Distal Myopathy and Dysferlinopathy/Dysferlinopathy include a spectrum of muscle disease characterized by two main phenotypes: Miyoshi myopathy with primarily distal weakness and limb-girdle muscular dystrophy type 2B (LGMD2B) with primarily proximal weakness. Miyoshi myopathy (median age of onset 19 years) is characterized by muscle weakness and atrophy, most marked in the distal parts of the legs, especially the gastrocnemius and soleus muscles. Over a period of years, the weakness and atrophy spread to the thighs and gluteal muscles. The forearms may become mildly atrophic with a decrease in grip strength; the small muscles of the hands are spared. LGMD2B is characterized by early weakness and atrophy of the pelvic and shoulder girdle muscles in adolescence or young adulthood, with slow progression. Other phenotypes are scapuloperoneal syndrome, distal myopathy with anterior tibial onset, elevated serum CK concentration only, and congenital muscular dystrophy.
Types of Dysferlinopathy or Distal Myopathy
Welander (Late-onset type I) Distal Myopathy
TIA1 cytotoxic granule-associated RNA-binding protein (TIA1); Chromosome 2p13.3; Dominant
- Epidemiology
- Especially common: Mid-Sweden & Finland gene frequency 1/4000
- Penetrance: Relatively low due to late age of onset
- Genetics [rx]
- Mutation: E384K
- Finnish & Swedish patients have shared haplotype
- Homozygotes: Weakness is more severe & proximal
- Allelic disorder: ALS-FTD (ALS 26)
- TIA1 mutations also found in patients with SQSTM1 & MYH7 related distal myopathies
- TIA1 protein (Nucleolysin TIA-1 isoform p40)
- Nucleic acid-binding protein: Preferentially recognizes poly(A) homopolymers
- Induces DNA fragmentation in permeabilized thymocytes
- Component of cytoplasmic stress granules
- Other components: eIF3, G3BP & TIAL1
- May be involved in the induction of apoptosis in CTL targets
- Expressed in many tissues including muscle: Nuclear + some cytoplasmic
- Accumulates in stress granules: Prion-like aggregation
- RNA metabolism
- Clinical: Typical disease
- Onset
- Age: Usually > 40 years; Median 5th decade; Range 20 to 77
- Location
- Arms; Wrist & Finger extensors: Most common
- Legs (Foot drop): 25%
- Weakness
- Hands > Legs in most
- Muscles involved: Long finger extensors; Intrinsic hand; Thumb & index-finger
- Progression to legs: Toe & ankle extensors
- Only rarely proximal weakness
- Tendon reflexes: Reduced at ankles
- Slow progression with a normal life span
- Sensory loss: Some patients; Subclinical neuropathy common
- Autonomic: Altered peripheral vasomotor response after vasoconstriction
- Onset
- Homozygotes: Subset with more severe disease
- Earlier onset
- Rapid progression
- Early: Leg & Proximal weakness
- Wheelchair < 50 years
-
- CK: Normal or mildly elevated
- EMG: Myopathic; Some irritability
- Muscle Pathology
- Chronic myopathic: Varied fiber size; Splitting
- Rimmed vacuoles: Variably present; contain increased p62, Ubiquitin & TIA1
- Tubulo-Filamentous inclusions (15 to 18 nm): Sarcoplasm & muscle fiber nuclei
- Neurogenic changes
- TIA1: Increase in the cytoplasm with occasional aggregates in atrophic & vacuolated muscle fibers
- Sural nerve: Aδ fiber lossLaboratory
- TIA1 variant: ALS 26 (ALS-FTD) [rx]
- Epidemiology: 1 family, 5 patients; 5 other ALS mutation carriers
- Genetics
- Inheritance: Dominant or Sporadic
- Mutations
- Missense: P362L, V294M, M334I, G355R, V360M, A381Y
- Low-complexity domain
- Other ALS: Increased burden of TIA1 low-complexity domain mutations in ALS patients vs controls
- ~ 2% of Familial ALS
- Allelic disorder: Welander distal myopathy
- TIA1 protein
- Clinical
- Onset ages: 28 to 73 years; Mean 59 years
- Weakness
- Bulbar
- Limb
- Aphasia
- Fronto-Temporal dementia
- Disease course: Death in 2 to 6 years
- Laboratory
- Brain pathology
- Inclusions: Round, hyaline, TAR DNA-binding protein 43 (TDP-43)-positive; Lewy body like
- Locations: Extra-motor neocortex, Motor cortex, Substantia nigra, Spinal cord corticospinal tracts & ventral horn
- Brain pathology
Finnish (Tibial) (Late-onset type IIa; Udd) Distal Myopathy
Titin Chromosome 2q31.2; Dominant
- Epidemiology
- Finland
- Large population with the same mutation
- Most common muscle disease
- Other regions
- French, Belgian & Spain families
- Iberian mutation: c.107889delA
- Finland
- Genetics
- Finnish population
- Probably arose from a single ancestor
- 20 per 100,000 population
- Mutations
- Common: 11 bp insertion-deletion of nucleotides 293,269 to 293,279 (In terminal exon)
- Other: Missense or Truncating; Last 2 TTN exons
- Allelic Disorders
- Genotype-Phenotype
- Same (11 bp) mutation may produce different patterns of weakness
- Most common: Tibial MD
- Other: Proximal; Posterior leg
- Severe or variant phenotype
- Often have 2nd titin mutation (Recessive LGMD 2J)
- Same (11 bp) mutation may produce different patterns of weakness
- Finnish population
- Clinical
- Onset age
- Heterozygotes
- 4th to 8th decade; Most in 40’s
- Many remain asymptomatic
- Homozygotes: Childhood; LGMD 2J
- Heterozygotes
- Distribution of weakness
- Legs: Anterior tibial selectively involved
- Arms
- Never hand weakness in Finnish patients
- Some Non-Scandinavian families with hand weakness
- Proximal weakness: 15%; Mild
- Progression
- Slow: Foot drop 10 to 15 years after onset when long toe extensors become weak
- Proximal legs may become weak late in disease
- Quadriceps weak in rare male
- Many remain ambulatory
- Earlier onset (2nd decade) may lose ambulation in 3rd to 6th decade
- Homozygotes: Loss of ambulation by 3rd decade
- Cardiomyopathy
- Onset age
- Laboratory
- CK: Mild elevation or normal
- MRI: Selective fatty replacement of muscles
- Early: Anterior tibial; Gluteus minimus
- Later: Gastrocnemius
- Pathology: Dystrophic (100%)
- Muscle fibers: Size variation; Splitting; Internal nuclei
- Basophilia
- No inflammation
- Rimmed vacuoles (30%): Contain degenerative cytoplasmic debris & organelles
- Calpain 3: Reduced
- Apoptosis in muscle nuclei
- Anti-titin antibodies
- Normal binding for most
- Binding to C-terminal epitope reduced
Markesbery (Late adult-onset type IIb) Distal myopathy
ZASP; Chromosome 10q23.2; Dominant [rx]
- Epidemiology: English, French & Finnish families
- Genetics
- Mutation: A165V; Common in European families
- Allelic disorders
- Clinical
- Onset age: > 40 years
- Weakness
- Early: Distal legs
- Hands: Distal finger & wrist extensors
- Late: Proximal arms & legs
- Progression
- Slow: Slower in Finnish tibial type
- Disability common
- Cardiomyopathy: Occasional patient
- Laboratory
- Serum CK: Normal or Slightly elevated
- Muscle pathology: Rimmed vacuoles
- MRI
Hereditary Inclusion Body Myopathy 2 (HIBM2; Nonaka): Recessive
A UDP-N-Acetylglucosamine 2-Epimerase/N-Acetylmannosamine kinase (GNE) ; Chromosome 9p13.3; Recessive
- Nosology: Same disorder as
- GNE myopathy
- Nonaka distal myopathy
- IBM2
- Epidemiology
- Iranian-Jewish families: Prevalence in Jews of Persian ancestry = 1:500
- Other families: Mexico; India; Bahamas; Georgia
- Prevalence range: 1 to 21 per 1,000,000
- Genetics: GNE gene mutations
- Type
- Missense >> Stop
- Heterozygous > Heterozygous
- Mutation locations
- Across entire gene
- Domains: Epimerase or Kinase
- Geographic
- Iranian-Jewish & Sangesar (Mahdishahr) in Northern Iran: Homozygous for Met712Thr
- Japanese (Nonaka) & Korean: V572L (60%; Founder effect); Homozygous or Heterozygous
- Japanese, Other: Asp207Val (Late-onset; Asymptomatic if homozygous); Val603Leu (Often homozygous)
- Korean: C13S
- Northern Britain: Ala662Val; Asp409Tyr
- Roma Gypsy & Indian (Rajasthan): Ile618Thr (Homozygous)
- Indian: Val727Met
- Middle Eastern (Persian Jews): Met743Thr
- Earlier onset: L539S
- Milder or atypical phenotype: H333R; Y361X
- Allelic disorder: Sialuria
- Type
- GNE protein: Bifunctional
- Catalyzes 1st 2 steps in the synthesis of N-acetylneuraminic (sialic) acid: Rate-limiting step
- Epimerase activity: N-terminal
- Kinase activity: C-terminal
- Tissue expression
- Full-length protein: Liver; Salivary glands; Intestinal mucosa
- Shorter form (exon 4 missing)
- Predominantly expressed in skeletal muscle
- Present in similar levels in control & myopathy patients
- GNE Mutants: No correlation between Disease pattern & Changed enzyme activity
- Sialic acid disorders
- External link: GeneTests
- Clinical
- Onset
- Age: 2nd or 3rd decade; Range 12 to 78
- Weakness: Foot drop
- Weakness
- Early: Peroneal & Anterior tibial
- Distal & Proximal
- Asymmetry: Some muscles
- Lower extremity
- Onset: Peroneal weakness (Anterior distal legs), Ankles & Toes
- Then: Hips, Hamstrings & Gastrocnemius
- Upper extremity
- Wrist: Extension & Flexion
- Hands: Intrinsic muscles; Grip
- Shoulder girdle
- Scapular winging: Some patients
- Neck: Flexors or Extensors may be weak
- Respiratory
- Frequency: 30%
- Especially with earlier onset
- Rarely severe
- Sparing
- Quadriceps
- Spared in most patients
- Weak in few patients (4%): Disease progression
- Arms: Deltoids
- Legs
- Hip muscles
- Ankle: Plantar flexors
- Cranial nerves
- Ptosis: Rare
- Facial weakness: Occasional patient
- Quadriceps
- Progression: Slow
- Usual: Weakness progresses to proximal & trucnal muscles
- Disability within 10 to 20 years of onset
- Often become wheelchair dependent
- Few patients: Weakness remains distal
- Lifespan: Not substantially reduced
- Variants
- Upper extremity early: Distal arm weakness
- Proximal leg: Hamstring weakness, No foot drop
- Axial early
- Late-onset
- Onset
- Laboratory
- CK: Mild elevation, 2x to 5x
- Urine sialic acid: Not elevated
- EMG: Spontaneous activity; Myopathic potentials
- MRI: Quadriceps sparing
- Muscle Pathology
- Myopathic
- Varied muscle fiber size
- Necrosis & Regeneration: Some patients
- Vacuoles: Red-rimmed
- Contain paired helical filaments
- ? Autophagic
- Many, but not all, patients
- Aggregates
- Constituents: βAPP; Ubiquitin; SMI-31 binding; ApoE; LC3; α-synuclein; Tau; TDP-43.
