
- Weakness in the Legs – The weakness is often times asymmetric.
- Loss of Sensation – Those affected may experience numbness or tingling in their perineum
- Loss of Reflexes – A person’s knee and ankle reflexes might be diminished, along with anal and bulbocavernosus abilities.
- Sensory Loss – Sensory loss may range from, ‘pins and needles,‘ to complete numbness. It might affect a person’s bowel, bladder and genitalia Bladder, Bowel and
Associate clinical feature is
- Severe back pain
- Saddle anesthesia i.e., anesthesia or paraesthesia involving S3 to S5 dermatomes, including the perineum, external genitalia, and anus; or more descriptively, numbness or “pins-and-needles” sensations of the groin and inner thighs which would contact a saddle when riding a horse.
- Bladder and bowel dysfunction, caused by a decreased tone of the urinary and anal sphincters.
- Detrusor weaknesses causing urinary retention and post-void residual incontinence as assessed by bladder scanning the patient after the patient has urinated.
- Sciatica type pain on one side or both sides, although pain may be wholly absent
- The weakness of the muscles of the lower legs (often paraplegia)
- Pain in one leg (unilateral) or both legs (bilateral) that starts in the buttocks and travels down the back of the thighs and legs (sciatica)
- Numbness in the groin or area of contact if sitting on a saddle (perineal or saddle paresthesia)
- Bowel and bladder disturbances
- Lower extremity muscle weakness and loss of sensations
- Inability to urinate (urinary retention)
- Difficulty initiating urination (urinary hesitancy)
- The decreased sensation when urinating (decreased urethral sensation)
- Inability to stop or control urination (incontinence)
- Reduced or absent lower extremity reflexes
- Local pain is generally a deep, aching pain resulting from soft tissue and vertebral body irritation.
- Leg pain (radicular pain) is generally a sharp, stabbing pain resulting from compression of the nerve roots.
- Radicular pain projects along the specific areas controlled by the compressed nerve (known as a dermatomal distribution).
- Inability to stop or feel a bowel movement (incontinence)
- Constipation
- Loss of anal tone and sensation
- Achilles (ankle) reflex absent on both sides.
- Sexual dysfunction
- Absent anal reflex and bulbocavernosus reflex
- Gait disturbance
Diagnosis of PLId/L2-3 Disc Disorders
Straight Leg Raise
- A tension sign for L5 and S1 nerve root
- Can be done sitting or supine
- Reproduces pain and paresthesia in the leg at 30-70 degrees hip flexion
- Sensitivity/specificity most important and predictive physical finding for identifying who is a good candidate for surgery
Contralateral SLR
- Crossed straight leg raise is less sensitive but more specific
League sign
- SLR aggravated by forced ankle dorsiflexion
Bowstring sign
- SLR aggravated by compression on the popliteal fossa
Kernig test
- Pain reproduced with neck flexion, hip flexion, and leg extension
Naffziger test
- Pain reproduced by coughing, which is instigated by lying patient supine and applying pressure on the neck veinsMilgram test
- Pain reproduced with straight leg elevation for 30 seconds in the supine position
- Gait analysis
- Trendelenburg gait due to gluteus medius weakness which is innervated by L5.
Physical Examination of PLID/L2-3 Disc Disorders
Observation of posture and function
- In standing her shoulders – were shunted to the left side, her back was extended and pelvis anteriorly tilted, and there was visible hyper-tonicity of the lumbar paraspinal muscles.
- This shunted antalgic posture – is commonly referred to as a lumber list. Observation of a lumber list, unfortunately, is a test lacking in reliability (Clare, Adams, & Maher, 2003). Maitland (2005), however, teaches us that if a person presents with an observable postural deformity, they are going to be more challenging to get better. In Sally’s case, she had a contralateral list (shoulders listed to the opposite side of back/leg pain), which is thought to respond more favorably to treatment than an ipsilateral list.
- In my experience antalgic postures – are very important to detect because they indicate a protective position; a mechanism which the body is adopting (often subconsciously) in the acute phase of injury to protect the injury, and if the antalgic posture is not carefully examined and carefully corrected, it can make the patient a lot worse.
Active range of movement
- Lumbar flexion P2 (right-sided low back pain) R`(upper thigh).
- Extension P2 (right buttock and leg pain) R` (vertical).
- Other movements were not assessed day 1 due to severity and irritability.
Neurological examination
- Weak single leg calf raises (SLCR) and was only able to perform three assisted raises to 50% range. Gr 5 strength of right leg SLCR x5 repetitions.
- No other myotomal weakness was detected.
- The S1 reflex on the right side was absent, with other lower limb reflexes being preserved.
- No sensory changes were noted.
Neurodynamic Examination
- The straight leg raise test (SLR) was positive in reproducing Sally’s posterior thigh pain and limited at 20 degrees on the right side.
- Her left SLR was limited by hamstring tightness at 50 degrees.

The research suggests the SLR reliable re-assessment asterisks for patient progress. It has been shown to be 91% sensitivity and 26% specificity in detecting lumbar disc pathology.D Neville et al. (2012) found that more than an 11-degree discrepancy in hip flexion range between sides was a clinically significant result. Compared to MRI, the SLR test has poor diagnostic accuracy and therefore is often used in conjunction with such imaging.