- 15 to 18 nm filamentous inclusions in cytoplasm & nucleus
- Sialylation: Abnormal on muscle proteins
- Mainly affects O-glycan sialylation
- Peanut (PNA) lectin staining of Gal(β1-3)GalNAc disaccharide: Increased on the sarcolemma
- NCAM pathology: Migrates as single, smaller 130 kD band on Western blot in some patients
- Myopathic groups: Vacuolar & small fibers clustered in regions
- Inflammation uncommon, but occasionally present
- α-Dystroglycan staining: Reduced
- LAMP2: Increased granular staining
- Myopathic
- GNE variant: Sialuria
- Epidemiology: 10 patients
- Genetics
- Inheritance: Dominant
- GNE Mutations
- Epimerase domain
- Binding site of cytidine monophosphate-sialic acid of GNE/MNK
- Functional defect: Loss of feedback inhibition
- Clinical
- Developmental delay
- Hepatosplenomegaly
- Laboratory
- Urine: Free sialic acid high
Miyoshi Myopathies
- Miyoshi 1 (MMD1): Dysferlin; 2p13.2
- Miyoshi 2 (MMD2): ? 10p
- Miyoshi 3 (MMD3): ANO5; 11p14
Miyoshi (Early adult-onset distal myopathy type II; MMD1)
Dysferlin ; Chromosome 2p13.2; Recessive
- Genetic associations
- Allelic with: Limb-girdle muscular dystrophy 2B
- Genetic heterogeneity
- ? Some families linked to chromosome 10 & other loci
- Protein: Dysferlin
- Skeletal muscle > Heart
- Attached to the cell membrane
- Clinical features
- Presymptomatic: Mild gastrocnemius wasting
- Early Adult-Onset: Teens to 38 years
- Weakness & Wasting
- Posterior Legs: Gastrocnemius; Soleus
- Symmetric
- Arms & Proximal muscles involved late
- Calf wasting
- Progression: Related to disease duration
- Asymmetry in families not linked to 2p
- Laboratory
- CK: Very high up to 20,000
- MRI
- Selective involvement of hamstring, gastrocnemius & soleus
- Early muscle edema
- Pathology: Dystrophic Muscle
- Necrosis & degeneration of muscle fibers
- Endomysial connective tissue: Increased in more involved muscles
- Muscle fibers: Size variation; Splitting
- No vacuoles
- Inflammation
- Perimysial & perivascular cell infiltrates
- Variable: May occur in some muscles but not others
- Variant: Anterior tibial onset
- Epidemiology: Spanish family
- Dysferlin mutation: 5966delG
- Onset: 14 to 28 years
- Weakness: Rapidly progressive
- Serum CK: Very high
- Muscle: No vacuoles; Absent dysferlin
- Differential diagnosis: Calpain-3 mutation
- Muscle CT scan: Abnormal medial head of the gastrocnemius
- Muscle: Absent calpain-3; Normal dysferlin
Miyoshi Myopathy 2 (MMD2)
Chromosome 8q22.3; Recessive
- Epidemiology: 3 Dutch families
Gowers (Laing; Early Adult-Onset Distal Myopathy Type III; MPD1)
Myosin heavy chain 7 (MYH7); Chromosome 14q11.2; Dominant or Sporadic
- Epidemiology
- Australian, German, Italian & Austrian families
- Genetics: MYH7 mutations
- Types: Missense; Charge reversing
- General location
- LMM region
- α-Helicoidal rod domain
- Exons 32, 34, 35, and 36
- Specific mutations: Arg1500Pro, Glu1508del, Lys1617del,
Ala1663Pro, Leu1706Pro, Lys1729del, Leu1793Pro - Leu1793Pro: May also produce neonatal hypotonia & Cardiomyopathy
- De novo mutations: 20% to 35%
- Clinical correlations
- Individual mutations may produce widely varied phenotypes
- Severe phenotype: L1591P
- Allelic disorders
- May have additional TIA1 mutations
- MYH7 protein
- Present in type I (Slow) muscle fibers
- Predicted mutation effect: Disrupts
- The ability of myosin tail to form normal coiled-coil structure
- Myosin dimerization: Altered structure of the thick filament
- Clinical Features
- Onset
- Age
- Common: < 5 years
- Range: Childhood or Young adult, 1.5 to 26 years
- Occasional: Neonatal or 6th decade
- Interfamilial variation
- Distal leg weakness: Steppage gait; Foot drop
- Hypotonia
- Age
- Weakness: Intrafamilial variation
- Legs
- Ankle dorsiflexion: Often severe with foot drop
- Hanging big toe
- Proximal muscles: Later in disease course
- Neck: Sternocleidomastoids & Neck flexors
- Arms
- Extensors: Finger (esp 5th) & Wrist
- Onset age: 3rd to 5th decade; 5 to 10 years after legs
- Later: Infraspinatus & Supraspinatus
- Intrinsic hand muscles: Normal
- Later in the course: Some families
- Hip & Shoulder abductors & external rotators
- Face: Mild
- Usually symmetric: Asymmetry reported
- Legs
- Muscle discomfort: Some patients
- Muscle size: Anterior tibial usually atrophic
- Tendon reflexes: Reduced at ankles; Present elsewhere
- Scoliosis (50%)
- Tremor: Hands, then postural
- ? Peripheral neuropathy with hypomyelination: Some patients
- Cardiomyopathy (50%)
- Dilated, Hypertrophic or Non-compacted left ventricle
- Course
- Slow progression
- Proximal weakness with disease progression
- Legs, Abdominal muscles
- Later ages: Mild disability
- Life expectancy: Normal
- Onset
- Laboratory
- CK: Normal or Mild elevation to 8x high
- EMG: Myopathic; Some spontaneous activity
- NCV: Normal
- Muscle Pathology
- Myopathic: Varied fiber size; Internal nuclei
- Type I muscle fibers: Small; Grouped; Predominance in some patients
- Myosin heavy chain expression: Abnormal; Double positive fibers
- Hyaline inclusions: Light green-stain on Gomori trichrome
- Vacuoles: None in most patients; Autophagic rimmed reported
- Cytoplasmic bodies
- Severe, early-onset patient
- Contents: Myotilin & Actin; Desmin+ rim
- Intranuclear tubule-filamentous inclusions: 15 to 20 nm
- Some muscle fibers (3%) express both fast & slow myosin
- Distal muscles may be more abnormal
- MRI
- Leg: Atrophy & later Increased signal in tibialis anterior & EHL
- Thigh: Abnormal Biceps & Semimembranosus
- MYH7 Variant: Distal myopathy with Hypertrophic cardiomyopathy [rx]
- Genetics
- Inheritance: Dominant
- Mutation: Val606Met; Homozygous
- Clinical
- Later onset: 6th decade
- Muscle hypertrophy: Anterior tibial
- Cardiomyopathy: Hypertrophic
- Genetics
- MYH7 Variant: Proximal weakness & Cardiomyopathy
- Genetics
- Inheritance: Recessive
- Mutation: Homozygous Glu1883Lys
- Clinical
- Weakness: Proximal
- Cardiomyopathy: Hypertrophic
- Pathology: Hyaline bodies in skeletal & cardiac muscle fibers
- Genetics
Distal Dystrophy with Rimmed Vacuoles
Perilipin-4 (PLIN4) ; Chromosome 19p13.3; Dominant
- Epidemiology: 1 Italian family; 22 patients
- Genetics
- Mutation
- Large repeat insertion: 9 Extra 99-mer nucleotide repeats; In-frame
- Coding
- Exon 3
- Amphipathic domain repeat expansion
- Mutation
- PLIN4 protein
- Highest expression: Skeletal muscle
- Coats: Phospholipid monolayer surrounding lipid droplets
- Regulates: Lipid droplets
- Absent perilipin-4: No phenotype
- Amphipathic domain: Normal protein
- 11-mer: Repeated 3 times; Forms a 33-mer
- 33-mer: Repeated 29 or 31 times
- Amphipathic domain: Mutated protein
- 33-mer: Repeated 40 times
- Size: Increased by 297 amino acids
- Perilipin disorder: Other
- Lipodystrophy, familial partial, type 4
- Clinical
- Onset age
- Adult; 4th to 50 years
- Weakness
- Early: Distal legs
- Distribution
- Most involved: Distal legs (Foot dorsiflexion)
- Also: Neck flexion; Wrist & Finger extensors; Scapular
- Progression
- Variable: Asymptomatic to Severely disabled
- Respiratory failure: Rare
- Onset age
- Laboratory
- Serum CK: Normal, or Mildly elevated (Up to 4x)
- EMG: Myopathic; High-frequency discharges
- NCV: Normal
- Cardiac: Normal
- Muscle pathology [rx]
- Fiber size: Varied, atrophy & hypertrophy
- Internal nuclei
- Necrosis
- Focal phagocytosis of muscle fibers
- Rimmed vacuoles
- Mainly in hypertrophic muscle fibers
- Located near fiber surface
- Contents: Basophilic granular material
- Lysosomal features
- Acid phosphatase positive: Around vacuoles
- LAMP-1 & LAMP-2 negative
- LIMP-I on the surface of vacuoles & fibers
- Inclusions
- Sarcoplasmic: p62; FK2; Perilipin-4
- Muscle Western blot: 2 PLIN4 bands, Normal & Increased sizes
Hereditary Inclusion Body Myopathy (IBM1; HIBM1) Dominant
Desmin; Chromosome 2q35; Dominant
- Nosology
- Originally identified as HIBM1
- Desmin mutations found: Myofibrillar myopathy
- Clinical
- Onset: Adult; 25 to 40 years
- Weakness
- Quadriceps early
- Distal: Foot Dorsiflexion
- Proximal: After disease progression
- CNS involvement: Some families
- Progression: Slow
- Laboratory
- Serum CK: Normal or Mildly increased
- Pathology
- Red rimmed vacuoles: Prominent on GT stain
- Multifocal myopathic changes
- Myopathic fascicles: Variation in fiber size; Endomysial fibrosis
- Vacuoles more common in myopathic fascicles
- ± Inflammation
- Also see: Other IBM
- Inclusion body myositis, Sporadic: Wrist & Finger flexors & Quadriceps weakness
- IBM2: Sporadic or Recessive; GNE; Chromosome 9p12; Distal weakness
- IBM3: Joint contractures & ophthalmoplegia: Myosin heavy chain IIa; Chromosome 17p13; Dominant; Proximal weakness
- IBM + Paget’s & Dementia: VCP; Chromosome 9p13; Dominant; Proximal & Distal weakness
- SQSTM1: 5q35; Dominant or Sporadic
- Differential diagnosis of rimmed vacuoles
Distal Myopathy with Vocal Cord & Pharyngeal Weakness (MPD2; VCPDM)
- Matrin 3 (MATR3); Chromosome 5q31.2; Dominant
- Epidemiology: North American, German & Bulgarian families
- Genetics [rx]
- Mutation: Ser85Cys
- Allelic disorders
- Familial ALS 21, Dominant
- Fronto-Temporal Dementia
- Mutation: Retrotransposed Full-Length Transcript of Martin-3 Variant 5
- Martin 3 protein [rx]
- Cell location
- Nuclear matrix
- The inner face of the nuclear envelope
- May move to the cytoplasm in diseased cells
- Tissue expression: Muscle & Other tissues
- Contains RNA-DNA binding motif
- Interacts with
- Proteins: TDP-43; DHX9
- DNA sequences: Repetitive; Adenine/Thymine-rich
- RNA: RNA stabilized by MATR3 binding
- Self-association
- Functions
- Transcriptional control
- DNA repair
- Stabilizes mRNA encoding Rad51
- Cell location
- Clinical
- Onset
- Age: 30 to 57 years; Average 46 years
- Weakness: Legs (Anterior & Distal); Occasionally Hands or Voice
- Weakness
- Initially asymmetric; May become symmetric
- Legs > Arms
- Peroneal distribution
- May also involve inversion
- Gastrocnemius: Relatively spared
- Hands
- Different finger extensors: Variable weakness
- Abductor policis brevis: Early
- Proximal
- Shoulder weakness: Especially deltoid
- Asymmetric
- Respiratory: < 86% of expected in 60%
- Bulbar dysfunction
- Voice (65%)
- Onset usually after limb weakness
- Initially: Hypophonic & Breathy
- Later: Wet, gurgling, hoarse; Hypernasal resonance
- Pharyngeal: Dysphagia & Aspiration
- Voice (65%)
- Tendon reflexes: Brisk; Absent at ankle
- Course
- Slowly progressive
- Respiratory failure: After 1 to 2 decades
- Serum CK: Normal to 8x High
- EMG
- Myopathic (especially pharynx & vocal cords)
- Neuropathic: Spontaneous activity; Complex repetitive discharges
- Nerve conductions: Normal or Mildly slowed
- MRI: Fat replacement
- Leg: Soleus & Medial gastroc
- Thigh: Posterior, Semimembranosus
- Paraspinal (50%)
- Asymmetric in some
- Muscle pathology
- Myopathic: Gastrocnemius > Quadriceps
- Fiber size: Varied
- Internal nuclei
- Rimmed vacuoles: Subsarcolemmal; Often elongated
- Myonuclei
- ? Variable staining
- Aggregates: Perinuclear, Cytoplasmic
- Ultrastructure
- Absent perinuclear sarcomeres
- Nuclei: Abnormal invaginationsLaboratory
- Onset
- MATR3 variant syndrome: Amyotrophic Lateral Sclerosis (ALS), Familial 21 (ALS21) [rx]
- Epidemiology: Sardinian & British families
- Genetics
- Inheritance: Dominant
- Mutations: Missense; Phe115Cys, Thr622Ala, Pro154Ser; Ser85Cys; Ser707Leu
- Allelic with: Distal myopathy with Vocal Cord & Pharyngeal Weakness (MPD2)
- MATR3 protein
- Clinical: Amyotrophic Lateral Sclerosis
- Onset age: 4th to 8th decade
- Weakness: Asymmetric; Arms & Legs; Dysarthria; Respiratory
- Muscle atrophy: Distal > Proximal
- Fasciculations
- Tendon reflexes: Brisk
- Cognitive disorders: Some patients (Phe115Cys, Ser707Leu)
- Course
- Death < 6 years
- Common: Rapidly progressive
- Ser85Cys: More slowly progressive
- Pathology
- Normal neurons: Nuclear, granular
- Disease: c9orf72 ALS = Cytoplasmic
HEREDITARY INCLUSION BODY MYOPATHY (HIBM) + PAGET DISEASE (IBMPFD)
Inclusion Body Myopathy with Paget disease of Bone & Dementia 1 (IBMPFD1)
Valosin-containing protein (VCP, p97); Chromosome 9p13.3; Dominant
- Nosology: Multisystem proteinopathy 1 (MSP1)
- Epidemiology
- Worldwide: > 70 families
- Male = Female
- Genetics [rx]
- Mutations
- Missense
- > 60 different
- Several involve same amino acid residue
- Locations
- N-terminal: Exons 1 to 6; N-, L1, or D1-ATPase domains
- Arg95G; Ile126Phe; P137L; Arg155C; Arg155H; Arg155Leu; Arg155P; Arg155S;
G156S; G157Arg; R159H; Leu198Trp; Arg191Gln; A232E; A439S
- Clinical genetic correlations
- R155C: Frontotemporal dementia with intraneuronal inclusions
- Arg159His: Interfamily variability
- A232E: Fractures & Paget disease at earlier age
- Homozygous mutation: Arg159His
- Allelic with
- ALS, Familial 14 ± FTD (9%)
- Familial Spastic Paraparesis
- Distal myopathy + Dementia
- CMT 2Y
- Demyelinating neuropathy
- Parkinson disease (4%)
- Cardiomyopathy
- Mutations
- VCP protein
- Locations: Ubiquitous
- Functions
- Protein degradation pathways (Autophagy): Regulatory role
- Cell cycle & Membrane fusion
- Segregates ubiquitinated protein complexes
- Binds ubiquitin
- AAA ATPase
- Chaperone
- Expression: Most tissues
- Aggregate-related
- Associates with aggregate prone polyglutamine containing proteins
- Present in inclusions from ALS, Parkinson’s disease & Huntington disease
- Mutated protein [rx]
- Causes increased levels of ubiquitinated cell proteins
- Sensitization to proteasome stress
- Impairs endoplasmic reticulum-associated degradation (ERAD) of proteins
- Promotes formation of aggregates
- Contain p97/ VCP, ubiquitin conjugates & ER-resident proteins
- Impaired protein aggregate clearance
- Upregulation of autophagy-related proteins
- Normal: Polymerization into hexamers; ATPase activity
- Clinical [rx]
- Intrafamilial variability: Prominent
- Onset
- 3rd & 4th decade
- Variable: Back pain; Weakness; Dementia
- Myopathy: Weakness (90%)
- Onset
- Ages: Mean 43 years; Range 3 to 66 years
- Presenting symptom in > 50%
- General: Marked variability in severity & pattern within families
- Legs: Distal & Proximal
- Arms: Proximal & Distal
- Respiratory
- Often involved: Vital capacity 29% to 70%
- Failure: With disease progression
- Scapular winging: Supraspinatus & Infraspinatus weakness
- Other regions: Some patients
- Cranial nerves: Face (50%); Tongue
- Posterior neck: Head ptosis
- Back: Camptocormia
- Dysphagia (22%)
- Finger flexion
- Ophthalmoplegia: 1 family (R155S)
- Asymmetric: Often
- Progression
- Slow: Over 1 to 2 decades
- To severe disability
- Severe weakness: Common
- Loss of independent walking in 13 years
- Death in 5th to 7th decade
- Onset
- Bone disease (42%)
- Paget disease (43% to 49%)
- Spine: Most common lesion location
- Other lesion locations: Hip; Skull; Pelvis
- Pain
- Onset: Mean 42 years; Range 29 to 61 years
- External link: Paget disease
- Skeletal: Lumbar lordosis
- Paget disease (43% to 49%)
- Dementia (30% to 37%)
- Onset
- Mean 52 to 55 years; Range 30 to 86 years
- Usually after Paget’s or Myopathy
- Frontotemporal (Behavioral variant)
- Language: Anomia; Aphasia; Mutism
- Personality change: Apathy; Agitation
- Hallucinations: Visual; Auditory
- Relatively preserved memory
- Onset
- Cardiomyopathy: Occasional
- Heart failure late in disease course
- Dilated
- Amyloid may be present
- Sensation: Normal
- Other: Occasional
- Hepatic disorders
- Cataracts
- Polyneuropathy: Sensory-Motor