[stextbox id=’info’]
Location of Pain and Motor Deficits in Association with Nerve Root Involvement at Each Lumbar Disc Level
| DISC LEVEL | LOCATION OF PAIN | MOTOR DEFICIT |
|---|---|---|
|
T12-L1 |
Pain in the inguinal region and medial thigh |
None |
|
L1-2 |
Pain in the anterior and medial aspect of the upper thigh |
Slight weakness in quadriceps; slightly diminished suprapatellar reflex |
|
L2-3 |
Pain in the anterolateral thigh |
Weakened quadriceps; diminished patellar or suprapatellar reflex |
|
L3-4 |
Pain in the posterolateral thigh and anterior tibial area |
Weakened quadriceps; diminished patellar reflex |
|
L4-5 |
Pain in the dorsum of the foot |
Extensor weakness of big toe and foot |
|
L5-S1 |
Pain in the lateral aspect of the foot |
Diminished or absent Achilles reflex |
[/stextbox]
- Palpation was conducted on the left side-lying position with pressure applied only to the onset of pain (P1).
- The presence of generalized hyperalgesia made it difficult to establish a comparable finding day.
Straight Leg Raise Test (SLR Test)
| Straight leg raise | |
|---|---|
| Medical diagnostics | |

Straight Leg test sometimes used to help diagnose a lumbar herniated disc
|
SLR test and its Modifications
| SLR (BASIC) | SLR2 | SLR3 | SLR4 | CROSS LEG
SLR 5 |
|
|---|---|---|---|---|---|
| HIP | Flexion and adduction | Flexion | Flexion | Flexion and Medial Rotation | Flexion |
| KNEE | Extension | Extension | Extension | Extension | Extension |
| ANKLE | Dorsiflexion | Dorsiflexion | Dorsiflexion | Plantar flexion | Dorsiflexion |
| FOOT | —— | Eversion | Inversion | Inversion | ——- |
| TOES | —— | Extension | —– | —— | —— |
| NERVE BIAS | Sciatic Nerve and Tibial Nerve | Tibial Nerve | Sural Nerve | Common Peroneal Nerve | Nerve Root (Disc Prolapse) |
Evidence
- A Cross-sectional study by Boyd and Villa (2012) examined normal asymmetries between limbs in healthy, asymptomatic individuals during SLR testing and the relationship of various demographic characteristics. The authors concluded that the overall range of motion during SLR was related to sex, weight, BMI and activity level, which is likely reflected in the high variability documented.
- We can be 95% confident that inter-limb differences during SLR neurodynamic testing fall below 11 degrees in 90% of the general population of healthy individuals. In addition, inter-limb differences were not affected by demographic factors and thus may be a more valuable comparison for test interpretation.
- Rabin et al. have shown the sensitivity of the SLR test to be.
- Deville et al. found the specificity to be.
- A systematic review of the Clinical utility of SLR by Scaia V, Baxter D and Cook C (2012) investigated the diagnostic accuracy of a finding of pain during the straight leg raise test for lumbar disc herniation, lumbar radiculopathy, and/or sciatica.
- The authors concluded that Variability in reference standard may partly explain the inconsistencies in the diagnostic accuracy findings.
- Further, pain that is not specific to lumbar radiculopathies, such as that associated with hamstring tightness, may also lead to false positives for the SLR; and may inflate the sensitivity of the test.
Diagnostic Test Accuracy Review (Cochrane Meta-analysis)-
Assessed the performance of tests performed during physical examination (alone or in combination) to identify radiculopathy due to lower lumbar disc herniation in patients with low-back pain and sciatica. The review included 16 cohort studies (median N = 126, range 71 to 2504) and three case-control studies (38 to100 cases). Only one study was carried out in a primary care population. Most studies assessed the Straight Leg Raising (SLR) test. In surgical populations, characterized by a high prevalence of disc herniation (58% to 98%), the SLR showed high sensitivity (pooled estimate 0.92, 95% CI: 0.87 to 0.95) with widely varying specificity (0.10 to 1.00, pooled estimate 0.28, 95% CI: 0.18 to 0.40). Results of studies using imaging showed more heterogeneity and poorer sensitivity. The crossed SLR showed high specificity (pooled estimate 0.90, 95% CI: 0.85 to 0.94) with consistently low sensitivity (pooled estimate 0.28, 95% CI: 0.22 to 0.35). Combining positive test results increased the specificity of physical tests, but few studies presented data on test combinations. The authors of the meta-analysis conclude that When used in isolation, current evidence indicates the poor diagnostic performance of most physical tests used to identify lumbar disc herniation. However, most findings arise from surgical populations and may not apply to primary care or non-selected populations. Better performance may be obtained when tests are combined.
Symptoms of lumbar disk disease/L2-3 Disc Disorders

The symptoms of lumbar disk disease vary depending on where the disk has herniated, and what nerve root it is pushing on. The following are the most common symptoms of lumbar disk disease. However, each individual may experience different symptoms. Symptoms may include:
- Intermittent or continuous back pain. This may be made worse by movement, coughing, sneezing, or standing for long periods of time.
- Spasm of the back muscles
- Sciatica. Pain that starts near the back or buttock and travels down the leg to the calf or into the foot.
- Muscle weakness in the legs
- Numbness in the leg or foot
- Decreased reflexes at the knee or ankle
- Changes in bladder or bowel function
The symptoms of lumbar disk disease may resemble other conditions or medical problems. Always consult your health care provider for a diagnosis.
Lab Diagnosis of PLID/L2-3 Disc Disorders
A doctor can diagnose cauda low back pain. Here’s what you may need to confirm a diagnosis
- A medical history – in which you answer questions about your health, symptoms, and activity.
- A physical exam to assess your strength – reflexes, sensation, stability, alignment, and motion. You may also need blood tests.
- Laboratory testing – may include white blood cell (WBC) count, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP).
- Elevated ESR – could indicate infection, malignancy, chronic disease, inflammation, trauma, or tissue ischemia.
- Elevated CRP – levels are associated with infection.