- Motor neuron loss
- Parkinsonism
- Laboratory
- Serum CK: Normal (80%), or Mildly increased (400 to 1165)
- Serum Alkaline phosphatase: High with Paget disease
- EMG: Variable
- Myopathy: Small amplitude, Polyphasic Brief motor unit potentials
- Spontaneous activity: Fibrillations; Positive sharp waves
- Chronic denervation: Some patients
- NCV: Normal
- Muscle biopsy
- Fiber sizes
- Varied
- Atrophy: Regional or Grouped; Some angular fibers, scattered
- Hypertrophy: Scattered muscle fibers
- Endomysial connective tissue: Patchy Increased
- Vacuoles: Rimmed
- Aggregates
- VCP staining inclusions: Sarcoplasmic & Myonuclear
- Other aggregates: TDP43; p62
- MHC-I on muscle fibers: Varied
- Ultrastructure: Tubulofilamentous inclusions
- Fiber sizes
- Muscle MRI: Widespread changes including axial muscles
- Echocardiogram: Cardiomyopathy (Late)
- Radiology: Paget disease of bone
- Brain pathology
- Cortical atrophy
- Inclusions: Intranuclear; Ubiquitin & TDP-43 positive
- VCP Variant syndrome: ALS, Familial 14 ± FTD (FTDALS6; ALS 14 ) [rx]
- Epidemiology: 1% to 2% of Familial ALS
- Genetics
- Dominant or Sporadic
- VCP Mutations: Ile151Val; R155H; R159G; R191Q; D592N
- Clinical
- Onset
- Age: 4th to 6th decade
- Weakness: More commonly in legs
- Upper motor neuron
- Spasticity: Arms & Legs
- Bulbar: Dysarthria; Dysphagia
- Tendon reflexes: Brisk, including jaw jerk
- Lower motor neuron signs
- Atrophy
- Weakness: Patterns not well described
- Respiratory failure
- Progression: Variable
- Respiratory failure
- Death: 1 to 12 years
- May also have VCP multisystem disease
- Dementia
- Paget
- Myopathy
- Onset
- Laboratory
- EMG: Denervation & Reinnervation
- Fibrillations
- Fasciculations
- Serum CK: Normal to 900
- Brain pathology
- Corticospinal tract pallor
- Ubiquitin-positive inclusions in surviving neurons
- TDP43 or p62 (SQSTM1) aggregates
- tau (MAPT ) aggregates: D395G mutation (601023.0014)
- EMG: Denervation & Reinnervation
- VCP Variant syndrome: Distal myopathy + Dementia [rx]
- Epidemiology: Finnish family
- VCP mutation: P137L
- Clinical
- Onset
- Age: > 35 years
- Leg weakness
- Weakness: Distal, anterior legs
- Dementia: Onset > 50 years
- Paget disease: 1 patient
- Onset
- Muscle pathology (Anterior tibial)
- Myopathic
- Endomysial fibrosis
- Atrophy
- Hypertrophy
- Ring fibers
- Vacuoles, rimmed: Some staining for TDP-43 or p62
- Myopathic
- VCP Varant syndrome: Progressive spastic paraplegia + Paget’s disease of bone [rx]
- Epidemiology: Dutch family
- VCP mutation: Arg159Cys
- Clinical
- Onset
- Age: 5th to 6th decade
- Gait disorder
- Spastic paraparesis
- Tendon reflexes: Increased in legs
- Spasticity: Legs
- Weakness: Distal legs (Anterior tibial)
- Tongue fasciculations: 1 patient
- Paget’s disease of bone
- Cognition: Normal
- Course
- Progressive to wheelchair over 10 years
- Survival: > 2 decades
- Onset
- Laboratory
- Alkaline phosphatase: High
- EMG: Denervation
- VCP Variant syndrome: CMT 2Y Sensory-Motor neuropathy
- Epidemiology: 1 family
- VCP genetics
- Mutation: Gly185Lys
- Inheritance: Dominant
- Clinical
- Onset age: 1st to 6th decade
- Weakness: Distal; Legs > Arms
- Sensory loss: Distal; Legs > Arms; Panmodal
- Laboratory
- NCV
- CMAP & SNAP amplitudes: Reduced
- Velocities: Normal
- NCV
- VCP Variant syndrome: Demyelinating Neuropathy [rx]
- Epidemiology: 1 patient, others in family with ALS or IBM
- Genetics
- Mutation: Arg191Gln in family, patient not studied
- Clinical
- Onset age: 6th decade
- Weakness: Diffuse, Arms & Legs
- Sensory loss: Vibration
- Tendon reflexes: Absent
- Cardiomyopathy
- Laboratory
- NCV: DL prolonged; CV 25 to 39 M/s; F-waves absent
- Nerve biopsy: Schwann cells with intranuclear ubiquitin; No demyelination
- CSF: Normal
- Serum CK: Normal
- VCP allelic disorder: VCP homozygous mutation [rx]
- Epidemiology: Belgian male
- Genetics
- Mutation: Homozygous; Arg159His
- Families (Heterozygous): Myopathy; Parkinsonism; Dementia
- Clinical
- General: May be similar severity to heterozygotes
- Onset age: 29 years
- Weakness
- Limb-Girdle
- Distal legs
- Legs > Arms
- Periscapular
- Paraspinal
- Muscle wasting: Legs
- Paget disease of bone
- Laboratory
- Serum CK: 1100
- Muscle
- Rimmed vacuoles
- Endomysial macrophages
- Necrosis & Regeneration
- MHC1: Patchy increase
- EMG: Mixed myopathy & Neuropathy
- MRI: Asymmetric, patchy involvement; Paraspinal & Legs
- Bone: Paget lesions
Myopathy with Paget disease of Bone ± Cognitive change or Motor Neuron Disease (IBMPFD2) [rx], [rx]
Heterogeneous nuclear ribonucleoprotein A2/B1 (HNRNPA2B1) ; Chromosome 7p15.2; Dominant
- Nosology: Multisystem proteinopathy 2 (MSP2)
- Epidemiology: 1 US family, 5 patients
- Genetics
- Mutation: Missense; D290V/D302V; Located in prion-like domain
- Allelic disorder: Paget disease of Bone, P310L mutation
- HNRNPA2 protein
- Most abundant isoform of hnRNPA2B1
- Localization: Nucleus > Cytoplasm (mRNP granules containing untranslated mRNAs)
- RNA binding
- Contains: Prion-like domain
- Essential for assembly of ribonucleoprotein granules
- Tends to assemble into self-seeding fibrils: Exacerbated by disease mutations
- Recruited to stress granules
- Clinical
- Onset age: 3rd to 5th decade
- Myopathy (100%)
- Weakness
- Legs: Distal, Ankles & Toes
- Upper extremity: Proximal; Scapular winging
- Muscle atrophy
- Slowly progressive
- Weakness
- Paget disease of bone (100%)
- May be severe & widespread
- Location: Long bones
- Cognitive disorders (40%)
- Motor neuron disease (40%)
- Weakness
- Rapidly progressive
- Muscle pathology
- Fiber size: Varied; Atrophic groups
- Internal nuclei
- Increased endomysial connective tissue
- Vacuoles: Rimmed
- TDP-43 inclusions
- Muscle fiber degeneration & Regeneration: Occasional
- Laboratory
- Radiology: Paget disease of bone
- EMG: Myopathic
- Serum CK: High or Normal; May become normal with progressive disease
- Serum Alkaline phosphatase: High
- Serum Osteocalcin: High in some patients
Myopathy (IBM) with Paget disease of Bone without Dementia (IBMPFD3) [rx]
Heterogeneous nuclear ribonucleoprotein A1 (HNRNPA1); Chromosome 12q13.13; Dominant
- Nosology: Multisystem proteinopathy 3 (MSP3)
- Epidemiology: German family
- Genetics
- Mutations: Missense; D262V/D314V; Located in prion-like domain
- Allelic disorders
- ALS20 & Motor syndromes
- IBM + Paget without Dementia 3
- HNRNPA1 protein
- Localization: Nucleus & Cytoplasm
- Ribonuclear proteins & Disorders
- Contains: Prion-like domain (PrLD)
- Enriched in uncharged polar amino acids & glycine
- Other proteins with PrLD
- TDP-43: ALS 10
- FUS: ALS 6
- EWSR1: ALS, Sporadic
- TAF15: ALS, Sporadic
- HNRNPA2B1: Myopathy + Pagets ± Motor neuron disease or Cognitive disorders
- TIA1: Welander distal myopathy
- HNRNPA1: IBMPFD3
- Involved in
- RNA binding
- Packaging of pre-mRNA into hnRNP particles
- Transport of poly(A) mRNA from nucleus to cytoplasm
- Essential for assembly of ribonucleoprotein granules
- Tends to assemble into self-seeding fibrils: Exacerbated by disease mutations
- Recruited to stress granules
- Clinical [rx]
- Onset
- Childhood: Clumsy
- Weakness: 35 to 43 years
- Myopathy (100%)
- Early: Proximal legs; Iliopsoas
- Foot dorsiflexors
- Abdominal wall
- Arms: Usually spared
- Scapular winging: Slight
- Progressive: Wheelchair in 5th or 6th decade
- Paget disease (50%)
- Cognition: Normal
- Onset
- Muscle pathology
- Fiber size: Varied
- Internal nuclei
- Vacuoles: Rimmed
- TDP-43 inclusions
- Laboratory
- Serum CK: 225 to 1250
- Alkaline phosphatase: Normal to 8x high
- HNRNPA1 Variant syndrome: Motor neuron disease only (ALS20)
- Nosology: ALS19 or ALS20
- Epidemiology: 2 Families & 1 Simplex patient
- Genetics