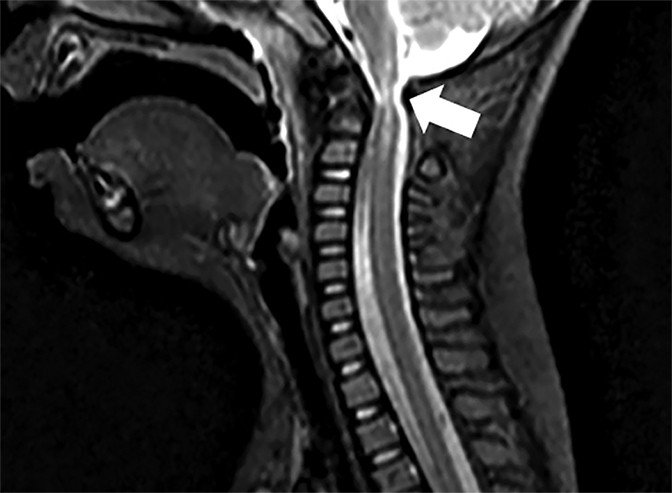
- Magnetic resonance imaging (MRI) scan – which uses magnetic fields and computers to produce three-dimensional images of your spine.
- A myelogram – an X-ray of the spinal canal after injection of contrast material — which can pinpoint pressure on the spinal cord or nerves.
- A computed tomography (CT) scan.
- Urodynamic studies – may be required to monitor the recovery of bladder function following decompression surgery.
- In most cases of low back pain, medical consensus advises not seeking an exact diagnosis but instead beginning to treat the pain. This assumes that there is no reason to expect that the person has an underlying problem. In most cases, the pain goes away naturally after a few weeks. Typically, people who do seek diagnosis through imaging are not likely to have a better outcome than those who wait for the condition to resolve.
Treatment of PLID/L2-3 Disc Disorders
Non-surgical
Rest – It is important that the patient take proper rest and sleep and avoid any activities which will further aggravate the disc bulge and its symptoms. Many minor disc bulges can heal on their own with rest and other conservative treatment.
Cervical Pillow – It is important to use the right pillow to give your neck the right type of support for healing from a cervical disc bulge and also to improve the quality of sleep.
Specific treatment for lumbar disk disease will be determined by your health care provider based on
- Your age, overall health, and medical history
- The extent of the condition
- Type of condition
- Your tolerance for specific medications, procedures, or therapies
- Expectations for the course of the condition
- Your opinion or preference
Typically, conservative therapy is the first line of treatment to manage lumbar disk disease. Approach for Treating and Reversing a Disc Bulge about half of the disc bulges heal within six months and only about 10% of the disc bulges require surgery. So, the good news is that conservative treatment for a disc bulge helps in treating as well as reversing the disc bulges.
Ice & Moist Heat Application

Ice application where the ice is wrapped in a towel or an ice pack for about 20 minutes to the affected region, thrice a day, helps in relieving the symptoms of a disc bulge. Heat application in the later stages of treatment also provides the same benefit.
Hot Bath – Taking a hot bath or shower also helps in dulling the pain from a disc bulge. Epsom salts or essential oils can be added to a hot bath. They will help in soothing the inflamed region.
Traction

- Massage therapy – may give short-term pain relief, but not functional improvement, for those with acute lower back pain. It may also give short-term pain relief and functional improvement for those with long-term (chronic) and sub-acute lower back pain, but this benefit does not appear to be sustained after 6 months of treatment. There does not appear to be any serious adverse effects associated with massage.
- Acupuncture – may provide some relief for back pain. However, further research with stronger evidence needs to be done.
- Spinal manipulation – is a widely-used method of treating back pain, although there is no evidence of long-term benefits.
- Back school – is an intervention that consists of both education and physical exercises. A 2016 Cochrane review found the evidence concerning back school to be very low quality and was not able to make generalizations as to whether the back school is effective or not.
- Patient education – on proper body mechanics (to help decrease the chance of worsening pain or damage to the disk)
- Physical therapy – which may include ultrasound, massage, conditioning, and exercise
- Over the Door Traction – This is a very effective treatment for a disc bulge. It helps in relieving muscle spasms and pain. Typically a 5 to 10-pound weight is used and it is important that patient do this under medical guidance.
- Weight control
- Use of a lumbosacral back support
- Typically – conservative therapy is the first line of treatment to manage lumbar disk disease. Approach for Treating and Reversing a Disc Bulge about half of the disc bulges heal within six months and only about 10% of the disc bulges require surgery. So, the good news is that conservative treatment for a disc bulge helps in treating as well as reversing the disc bulges.
Eat nutritiously during your recovery
All bones and tissues in the body need certain nutrients in order to heal properly and in a timely manner. Eating a nutritious and balanced diet that includes lots of minerals and vitamins are proven to help heal back pain of all types. Therefore focus on eating lots of fresh produce (fruits and veggies), whole grains, lean meats, and fish to give your body the building blocks needed to properly healing PLID. In addition, drink plenty of purified water, milk, and other dairy-based beverages to augment what you eat.
- PLID needs ample minerals (calcium, phosphorus, magnesium, boron) and protein to become strong and healthy again.
- Excellent sources of minerals/protein include dairy products, tofu, beans, broccoli, nuts and seeds, sardines and salmon.
- Important vitamins that are needed for bone healing include vitamin C (needed to make collagen), vitamin D (crucial for mineral absorption), and vitamin K (binds calcium to bones and triggers collagen formation).
- Conversely, don’t consume food or drink that is known to impair bone/tissue healing, such as alcoholic beverages, sodas, most fast food items and foods made with lots of refined sugars and preservatives.
[stextbox id=’info’]
Medications
- Analgesics – Prescription-strength drugs that relieve pain but not inflammation.
- Muscle Relaxants – These medications provide relief from spinal muscle spasms.
- Neuropathic Agents – Drugs(pregabalin & gabapentin) that address neuropathic—or nerve-related—pain. This includes burning, numbness, and tingling.
- Opioids – Also known as narcotics, these medications are intense pain relievers that should only be used under a doctor’s careful supervision.
- Topical Medications – These prescription-strength creams, gels, ointments, patches, and sprays help relieve pain and inflammation through the skin.
- NSAIDs – Prescription-strength drugs that reduce both pain and inflammation. Pain medicines and anti-inflammatory drugs help to relieve pain and stiffness, allowing for increased mobility and exercise. There are many common over-the-counter medicines called non-steroidal anti-inflammatory drugs (NSAIDs). They include etodolac, aceclofenac, etoricoxib, ibuprofen, and naproxen.
- Topical Medications – These prescription-strength creams, gels, ointments, patches, and sprays help relieve pain and inflammation through the skin.
- Calcium & vitamin D3 – To improve bones health and healing fracture. As a general rule, men and women age 50 and older should consume 1,200 milligrams of calcium a day, and 600 international units of vitamin D a day.
- Glucosamine & Diacerein, Chondroitin sulfate – can be used to tightening the loose tendon, cartilage, ligament, and cartilage, ligament regenerates cartilage or inhabits the further degeneration of cartilage, ligament.
- Dietary supplement -to remove general weakness & improved health.
- Antidepressants – A drug that blocks pain messages from your brain and boosts the effects of endorphins (your body’s natural painkillers).
- Corticosteroid- to healing the nerve inflammation and clotted blood in the joints.
[/stextbox]
Surgical Treatment /L2-3 Disc Disorders
When these conservative measures fail, surgery for removal of a herniated disk may be recommended. Surgery is done under general anesthesia. An incision is placed in the lower back over the area where the disk is herniated. Some bone from the back of the spine may be removed to gain access to the area where the disk is located. Typically, the herniated part of the disk and any extra loose pieces of a disk are removed from the disk space.
Percutaneous Endoscopic Discectomy
With the increasing use of endoscopic surgical techniques in spinal surgery, PED was introduced to the treatment of pediatric LDH [Rx]. Two relevant articles published by Mayer et al. [Rx] (4 cases) and Lee et al (46 cases) were obtained from the literature search. PED was associated with a short-term success rate of 91.3 and 100% respectively, without complications such as leakage of CSF, nerve root injury, interspace infection, etc. The long-term follow-up is yet to be reported. Their recommended indications of PED for pediatric LDH include
- (1) failure of 6 weeks of conservative treatment;
- (2) a comparatively intact disc;
- (3) subligamentous protruded or extruded disc. The minimally invasive nature of PED means less surgical trauma and shorter hospital stay. Its success, however, requires a correct selection of patients and the surgeon being able to master the surgical procedure.
Open Discectomy
- Discectomy remains the most used surgical procedure for LDH in children and adolescents as well as in adults. It is generally agreed in the literature that posterior discectomy with partial laminotomy is indicated for posterolateral disc herniation, whereas hemilaminectomy or laminectomy is required in cases of central disc herniation. There were also reports of successful use of extraperitoneal anterolateral discectomy on centrally protruded disc [Rx].
- More recently, MD has also been used for the treatment of pediatric LDH [Rx] and associated with a good result. The present review found five published series with clinical outcome obtained from 143 MD cases. The short-term success rate ranged from 98 to 100% while the mid and long-term success rate dropped to 92 and 85% respectively.
- Surgical indications should be proposed if conservative treatment fails, or if the neurological symptoms progress.
- In such cases, microdiscectomy (under a magnifying glass or through a microscope) with preservation of the ligament flavum has been shown to be effective for preventing complications, avoiding peridural fibrosis and reducing symptomatic relapses.
Others Treatment/ L2-3 Disc Disorders
Intradiscal therapy
- Although there are various forms of intradiscal therapy available for adult LDH, similar reports on children and adolescents are comparatively sparse. According to the literature, chemonucleolysis was the only form of intradiscal therapy reported being used on children and adolescents.
- Although FDA approval for chymopapain use in humans has long been withdrawn, it is still being manufactured and in clinical use in Korea, Canada, Australia, UK and three states in the US [rx]. In comparison with surgery, chemonucleolysis is advantageous in that it is associated with less trauma and post-operative adhesion, shorter hospital stay, earlier remobilization, and lower cost.
Chiropractic Care
- Sixty percent of people with sciatica who didn’t get relief from other therapies and then tried spinal manipulation experienced the same degree of pain relief as patients who eventually had surgery, found a 2010 study in the Journal of Manipulative and Physiological Therapeutics.
- The 120 people in the study saw a chiropractor about 3 times a week for 4 weeks and then continued weekly visits, tapering off treatment as they felt better.
- In people who responded to chiropractic care, benefits lasted up to a year. “spinal manipulations may create a response in the nervous system that relieves pain and restores normal mobility to the injured area,” says study researcher Gordon McMorland, DC, of National Spine Care in Calgary, Alberta. “It also reduces inflammation, creating an environment that promotes the body’s natural healing mechanisms.
Acupuncture
- You can get relief as soon as the first session, though it takes about 12 sessions to see improvement,” says Jingduan Yang, MD, assistant professor at the Jefferson Myrna Brind Center of Integrative Medicine at Thomas Jefferson University. A small study in the Journal of Traditional Chinese Medicine found that of 30 people with sciatica, 17 got complete relief and 10 saw symptoms improve with warming acupuncture, in which the needles are heated.
Yoga
- A study in the journal Pain reported that people with chronic back pain who practiced Iyengar yoga for 16 weeks saw pain reduced by 64% and disability by 77%. Although yoga’s effects on sciatica are less clear, gentle forms may be beneficial. By strengthening muscles and improving flexibility, a yoga practice can help sciatica sufferers “move and function better so they don’t fall into a posture that aggravates sciatica.