- Inheritance: Dominant
- Mutations
- Family: Same as myopathy (D262V/D314V)
- Single ALS patient: N267S/N319S
- Flail arm: c.862/1018C>T (p.P288S/P340S)
- Clinical
- Onset age: Adult
- Motor neuron syndromes
- ALS-like
- Flail-arm syndrome
- Muscle wasting & weakness: Distal or Proximal; Arms > Legs
- Also: Bulbar features, Dysphagia, Dysarthria
- Tendon reflexes: May be brisk
- Course: Slow progression (3 decades)
- Scapuloperoneal SMA
- Other CNS: Normal
- Electrodiagnostic
- EMG: Ongoing & Chronic denervation
- NCV: Normal
Myofibrillar Myopathy with Early Respiratory Failure (MFM9; HIBM-ERF; HMERF; ADMERF)
Titin (TTN) Chromosome 2q31.2; Dominant or Sporadic
- Nosology
- Hereditary IBM with Early Respiratory Failure
- Distal myopathy with Early Respiratory Failure
- Myofibrillar myopathy with Early Respiratory Failure
- Edstrom myopathy
- Myopathy with Proximal Weakness, Early Respiratory Failure & Cytoplasmic aggregates
- Necklace body myopathy
- Epidemiology: > 30 families
- Genetics
- TTN mutations
- Missense
- Common: Cys31712Arg; Cys30071Arg (British founder mutation)
- Other: W30088 (Hotspot); P30091L; N30145K; G30150 (Hotspot); R32450W
- Location: Myosin binding (Fibronectin; FN3 119 domain) A-band; Exons 343-344
- Commonly private
- May be de novo
- Missense
- TTN mutations
- Titin protein
- Clinical
- Onset: Variable
- Age: 12 to 71 years; 4th & 5th decade most common; Mean 35 to 42 years
- Weakness
- Legs: Most common
- Patterns: Symmetric; Foot dorsiflexion; Respiratory; Proximal
- Weakness: Variable patterns
- Patterns
- Distal 30%
- Proximal 40%
- Other 30%: Distal + Proximal
- Legs > Arms
- Legs: Distal & Proximal; Anterior tibial
- Arms: Wrist flexion & extension; Deltoid; May be diffuse
- Trunk: Severe weakness common
- Neck flexors
- Ankle extension: Strong
- Face: Mild in some patients
- Symmetric (90%)
- Progression
- Slow
- Cane & occasionally wheelchair needed after 5 to 15 years
- Weakness: Proximal legs; Shoulders; ? Quadriceps sparing
- Nocturnal non-invasive ventilatory support
- Patterns
- Respiratory failure
- VC & FEV1 < 75% of predicted in most patients at presentation
- Course: Progressive
- Muscle hypertrophy: Posterior leg (Calf)
- Contractures: None
- Cardiac
- Conduction Δ (32%)
- Mild cardiomyopathy (18%)
- Onset: Variable
- Laboratory
- Serum CK: 65 to 966
- EMG: Myopathic; Irritable
- Nerve conduction studies: Normal
- MRI: Muscle
- Proximal legs
- Selective early involvement: Semitendinosus & Obturator externus
- Proximal more than distal involvement in individual muscles
- Adductor longus spared
- Distal legs
- Most involvement: Antero-Lateral; Tibialis anterior
- Relative sparing: Gastrocnemius & Soleus
- Shoulder girdle
- Moderate involvement: Supraspinatus, Infraspinatus, Serratus anterior, Subscapularis & Trapezius
- Proximal legs
- Muscle pathology
- Fiber size: Varied
- Myofibrillar pathology: Cytoplasmic aggregates
- Contain: Actin; Desmin
- In type I muscle fibers
- Myofibrillar pathology
- Not typical Cytoplasmic bodies
- Eosinophilic inclusions
- Congophilic
- Variably contain: β amyloid, desmin, SMI-31 binding
- Cytoplasmic bodies (95%)
- Stain for F-actin (Phalloidin)
- “Necklace” pattern in muscle fibers [rx]
- Muscle fiber splitting: With more severe weakness
- Vacuoles (50%): Rimmed, blue; With more severe weakness
- Fiber types: Type 1 predominance (50%)
- Internal nuclei
- No necrosis or inflammation
- Calpain-3: Reduced on Western blot
- Ultrastructure
- Z-line streaming
- Thin filaments & Dense material related to Z-discs
Myopathy with Ringed muscle fibers [rx]
- Inheritance: Sporadic
- Clinical features
- Onset: 3rd decade
- Weakness: Proximal (quadriceps) + Ankle dorsiflexion
- Progression: Moderate 1 to 5 years
- Lab
- Serum CK: Normal
- EMG: Irritable myopathy
- Muscle Pathology
- Myopathic: Fiber size variation; Increased connective tissue; Central nuclei
- Rings in fibers: Outer sarcoplasmic pad; Middle annular myofibrils; Center normal
Distal Myopathy: MPD3 [rx]
Autosomal Dominant
- Genetics: Two possible loci 8p22-q11 & 12q13-q22
- Epidemiology: Single Finnish family
- Onset
- Age: 32 to 45 years
- The clumsiness of hands or legs
- Weakness
- Legs
- Distal
- Anterior & Posterior
- Muscles involved: TA, EDL, Gastrocnemius, Gluteus medius; TFL
- Arms: Hands
- Distal
- Abductor pollicis; Opponens policis; 1st Dorsal interossei; Abductor digiti minimi
- Asymmetric
- Intrafamilial variability
- Course: Progressive
- Over years
- To more proximal limbs: Forearm, Triceps, Infraspinatus, Proximal legs
- Patients remain ambulatory
- Legs
- Laboratory
- EMG: Myopathic
- Serum CK: Normal or Slightly elevated
- Muscle biopsy
- Myopathy: Severe; Endomysial fibrosis; Fiber size variation
- Rimmed vacuoles
- Cytoplasmic inclusion bodies
Distal myopathy with spared anterior leg muscles (William’s myopathy) (MPD4) [rx]
Filamin C (Filamin 2; FLNC) ; Chromosome 7q32.1; Dominant
-
- Epidemiology: Australian & Italian families
- Genetics
- Missense mutations
- In actin-binding domain
- Met251Thr, Ala193Thr
- Allelic with
- Myofibrillar myopathy
- Distal myopathy with upper limb predominance
- Missense mutations
- Filamin C protein
- Clinical
- Variable within the family: Some affected members are asymptomatic
- Onset
- Age: 0 to 30 years
- Weakness
- Muscle discomfort
- Weakness
- Symmetric
- Distal
- Arms + Legs
- Arms: Forearm pronators, Finger flexors, Intrinsic hand muscles
- Legs: Ankle evertors, Plantar-flexors (Calf atrophy)
- Differential diagnosis: LGMD 2B
- Sparing: Anterior leg; Posterior arm
- Muscle wasting: Distal
- Discomfort
- Type: Cramps; Deep pain
- Worse after exercise
- Tendon reflexes: Absent at ankles
- Systemic
- Cardiomyopathy: 2 patients
- No respiratory involvement
- Course
- Slowly progressive
- Patients remain ambulatory
- Laboratory
- Serum CK: Normal or Mildly elevated
- EMG: Myopathic
- MRI
- Involvement of posterior & lateral leg muscles
- Some asymmetry
- Muscle
- Varied fiber size: Small angular fibers
- Internal architecture: Irregular in some biopsies
- No myofibrillar aggregates, vacuoles or inflammation
- Dysferlin normal
- FLNC variant syndrome: Distal myopathy with upper limb predominance [rx]
- Epidemiology: Bulgarian families, 13 patients
- FLNC mutations
- Stop: c.5160delC frameshift deletion; p.Phe1720Leufs*63
- Missense: Actin binding domain; p.Ala193Thr, p.Met251Thr
- Mechanisms: Haploinsufficiency of filamin C
- Inheritance: Dominant
- Penetrance: Partial
- Clinical
- Onset
- Age: 20 to 54 years
- Weakness: Fingers
- Walking difficulty: Steppage gait
- Weakness
- Distal > > Proximal
- Arms before Legs in some
- Finger extensors & Interossei
- Atrophy: Distal arms & legs
- Sensory: Loss in 40%
- Onset
- Other
- Pes cavus (20%)
- Hypertension (30%)
- Cardiomyopathy (10%)
- Laboratory
- Serum CK: Normal to 6x high
- NCV: CMAP amplitude reduced
- EMG: Myopathic
- Muscle
- Varied fiber size
- Necrosis
- Pyknotic nuclear clumps
- Type I predominance
- No or Few myofibrillar aggregates
- Ultrastructure: Myofibrillar disorganization
Distal nebulin myopathy [rx]
Nebulin; Chromosome 2q23.3; Recessive
- Genetics
- Mutations: Missense; Often homozygous
- Different from Rod myopathy in which at least 1 mutation causes protein termination
- Allelic with: Rod myopathy
- Clinical
- Onset age: Child or Adult
- Weakness: Similar to MPD1 (Gowers-Laing myopathy)
- Distal
- Hanging big toe sign
- Extensor finger weakness: Index finger spared
- Neck flexors
- Slender stature
- Muscle
- Rods: None or Small
- Ultrastructure: Z-line streaming; Minor rod changes
Distal Myopathy 5 (MPD5; Rod Myopathy)
Adenylosuccinate synthase-like 1 (ADSSL1); Chromosome 14q32.33; Recessive
- Epidemiology