 Massage
Massage
- Don’t expect a chilled-out spa massage if you have sciatica. In this instance, trigger-point therapy is best, says Jeff Smoot, vice president of the American Massage Therapy Association. The sciatic nerve sits underneath a muscle called the piriformis, which is located beneath the glutes.
- When the piriformis muscle gets tight, it pinches the sciatic nerve, causing tingling and numbness down into the leg,” says Smoot. He applies pressure to irritated and inflamed areas, or trigger points, in the piriformis muscle, as well as in muscles in the lower back and glutes. Typically, Smoot schedules treatments 7 to 10 days apart. If patients don’t see progress by the fourth visit, “they need to try another form of therapy,” he says.
Topical Preparations
- St. John’s wort oil, a liniment, is “one of my favorites for nerve pain,” says Tieraona Low Dog, MD, director of the fellowship at the Arizona Center for Integrative Medicine. Apply the anti-inflammatory oil two or three times a day where there’s a pain. Another option: an OTC cayenne pepper plaster or cream; capsaicin, found in chiles, hinders the release of pain-causing compounds from nerves. For severe cases, Low Dog uses the prescription chile patch Qutenza, designed for shingles pain. “One application is effective for weeks,” says Low Dog.
Ice or Heat
- Because the sciatic nerve is buried deep within the buttock and leg, ice or heat on the surface of the body won’t ease that inner inflammation. But the time-honored treatments can act as counterirritants—that is, “they give your body other input in the painful area, and that brings the pain down a notch,” says Ruppert. Apply an ice pack or a heating pad as needed for 15 minutes.
Devil’s Claw
- The herbal medication devil’s claw is “quite a potent anti-inflammatory, working like ibuprofen and similar drugs to inhibit substances that drive inflammation,” says Low Dog. She generally starts patients on 1,500 to 2,000 mg twice a day. Look for a brand that has a standardized extract of roughly 50 mg of harpagoside, the active compound. Safety reviews show that the supplement is well tolerated by most people but should be avoided by patients with peptic ulcers or on blood-thinning medications.
Epidural Steroid Injections

People whose pain doesn’t lessen within about a month and who aren’t helped by other therapies may find their pain remedied by an x-ray-guided injection of steroid into the lower back near the sciatic nerve, says Raj Rao, MD, a spokesperson for the AAOS. “The hope is to reduce inflammation within that nerve branch,” explains Rao. Because of concerns about side effects, such as loss of bone density, the epidural shots are limited to three a year.
Physiotherapy in PLID/L2-3 Disc Disorders
In stage 1&2 of PLID physiotherapy must be applied to cure PLID. In the case of stage 3&4, physiotherapy can’t apply due to avoiding another case of foot drop.
Physiotherapy for a lumbar disc bulge
Physical therapy often plays a major role in herniated disc recovery. Its methods not only offer immediate pain relief, but they also teach you how to condition your body to prevent further injury.
There are a variety of physical therapy techniques. Passive treatments relax your body and include deep tissue massage, hot and cold therapy, electrical stimulation (eg, TENS), and hydrotherapy.
Your physical therapy program will usually begin with passive treatments. But once your body heals, you will start active treatments that strengthen your body and prevent further pain. Your physical therapist will work with you to develop a plan that best suits you.
Passive Physical Treatments for Herniated Discs/L2-3 Disc Disorders

- Deep Tissue Massage – There are more than 100 types of massage, but a deep tissue massage is an ideal option if you have a herniated disc because it uses a great deal of pressure to relieve deep muscle tension and spasms, which develop to prevent muscle motion at the affected area.
- Hot and Cold Therapy – Both hot and cold therapies offer their own set of benefits, and your physical therapist may alternate between them to get the best results. Your physical therapist may use heat to increase blood flow to the target area. Blood helps heal the area by delivering extra oxygen and nutrients. Blood also removes waste byproducts from muscle spasms. Conversely, cold therapy (also called cryotherapy) slows circulation. This reduces inflammation, muscle spasms, and pain. Your physical therapist may place an ice pack on the target area, give you an ice massage, or even use a spray known as fluoromethane to cool inflamed tissues.
- Hydrotherapy – As the name suggests, hydrotherapy involves water. As a passive treatment, hydrotherapy may involve simply sitting in a whirlpool bath or warm shower. Hydrotherapy gently relieves pain and relaxes muscles.
- Transcutaneous electrical nerve stimulation (TENS): A TENS machine uses an electrical current to stimulate your muscles. It sounds intense, but it really isn’t painful. Electrodes taped to your skin send a tiny electrical current to key points on the nerve pathway. TENS reduces muscle spasms and is generally believed to trigger the release of endorphins, which are your body’s natural painkillers.
- Traction – The goal of traction is to reduce the effects of gravity on the spine. By gently pulling apart the bones, the intent is to reduce the disc herniation. The analogy is much like a flat tire “disappearing” when you put a jack under the car and take the pressure off the tire. It can be performed in the cervical or lumbar spine.
- Active Treatments You May Try in Physical Therapy – Active treatments help address flexibility, posture, strength, core stability, and joint movement. An exercise program may also be prescribed to achieve optimal results. This will not only curb recurrent pain but will also benefit your overall health. Your physical therapist will work with you to develop a program based on your specific diagnosis and health history.
- Core stability – Many people don’t realize how important a strong core is to their spinal health. Your core (abdominal) muscles help your back muscles support your spine. When your core muscles are weak, it puts extra pressure on your back muscles. Your physical therapist may teach you core stabilizing exercises to strengthen your back.
- Flexibility – Learning proper stretching and flexibility techniques will prepare you for aerobic and strength exercises. Flexibility helps your body move easier by warding off stiffness.
- Hydrotherapy – In contrast to simply sitting in a hot tub or bath like its passive counterpart, active hydrotherapy may involve water aerobics to help condition your body without unnecessary stress.
- Muscle-strengthening – Strong muscles are a great support system for your spine and better handle pain.

Your physical therapist will teach you ways to condition and strengthen your back to help prevent future pain. You may learn self-care principles so you understand how to best treat your symptoms. The ultimate goal is for you to develop the knowledge to maintain a pain-free lifestyle.
It’s essential that you learn how to exercise and condition your back after the formal physical therapy ends. If you don’t implement the lessons you learned during physical therapy, you won’t enjoy its long-term results. By taking care of your back on your own, you may prevent further herniated disc pain.
Reversal Treatment of PLID with Physical Therapy/L2-3 Disc Disorders
The patient’s posture, standing, and sitting positions are also examined. The soft tissues surrounding the spine are also examined to look for abnormal temperature, texture, and tenderness for detecting any irritation, inflammation and muscle spasms. Physical therapy combines therapeutic exercises, pain control techniques, massage therapy, and functional training practices, which help the patient by:
- Physical therapy helps in easing the disc bulge to revert back to its normal position and in alleviating the inflammation and pain.
- Physical therapy helps in increasing the blood circulation, oxygen, and nutrients to the spine.
- Physical therapy helps in gently pushing the disc bulge back into its normal position in the spinal canal thus tries to reverse the process of the disc bulge.
- Physical therapy strengthens the back and abdominal muscles, which provide enhanced support to the spine along with increasing spinal flexibility and strength.
- The stretching and strengthening exercises of physical therapy helps in improving the spinal range of motion, flexibility, and strength.
- Egoscue is a type of postural therapy, which is a series of gentle and targeted exercises that help in correcting musculoskeletal dysfunctions and other compensations which increase the risk of spinal injuries.
- Physical therapy also helps in strengthening the back muscles which helps in preventing future injuries.
- Physical therapy also helps in developing and maintaining a good posture.
Techniques of Physical Therapy for Treating and Reversing a Disc Bulge in PLID/L2-3 Disc Disorders
Some of the common physical therapy techniques for relieving and reversing a disc bulge consist of:
- Traction machine is used to apply traction to the spine which gently pulls on the muscles and joints and helps in easing the disc bulge back into its normal place.
- Joint mobilization can be achieved by applying varying degrees of pressure to the spinal joints.
- Electrical stimulation can also be used for relieving muscle spasms and pinched nerves.
- The ultrasound device is used for sending high-frequency sound waves to the affected region. This helps in increasing blood flow, oxygen, and nutrients to the affected disc region and helps in relieving the symptoms of a disc bulge.
- Infrared light therapy is another beneficial and effective treatment for treating the symptoms of a disc bulge. Daily use of an infrared heating pad for half an hour helps in relieving back pain for several hours without using any medication. Ordinary heating pads only heat the skin’s surface, whereas infrared heating pads penetrate deep into the tissues and are safe to use as it carries no risk of burns, skin drying etc.
- Far infrared (FIR) therapy is invisible to the naked eye and these rays can penetrate deep into the human body and improve the blood circulation in the affected region. This results in immediate pain relief along with boosting the healing process of a disc bulge.
- Stretching exercises help in relieving and reversing the disc bulge along with increased strength and flexibility of the spine.
- Proper posture of the body should be used for daily activities, such as bending, washing and taking out the garbage.
- It is also important to rest and avoid any physical activity which aggravates the condition.
- Soft tissue massage also helps in relieving the symptoms of a disc bulge. Massage helps in relaxing the tight muscles, increasing blood circulation and also increasing the production of endorphins. However, the use of massage therapy in the treatment of disc bulge or other disc problems is controversial and should be used with caution after a doctor’s approval.
- Acupuncture is an alternative therapy that uses tiny needles that unleash the natural flow of energy in the body. Acupuncture helps in relieving the symptoms of a disc bulge.
- Therapeutic massage along with heating packs applied to the affected region help in easing the stiffness and inflammation from a disc bulge. It is important to be careful when using heat application. Heat should be avoided in the acute phase of an injury.
Spinal Decompression Therapy for Reversing a Disc Bulge/L2-3 Disc Disorders
- For naturally healing or reversing a disc bulge, the space between the vertebrae needs to be increased. This encourages the bulged disc to revert back to its normal position. Increasing the intervertebral space also helps in rehydrating the disc, which in turn encourages the natural healing process of the affected spinal region along with decreasing any lower back pain, as the pain occurs as a result of nerve compression leading to inflammation of the lower back.
- If the pressure is relieved by increasing the intervertebral space, then the pain also gets relieved. Spinal decompression is the name of the process, which helps you achieve this without any medication or surgery and allows the body to naturally heal on its own.
- Different body positions affect the type of pressure exerted on our spinal discs. When a person is sitting, there is about 50% of increased pressure on the back compared to when standing in the right posture.
- When a person is lying down, there is still around 25% of the standing body pressure on the spine because of the ligaments and muscles that support our back. Gravity decompression is done at an angle where about 60% of our body weight stretches the spine and its vertebrae decreases the pressure on the discs to almost a nil.
Spinal decompression can be done by 2 methods
Inversion Therapy
- An inversion table can be used for spinal decompression and it helps in bringing great pain relief in many patients in less than a minute of its use. Long-term benefits of Inversion Therapy is that it helps in relaxation of the back muscles, elongation of the spine so that there is more space for the discs to reverse back to their normal position.
- It is important that the discs have adequate space to naturally rehydrate, realign and heal. This will help in shock absorption, spine flexibility, and improved posture.
Nubax Trio
- This is a portable traction device and it is a very good alternative to inversion tables. It is equally effective in decompressing the spine as an inversion table and is smaller and more portable. The patient needs about 5 minutes of treatment daily on a Nubax Trio where the patient has to lean over this device and relax.