- Korean & Japanese families
- Japan: Most common nemaline rod myopathy [rx]
- Genetics
- Mutations: Compound heterozygous; D304N (c.910G>A), I350fs (c.1048delA), L407P (c.1220T>C)
- Common in Japan: c.781G>A; c.919delA
- ADSSL1 protein
- Location: High in skeletal muscle
- Muscle isozyme of adenylosuccinate synthase
- Conversion of inosine monophosphate (IMP) to adenosine monophosphate (AMP): Catalyzes initial reaction
- Clinical
- Onset age: 5 to 8 years
- Weakness
- Early: Diffuse
- Distal > Diffuse
- Legs > Arms
- Quadriceps: 4th decade
- Face: Common
- Neck
- Dysphagia (38%)
- Respiratory
- Muscle size: Mild atrophy
- Sensory: Normal
- Disease course: Slow progression; Remain ambulant
- Cardiomyopathy, Hypertrophic
- Laboratory
- Serum CK: 108 to 493
- Muscle MRI
- Lower extremity
- General: Hyperintense signal in lower leg muscles
- Posterior > Anterior
- Thigh
- Vastus lateralis (Periphery), Adductor, Biceps femoris
- Quadriceps: Involved later
- Spared: Rectus femoris; Sartorius; Semitendinous
- Leg: Soleus; Gastrocnemius
- Tongue & Masseter: Fat replacement
- Trunk: Neck & Upper thoracic
- Lower extremity
- Muscle pathology
- Fiber size: Varied
- Internal architecture: Internal nuclei; Splitting
- Rimmed vacuoles (50%): Few fibers
- Endomysial connective tissue: Increased
- Type I fiber predominance:? Fiber type groups
- ADSSL1 expression: Absent or Reduced
- Nemaline rods [rx]
- Lipid droplets (Type 1 fibers)
Cystinosis, Nephropathic
Cystinosin (CTNS) ; Chromosome 17p13.2; Recessive
- Genetics: Mutations
- General: Missense & Stop
- French-Canadians: 57-kb deletion
- CTNS protein
- Lysosomal membrane
- Clinical
- Frequency [rx]
- 30% to 40% of patients with cystinosis
- Similar frequency in patients with & without cysteamine treatment
- Onset
- Age: 1st year to Adult
- Failure to thrive: 1st year
- Skeletal
- Short stature
- Frontal bossing
- Hypophosphatemic rickets
- Contractures (15%): Hands
- Eyes: Retinopathy; Corneal cysteine crystals
- GI: Not frequent
- Hepatomegaly; Pancreatic insufficiency; Splenomegaly
- GI complaints related to Cysteamine treatment: Treat with protein pump inhibitor
- Renal
- Fanconi syndrome
- Renal failure: Transplant often necessary
- Endocrine
- Hypothyroidism, Primary
- Diabetes mellitus: Insulin-dependent
- Delayed puberty
- Skin
- Hypohidrosis
- Light hair pigmentation
- Cardiac: Coronary artery calcifications
- Muscle
- Weakness
- Distal > Proximal
- Hands (Thenar & Hypothenar; Grip) > Feet
- Proximal muscles involved: Neck flexion; Arm abduction; Hip flexion
- Dysphagia (30% to 60%)
- Respiratory
- Face (10%)
- Wasting
- Weakness
- CNS: Visuo-spatial processing defect
- Treatment
- Replacement of renal losses
- Cystine-depleting agents: Cysteamine
- Frequency [rx]
- Laboratory
- Diagnosis: Leukocyte cystine measurement
- Urine: Proteinuria; Glucosuria; Microscopic hematuria
- Blood: Hyponatremia; Hypokalemia; Hypophosphatemia; Hyperlipidemia
- Carnitine deficiency
- Aminoaciduria, Generalized
- White blood cell cystine: Elevated
- Brain: Cerebral atrophy
- Muscle pathology
- Muscle fiber size: Varied
- Vacuoles: Rimmed; Mildly acid phosphatase positive
- Aggregates: AMPDA+
Distal weakness, Early-onset [rx]
Kelch-like homologue 9 (KLHL9) ; Chromosome 9p22; Dominant
- Nosology: Maybe distal myopathy or predominantly motor neuropathy
- Epidemiology: German family
- Genetics
- Mutation: Missense; L95F
- KLHL9 protein
- Complexes with Culllin 3
- Ubiquitin-dependent protein degradation pathway
- Clinical
- Onset age: 8 to 16 years
- Weakness
- Hands: Intrinsic muscles
- Legs: Distal
- Proximal: Normal
- Atrophy: Anterior tibial
- Contractures: Ankles
- Sensory loss
- Distal
- Arms & Legs
- Later in disease course
- Course
- Very slow progression
- Remain ambulant
- Laboratory
- Serum CK: 110 to 1400; Usual 150 to 260
- NCV
- Motor: Velocities normal; Distal latency occasionally long
- Sensory: Normal
- EMG: Distal fibrillations & Polyphasic large potentials
- Muscle biopsy: Varied fiber size
- MRI: Atrophy of distal leg muscles
dHMN: Distal Weakness, Hoarseness, Hearing loss (PNMHH)
Myosin heavy chain 14, non-muscle (MYH14) ; Chromosome 19q13.33; Dominant
- Epidemiology: Korean & North American families
- Genetics
- Mutation: Missense; Arg941Leu (c.2822G>g;T); In tail domain
- Allelic with: Deafness, autosomal dominant 4 (DFNA4)
- Contains microRNA, miR-499
- MYH14 protein
- Myosin: Non-muscle
- Locations: Heart, Slow muscles, Extraocular (EO) muscles; GI tract; Renal
- Myosin disorders
- Clinical
- Onset age: 4 to 23 years
- Weakness
- Distal: Occasionally also proximal
- Legs > Arms
- Symmetric
- Slow progression over decades
- Hoarseness (50%)
- Sensory loss: None
- Tendon reflexes: Variable
- Foot deformity (50%)
- Hearing loss (30% to 100%): Onset after weakness
- Cardiac: Normal
- Laboratory
- Serum CK: Normal to mildly high (< 2.5-fold high)
- EMG: Denervation, More distal
- Fibrillations
- Motor unit potentials: Large
- Recruitment: Reduced
- NCV
- Velocities: Normal
- CMAP amplitudes: Small
- SNAPs: Normal
- Muscle biopsy
- Fiber type grouping
- Grouped atrophy
- Ultrastructure: Abnormal mitochondria; Paracrystalline inclusions
Intellectual Disability
NOL1/NOP2/SUN domain family, member 2 (NSUN2); Chromosome 5p15.31; Recessive
- Epidemiology: Pakistan & Iran families
- Mutation: Homozygous; Missense; Gly679Arg
- NSUN2 protein
- RNA Methyltransferase
- Catalyzes the formation of 5-methylcytosine at C34 of tRNA-leu(CAA)
- Role in spindle assembly during mitosis & chromosome segregation
- Localization: Nucleolus
- Clinical
- CNS
- Intellectual disability
- IQ: 40 to 50
- Developmental delay: Motor; Speech
- Upper motor neuron
- Muscle tone: Increased
- Tendon reflexes: Brisk
- Morphology
- Face: Long; Pointed nose & chin
- Microcephaly
- Fingers: Tapering
- Height & Weight: Low
- Feet: Pes cavus; Abnormal toe separation
- Strabismus
- Distal myopathy: Not well documented
- CNS
- Laboratory
- Head CT: Normal
- Serum CK: Mildly high in 2 patients
Myopathy/Neuropathy [rx]
DNAJ/HSP40 homolog, subfamily B, member 5 (DNAJB5); Chromosome 9p13.3; Dominant
- Epidemiology: 1 patient
- Genetics
- Mutation: p.P15S
- DNAJB5 protein
- DNAJ family
- Other DNAJ disorders
- Clinical
- Onset age: 20 years
- Myoclonus
- Muscle
- Weakness
- Atrophy: Distal
- Laboratory
- NCV: Median motor 52 m/sec; Median CMAP 6 mV
- EMG: Spontaneous activity; Motor units small or large
Syndromes with Neuropathy & Myopathy
- Systemic disorders
- Paraneoplastic (with weight loss > 15%)
- Neuropathy: Distal; Sensory > Motor
- Myopathy: Proximal with type II muscle fiber atrophy
- Metabolic
- Uremia
- Acromegaly
- Immune
- Collagen vascular disorders: Sjögren
- Sarcoid
- Graft vs Host disease
- HIV Infection
- Myopathy: Inflammatory
- Neuropathy: Several types
- Paraneoplastic (with weight loss > 15%)
- Inclusion Body Myositis
- Debrancher deficiency
- HMSN: BAG3
- Lamin A/C mutations
- Congenital muscular dystrophy: Merosin (Laminin-α2) deficiency
- Dynamin-2
- Marinesco-Sjögren
- Mitochondrial: MNGIE; MERRF
- Motor neuropathy + Myopathy: VWA1
- Trifunctional protein deficiency
- TyrosinemiaHereditary
- Drugs & Toxins
- Amiodarone
- Chloroquine
- Chlorphenoxy
- Clofibrate: Risk factor – renal failure
- Colchicine: Risk factor – renal failure
- Doxorubicin
- Eosinophilia-myalgia syndrome
- Ethanol: Risk factor – fasting
- Hydroxychloroquine
- Organophosphates
- Perhexiline
- Vincristine
Causes of Distal Myopathy and Dysferlinopathy
The distal myopathies are inherited as either autosomal dominant or recessive traits. Genetic diseases are determined by the combination of genes for a particular trait that is on the chromosomes received from the father and the mother.
Dominant genetic disorders occur when only a single copy of an abnormal gene is necessary for the appearance of the disease. The abnormal gene can be inherited from either parent or can be the result of a new mutation (gene change) in the affected individual. The risk of passing the abnormal gene from affected parent to offspring is 50% for each pregnancy regardless of the sex of the resulting child.
Autosomal recessive genetic disorders occur when an individual inherits an abnormal gene for the same trait from each parent. If an individual receives one normal gene and one gene for the disease, the person will be a carrier for the disease, and usually will not show symptoms. The risk for two carrier parents to both pass the defective gene and, therefore, have an affected child is 25% with each pregnancy. The risk to have a child who is a carrier like the parents is 50% with each pregnancy. The chance for a child to receive normal genes from both parents and be genetically normal for that particular trait is 25%. The risk is the same for males and females.
The distal myopathies are caused by a deficiency or lack of specific proteins that play an essential role in the proper function and health of muscle cells.
Laing distal myopathy is caused by mutations in the beta cardiac myosin (MYH7) gene located on the long arm (q) of chromosome 14 (14q12). The MYH7 gene contains instructions to create (encode) the muscle protein, myosin. Chromosomes, which are present in the nucleus of human cells, carry the genetic information for each individual. Human body cells normally have 46 chromosomes. Pairs of human chromosomes are numbered from 1 through 22 and the sex chromosomes are designated X and Y. Males have one X and one Y chromosome and females have two X chromosomes (in most cases). Each chromosome has a short arm designated “p” and a long arm designated “q”. Chromosomes are further sub-divided into many bands that are numbered. For example, “chromosome 14q12” refers to a specific band on the long arm of chromosome 14. The numbered bands specify the location of the thousands of genes that are present on each chromosome. Laing distal myopathy is inherited as an autosomal dominant trait.
Udd distal myopathy is caused by mutations of the titin (TTN) located on the long arm of chromosome 2 (2q24.3). The TTN gene encodes the muscle protein, titin, found in both skeletal and heart (cardiac) muscles. Udd distal myopathy is inherited as an autosomal dominant trait.
Inclusion body myopathy type 2 (DMRV) is caused by mutations of GNE gene located on the short arm of chromosome 9 (9p12-p11). The GNE gene encodes the protein UDP-N-acetylglucosamine-2-epimerase/N-acetylmannosamine kinase. IBM2 is inherited as an autosomal recessive trait.
Miyoshi myopathy is caused by mutations of the dysferlin (DYSF) gene located on the short arm of chromosome 2 (2p13.3-p13.1). Miyoshi myopathy is inherited as an autosomal recessive trait.
Researchers have linked other forms of distal myopathy to specific chromosomes, but have not yet identified the causative genes. Welander distal myopathy has been linked to the short arm of chromosome 2 (2p13). Distal myopathy with vocal cord and pharyngeal signs has been linked to the long arm of chromosome 5 (5q). Distal myopathy 3 has been linked to the short or long arm of chromosome 8 (8p22-q12) or the long arm of chromosome 12 (12q13-q22). These three forms of distal myopathy are inherited as autosomal dominant traits.
Symptoms of Distal Myopathy and Dysferlinopathy
- Ankle dorsiflexion and finger extension weakness, as well as neck flexion weakness were common in our patients
- Abnormal, sometimes waddling, walk
- Joints that are fixed in a contracted position (late in the disease)
- Large and muscular-looking calves (pseudohypertrophy), which are not actually strong
- Loss of muscle mass, thinning of certain body parts
- Shoulder weakness
- Weakness of the muscles in the face (later in the disease)
- Weakness in the muscles of the lower legs, feet, lower arms, and hands (later in the disease)
- Chronic respiratory infections precipitated by weakness in the smooth muscle of the bronchioles.[rx]
- Impotence caused by gonadal atrophy, which is characteristically associated with myotonic dystrophy.[rx]
- It is common to possess dysphagia, which is esophageal muscle involvement.[rx]
- Myotonia is a term that describes the inability to relax muscles, which classically indicating as an inability to loosen one’s grip or release a handshake.[rx]
- As a pediatric disease, parents will often complain that their child is clumsy or becomes extremely weak quickly.[rx]
- The Gower sign is when subjects try to stand from a supine position, they march their hands and feet to each other).[rx]
- Weakness and stiffness of distal muscles are usually the presenting symptoms in adolescents with myotonic dystrophy.[rx]
-
Proximal muscle weakness (pelvic and/or shoulder girdle) with early-onset (age <12 years), adult-onset, or late-onset (age >30 years)
-
Symmetric atrophy and wasting of proximal limb and trunk muscles; calf hypertrophy is rarely and sometimes only transiently present [Fardeau et al 1996].
-
Scapular winging, scoliosis, Achilles tendon contracture, and other joint contractures (including hip, knee, elbow, finger, and spine)
-
Waddling gait; tip-toe walking; difficulty in running, climbing stairs, lifting weights, and getting up from the floor or from a chair
-
Sparing of facial, ocular, tongue, and neck muscles
-
Elevated creatine kinase (CK) concentrations, especially in childhood or adolescence, with or without overt muscle symptoms
-
Absence of cardiomyopathy and intellectual disability
Clinical findings
-
Initial weakness of the great toe and ankle dorsiflexors – eventually leading to a high-stepping gait and secondary tightening of the Achilles tendon. Onset is usually before age five years, but maybe later (into the 6th decade).
-
Subsequent weakness of the finger extensors – (onset from months to 3 decades after lower-limb weakness), with sparing of the thumb, and often accompanied by an action tremor of the hands
-
Mild involvement of the facial musculature – particularly of the orbicularis oculi and oris muscles
-
Early weakness of neck flexion in most families
-
The very slow progression of weakness – with gradual involvement of the proximal leg and trunk muscles. With early-onset, a wheelchair may eventually be required for mobility.
- Lower leg weakness – follows a typical sequence: initially dorsiflexion of the ankle and the great toe is affected and leads to a high-stepping gait, dropped big toe, and secondary tightening of the Achilles tendon. Early development of anterior compartment weakness has led to the marked tightening of the Achilles tendon bilaterally, with the affected individual unable to place his heels on the ground.
- Weakness of finger extensors – develops between months and several decades after the onset of leg weakness [Lamont et al 2014]. The third and fourth fingers appear to be more severely affected than the other fingers, although any of the fingers can be affected. The thumb is spared. Weakness of the finger extensors is often accompanied by a postural and action tremor of the hands. Individual with Laing distal myopathy attempting to extend her second to fifth fingers. Note marked weakness of third- and fourth-finger extension.
- Mild facial weakness – is often present, leading to the inability to bury the eyelashes completely when closing the eyes tightly, and the inability to keep the lips pursed against resistance. One affected individual has a mild Bell phenomenon.
- Weakness of neck flexion – seen in all affected individuals, is usually early in onset, though the weakness of neck flexion did not manifest in one family until the sixth decade. In most affected individuals and sites, the weakness is symmetric.
- Proximal weakness – After distal weakness has been present for more than ten years, mild proximal weakness occurs, with a slight Trendelenburg gait and mild scapular winging. Axial musculature may be mildly weak as well (manifesting as, e.g., inability to do a sit-up).
- Progression – is usually extremely slow; however, in one person the weakness became generalized and a wheelchair was required for mobility by age 15 years [Lamont et al 2014].
- Spinal manifestations – which can include kyphoscoliosis, spinal rigidity, and spinal extensor muscle contractures, occur in one-third of individuals and can vary within a family [Feinstein-Linial et al 2016, Fiorillo et al 2016]. Severe axial involvement with scoliosis, cervical hyperextension, and bent spine has been described [Dabaj et al 2018].
- Cardiac problems – are common. In their review of 88 affected individuals from 22 families, Lamont et al [2014] reported cardiac involvement ranging from hypertrophic cardiomyopathy with onset from birth to the third decade of life to dilated cardiomyopathy with onset from birth to the second decade of life. In an earlier report, a father and son in one family developed a dilated cardiomyopathy for which no other cause was found [Hedera et al 2003].
- Respiratory issues – present in approximately 40% of individuals in the form of reduced forced vital capacity, are not usually life-threatening [Lamont et al 2014]. Sleep apnea or sleep-related respiratory insufficiency may develop [Yu et al 2020].
- CNS involvement – with white matter lesions and epilepsy has been described in a single-family including three of 14 family members over three generations [Lefter et al 2015].
Diagnosis of Distal Myopathy and Dysferlinopathy
History and Physical
It includes detailed birth history, medical/surgical history, and 3-generation family history. Clinical features associated with myotonic dystrophy are as follow:[rx]
-
Prenatal – polyhydramnios, reduced fetal movements, preterm delivery <36 weeks, small for gestational age.