Chiropractic Spinal Adjustments for Treating and Reversing a Disc Bulge
- This is an alternative therapy where a chiropractor determines the type of a disc bulge the patient has and helps in diagnosing the underlying cause. After this, the chiropractor performs targeted spinal adjustments, which will help the realignment of the spinal discs and reversing the disc bulge.
- Some of the chiropractic adjustments include flexion-distraction, physiotherapy, muscle stimulation, at-home exercises, stretches, and other treatments. Chiropractic adjustments help in relieving the symptoms of a disc bulge, such as neck stiffness, sciatica, and chronic low back pain.
- The range of motion exercises helps in improving the range of motion of the neck and spine along with strengthening the spinal muscles and preventing the development of stiffness in the spine.
Best Exercises For PLID/L2-3 Disc Disorders
Our spinal cord is supported by a number of muscles. Relevant exercises help relieve the pain and reduce the symptoms. Muscle exercises of those muscles associated with the affected area are necessary. Patients must know the region that has a slipped disc and then opt for exercises related to that muscle. The list of best exercises for the slipped disc are mentioned as follows:
- Abdominal Isometrics – It can be performed either on the floor, mat or bed. This exercise involves moving your lower back towards the surface at which you are performing this exercise. Leg movement must be reduced in this exercise and stomach muscles must be made active. This reduces pain in the lower back because of the attachment of abdominal muscles to the lower side of the vertebral column. Ten repetitions are effective.
- Crunches – Lie on a flat surface with knees bent. Cross your arm under your head, raise your head and chest in such a manner that your rib cage curl interiorly towards your backbone. Perform this exercise slowly and gradually. In the beginning, perform fewer crunches and repeat it daily and increase the number of turns as you gain strength.
- Lower back extension – Lie in an upside-down position, raise your upper body with the help of elbow and hold up yourself in an elevated position for a short span of time and then slowly lower down. Please make sure that during this exercise you do not raise your pelvic girdle (hip region).
- Bilateral knee to the chest – Lay down on a flat surface and draw your knee towards your abdominal region, repeat it 5 times and then switch leg. You can also increase the number of turns each time you repeat it.
- Iso-hip flexion – Lay down over a flat surface and draw your knees towards your chest region in a 90-degree position with your stomach. Place your hands over your knees and then exert your hand pressure to lower your knee. Then utilize the knee pressure to resist the downward movement of your legs, in all both movements should just exert pressure and allow no movements. This position should be maintained for a few seconds and then lowered slowly and gradually.
- Air bike – Sit on a chair with your chest and shoulders supported. Align your knees and feet together and then bring them towards your body and perform a pedaling motion in the air then repeat the same motion while moving your knees farther away from the body. Follow ten repetitions each time and increase its number as you gain strength.
- Hamstring stretch – Lie on a flat surface with your knees bent, place your hands under your knees and then slightly pull your leg towards your chest, repeat it with another leg. This exercise must involve a stretch over lower thigh muscle.
- Lumbar roll – Lie on a flat surface with your knee bent and your feet lying on the floor then move your legs together towards the right side and then towards your left side. Repeating these movements 5 times on each side.
The above mentioned best exercises for the slipped disc can be followed but if pain increases or muscle pain is persisting then quit these exercises right away. These exercises not only help in reducing the pain but they also activate efficient muscle movement. Along with these exercise tips, proper body postures must be also maintained to prevent further disc damages.
Home Remady for Herniated L2-3 Disc Disorders
Positioning Yoga( only home practice)
Physiotherapy is a very cheap and good way of getting rid of a herniated disc from itself. Therapists will teach your proper exercises and stretches which will improve the disc shape to a great extent. You will notice good differences while performing daily chores after just 4-5 sessions of therapy.
Turmeric
- Turmeric contains curcumin which is a very good anti-oxidant and anti-inflammatory agent. This is why it stops the gel-like fluid inside the discs from coming out and bulge. It also shows antihistamine properties which help to reduce pain because of slowed blood circulation to the area of pain.
Dimethyl Sulfoxide (DMSO)
- Dimethyl sulfoxide is a derivative from sulfur which has antioxidant properties as well as the organic sulfur present in it helps in the growth of new cells and detoxification of the body. The growth of new cells helps to replace the old cells of the discs and prevent the fluid from leaking outside.
Massage With Essential Oils
- Massage with essential oils on the full-body, especially on the spine and lower back regions, will help in good blood circulation and promote the growth of new cells. It will help relieve pain and promote better absorption of oxygen and nutrients. Essential oils will also regenerate the cells of the disc and hence stop the disc from getting slipped.
Acupressure
- In both techniques, the pressure is used for relieving the pain from the swelled area. In acupressure fingers, tips and elbow are used and acupuncture needles are used. But this should be done with the help of an experienced practitioner and not alone. This is not recommended for patients having high blood pressure and for women who are pregnant.
TENS
- TENS stands for Transcutaneous Electrical Nerve Stimulation and this is one of the best remedies for a herniated disc at home. This treatment uses low voltage electric current which is applied to the affected area and helps the body to release endorphin which decreases the pain.
Cayenne Pepper
- It is a very effective ingredient for the treatment of herniated disc. You can drink its tea or make a paste of the pepper using water and apply it on the affected area.
Diet
- Diet is necessary to keep away all types of bad conditions that might affect you. Drink a lot of water and eat a balanced diet. Take excess of fibers and proteins. During this condition, you should avoid dairy products and red meat. Also, avoid fat-free foods.
Epsom Salt
- Epsom salt is one of the widely used natural painkillers and anti-inflammatory agents. You can use this by adding 3-4 cups of salt in a hot water bath. Stay inside the bath for 15 minutes. It will help you achieve maximum relaxation. Do not use this remedy if you are diabetic or pregnant. If you are on any type of medication consult your doctor before bathing in Epsom salt.
Horsetail
- Horsetail is a herb which has high quantities of minerals in it. It nourishes our tissues and has the ability to heal broken bones and torn ligaments. All you need to do is add some horsetail leaves to half a liter of water. Boil on low heat till the water quantity reduces to half its quantity. Cool the solution and filter it off. You can drink 5 ml of the solution thrice a day. It will heal herniated disc very fast.
California Poppy
- California poppy is anti-inflammatory and analgesic in nature. This is what makes it a good treatment for a herniated disc. You can tear the leaves of California poppy into small pieces and make a paste out of it using water. Use little hot water so that when you apply the paste to the affected area it is still warm.
White Willow Bark
- White willow bark is used for reducing the discomfort of herniated discs. The chemical structure of these drugs shows a marked similarity to aspirin hence acts as an analgesic but doesn’t irritate your gut. It is also astringent and anti-inflammatory in nature. This herb might react with drugs hence do consult your doctor if you are on any kind of medication.
Comfrey Leaves
- Comfrey leaves have the power to heal bones and connective tissues of the body. All you need to do is take some fresh leaves and add it to cold water. Let it remain undisturbed for around 12 hours. After 12 hours heat the above solution and filter it. Add the filtrate to bathwater and take a bath in it 2 times a day. Do not consume it orally because it contains hepatic-toxin alkaloids.
Boswellia
- Boswellia is a naturally occurring painkiller which is a very effective remedy for a herniated disc. All you can do is make a decoction of Boswellia and consume it 2 times a day to reduce pain and discomfort associated with herniated discs. Boswellia is an organic painkiller that effectively treats the problem of a herniated disc. It is also an herbal cure for osteoarthritis.
Omega-3 Fatty Acids
- Omega-3 Fatty acids are helpful in decreasing the inflammation and pain experienced due to herniated disc disorder. This acid forms the ocollagen which is used by the broken discs for repairing itself. Eat foods that are high in this kind of fats like fish, almonds, sprouts, and walnuts.
Colchicine
- Colchicine is an active amino-alkaloid found in the plant of Kurchi or autumn crocus. This powder is obtained by crushing the seeds of the plant. It has anti-inflammatory properties that are effective against the slipped disc. Make a paste with kurchi powder and honey and consume it once a day. You can also make tea out of the powder or mix the powder in milk and have it once or twice a day.
Burdock
- Burdock contains a lot of anti-oxidants which is helpful to detoxify the body and remove all kinds of harmful substances and decrease the pain and inflammation in your body. It also treats arthritis. Burdock can be consumed as a decoction once or twice a day.
Passionflower
- Passionflower is helpful for slipped discs because the essential oils present is antispasmodic in nature. It reduces pain and inflammation. You can massage with passionflower essential oil or take capsules made from it, however, do consult your doctor before taking capsules.
Homeopathy For PLID/L4-5 Slip Disc Disorders
Primary Remedies
- Aesculus – Pain in the very low back (the sacral or sacroiliac areas) that feels worse when standing up from a sitting position, and worse from stooping, may be eased with this remedy. Aesculus is especially indicated for people with low back pain who also have a tendency toward venous congestion and hemorrhoids.
- Arnica montana – This remedy relieves lower back aches and stiffness from overexertion or minor trauma.
- Bryonia – This remedy is indicated when back pain is worse from even the slightest motion. Changing position, coughing, turning, or walking may bring on sharp, excruciating pain. This remedy can be helpful for back pain after injury and backaches during illness.
- Calcarea carbonica – This is often useful for low back pain and muscle weakness, especially in a person who is chilly, flabby or overweight, and easily tired by exertion. Chronic low back pain and muscle weakness may lead to inflammation and soreness that are aggravated by dampness and cold.
- Calcarea phosphorica – Stiffness and soreness of the spinal muscles and joints, especially in the neck and upper back, may be relieved by this remedy. The person feels worse from drafts and cold, as well as from exertion. Aching in the bones and feelings of weariness and dissatisfaction are often seen in people who need this remedy.
- Natrum muriaticum – Back pain that improves from lying on something hard or pressing a hard object (such as a block or book) against the painful area suggests a need for this remedy. The person often seems reserved or formal but has strong emotions that are kept from others. Back pain from suppressed emotions, especially hurt or anger may respond to Natrum muriaticum.
- Nux vomica – This remedy is indicated for muscle cramps or constricting pains in the back. Discomfort is made worse by cold and relieved by warmth. The pain usually is worse night, and the person may have to sit up in bed to turn over. Backache is also worse during constipation, and the pain is aggravated when the person feels the urge to move the bowels.
- Rhus Toxicodendron – This remedy can be useful for pain in the neck and shoulders as well as the lower back when the pain is worse on initial movement and improves with continued motion. Even though in pain, the person finds it hard to lie down or stay still for very long, and often restlessly paces about. Aching and stiffness are aggravated in cold damp weather and relieved by warm applications, baths or showers, and massage.
- Sulfur – This remedy is often indicated when a person with back pain has a slouching posture. The back is weak and the person feels much worse from standing up for any length of time. Pain is also worse from stooping. Warmth may aggravate the pain and inflammation.
Additional Tips
- If you are overweight, try to lose some pounds.
- Exercise every day.
- Lift things in a proper way, as guided by a therapist. Do not lift heavyweights.
- Stop smoking and drinking.
- Always make sure you are in the right posture whatever activity you may be doing.
- Wear flat and soft shoes. Avoid heels.
- Walk and move around cautiously.
Slipped discs can be really painful but with the right treatment and precautions, you can become as fit as you were before. So start taking home remedies and consult a doctor whenever you feel any kind of severe pain.
Reference

![]()










About the author