-
Neonatal – hypotonia, hyporeflexia, muscle weakness (distal > proximal), neck muscle weakness (flexion), myopathic facies (ptosis, facial diplegia, atrophy of temporalis muscles, tent-shaped mouth), contractures, arthrogryposis, scoliosis, talipes equinovarus, visual impairment (cataract, lens opacification), respiratory distress, weak cough, sleep apnea, pulmonary hypoplasia, bronchopulmonary dysplasia, raised right hemidiaphragm, pneumothorax, recurrent infections/otitis media, aspiration pneumonia, feeding and sucking difficulties, gastroparesis, GERD, constipation/diarrhea, fecal incontinence, increased sensitivity to anesthesia (due to respiratory muscle compromise and central dysregulation of breathing), cardiac conduction disturbances, valve defects (mitral), and early death.
-
Infancy and childhood, age 1 to 10 years – usually, they are able to walk with improvement in motor function; however, progressive weakness restarts in the 2nd decade. Myotonia (by 10 years of age), intellectual disability (50-60%), autism, ADHD, psychiatric disorders, vision problems (hyperopia, astigmatism, cataract), excessive daytime sleepiness, cardiac and endocrine complications.
-
Respiratory – respiratory difficulties are found in 50% of neonates and are the main cause of neonatal mortality and used to distinguish between mild and severe CDM.
-
Musculoskeletal – proximal muscle weakness in DM1 indicates a poor prognosis. The biphasic course in myotonic dystrophy shows improved/stable disease until adolescence/young adult with gradual deterioration. Complications of muscle weakness may include scoliosis and contractures producing foot deformity and toe walking. Bulbar muscle weakness may produce swallowing, speech, and language difficulties.
-
Cognition – Cognitive impairment is one of the most common and challenging manifestations of childhood DM1. CDM patients are most affected, with IQ range 40 to 80, mean 70 (average normal 100). Cognitive impairment correlates with the severity of weakness, size of CTG repeat, and maternal transmission.
-
Sleep – excessive sleep disorder and sleep apnea may adversely affect learning, memory, high-level cognitive processing, and physical functioning, exacerbating psychomotor and cognitive delays.
-
Psychosocial – 50% of children have psychiatric diseases (phobia, depression, anxiety), and ADHD. Avoidant personality, apathy, and autistic features may be present.
-
Cancer – There is an increased risk of cancer in patients with type 1 myotonic dystrophy, including thyroid, uterine, choroidal melanoma, colon, testicular, prostate, and basal cell cancer.
-
Other – features of adult “classic” myotonic dystrophy are not evident in childhood, including cataracts, significant cardiac disorders, and diabetes mellitus. Lens pathology is evident in 40% and can predict future cataracts. Conduction disturbances observed on ECG, or valve abnormalities may be symptomatic. Hypothyroidism, hypogonadism, growth hormone abnormalities, and androgen insensitivity are rare. In contrast, testicular atrophy and infertility are common in CDM males, as are irregular menses in CDM females.
Physical Exam
- Vital signs, weight, height, and head circumference measurements are essential. Comprehensive neonatal exam looking for dysmorphic features, contractures, scoliosis, pulmonary and cardiac evaluation for abnormal chest rise, or murmurs.
- Abdominal exam for organomegaly, back for scoliosis, the musculoskeletal system for contractures, detailed neurological exam assessing mental status, cranial nerves (myopathic facies, ptosis, dysphagia, weak cry/cough/gag, respiratory failure), motor (axial and appendicular hypotonia, frog-like posture, decreased movements), reflexes, Babinski response, sensory, coordination and primitive reflexes.
- Examine mother (myopathic facies, shake hand as myotonia prevents the prompt release of grip, percussion with a reflex hammer, by tapping thenar, wrist extensor will produce involuntary muscle contraction with a delay in relaxation, called percussion myotonia).[rx]
Laboratory Tests
When myotonic dystrophy is suspected after history and examination, creatinine kinase level followed by dystrophin gene deletion analysis or muscle biopsy with dystrophin antibody staining is the mainstay of the laboratory studies to confirm the diagnosis.[rx] However, in most instances, muscle biopsy is avoided, and genetic testing is confirmatory.
- Blood and urine tests – can detect defective genes and help identify specific neuromuscular disorders. On microscopic examination, the hallmark of congenital muscular dystrophy is ongoing myofiber necrosis and regeneration. Active muscle fiber necrosis and a cluster of basophilic regenerating fibers are more prominent at a younger age. In contrast, myofiber splitting with necrosis, increased internal nuclei, fiber hypertrophy, fatty replacement, and endomysia fibrosis are conspicuous in older age.[rx][rx]
- Creatine kinase – is an enzyme that leaks out of the damaged muscle. Elevated creatine kinase levels may indicate muscle damage, including some forms of congenital muscular dystrophy before physical symptoms become apparent. A creatine kinase level (CK), aldolase, alanine aminotransferase (ALT), and aspartate aminotransferase (AST), nerve conduction studies and EMG should be considered. However, creatine kinase levels may vary from being completely normal to significantly elevated based on phenotype. An elevated CK, aldolase level, usually signifies a dystrophic process.
- Myoglobin – is measured when injury or disease in skeletal muscle is suspected. Myoglobin is an oxygen-binding protein found in cardiac and skeletal muscle cells. High blood levels of myoglobin are found in people with congenital muscular dystrophy.
- Polymerase chain reaction (PCR) – can detect some mutations in the dystrophin gene. Also known as molecular diagnosis or genetic testing, PCR is a method for generating and analyzing multiple copies of a fragment of DNA.
- Serum electrophoresis – is a test to determine quantities of various proteins in a person’s DNA. A blood sample is placed on specially treated paper and exposed to an electric current. The charge forces the different proteins to form bands that indicate the relative proportion of each protein fragment. [rx]
- Exercise tests – can detect elevated rates of certain chemicals following exercise and are used to determine the nature of congenital muscular dystrophy or other muscle disorders. Some exercise tests can be performed bedside while others are done at clinics or other sites using sophisticated equipment. These tests also assess muscle strength. They are performed when the person is relaxed and in the proper position to allow technicians to measure muscle function against gravity and detect even slight muscle weakness. If weakness in respiratory muscles is suspected, respiratory capacity may be measured by having the person take a deep breath and count slowly while exhaling.[rx]
- Genetic testing – looks for genes known to either cause or be associated with inherited muscle disease. DNA analysis and enzyme assays can confirm the diagnosis of certain neuromuscular diseases, including congenital muscular dystrophy. Genetic linkage studies can identify whether a specific genetic marker on a chromosome and a disease are inherited together. They are particularly useful in studying families with members of different generations who are affected. An exact molecular diagnosis is necessary for some of the treatment strategies that are currently being developed. Advances in genetic testing include whole-exome and whole-genome sequencing, which will enable people to have all of their genes screened at once for disease-causing mutations, rather than have just one gene or several genes tested at a time. Exome sequencing looks at the part of the individual’s genetic material, or genome, that “code for” (or translate) into proteins. [rx]
- Molecular Genetic Testing (first line) – targeted analysis of the DMPK gene appears positive for a heterozygous pathogenic variant in nearly 100% of affected individuals. If the diagnosis is uncertain, the panel can be completed. The multigene panel can include testing for the DMPK CTG repeat expansion and other disorders of interest, depending on the laboratory.
- Genetic counseling – can help parents who have a family history of congenital muscular dystrophy/ myotonic dystrophy determine if they are carrying one of the mutated genes that cause the disorder. Two tests can be used to help expectant parents find out if their child is affected.
- Amniocentesis – done usually at 14-16 weeks of pregnancy, tests a sample of the amniotic fluid in the womb for genetic defects (the fluid and the fetus have the same DNA). Under local anesthesia, a thin needle is inserted through the woman’s abdomen and into the womb. About 20 milliliters of fluid (roughly 4 teaspoons) is withdrawn and sent to a lab for evaluation. Test results often take 1-2 weeks.
- Chorionic villus sampling, or CVS – involves the removal and testing of a very small sample of the placenta during early pregnancy. The sample, which contains the same DNA as the fetus, is removed by a catheter or a fine needle inserted through the cervix or by a fine needle inserted through the abdomen. The tissue is tested for genetic changes identified in an affected family member. Results are usually available within 2 weeks. [rx]
- Alanine Aminotransferase (ALT, SGPT) – The normal range in males is 10 to 40 U/L. The normal range in females is 8 to 35 U/L; it is elevated in muscular dystrophy.[rx]
- Aldolase (Serum) – The normal range is 0 to 6 U/L. It is elevated in muscular dystrophy but decreases in later stages of muscular dystrophy.[rx]
- Arterial Blood Gases (ABG) – Normal ranges: PO2 is 75 to 100 mmHg; PCO2 is 35 to 45 mm Hg; HCO3- is 24 to 28 mEq/L; pH is 7.35 to 7.45. Respiratory acidosis can develop if there are defects in muscles involved in respiration.[rx]
- Aspartate Aminotransferase (AST) – Normal ranges from 0 to 35 U/L. Elevated in muscular dystrophy.[rx]
- Creatine Kinase (CK, CPK) and Creatine Kinase Isoenzymes (CK-MB and CK-MM) – Normal ranges from 0 to 130 U/L. Elevated in muscular dystrophy (hyperkalemia).[rx] The serum enzymes, especially creatine phosphokinase (CPK), is increased to more than ten times normal, even in infancy and before the onset of weakness.[rx][rx] Serum CK levels are invariably elevated between 20 and 100 times normal in Duchenne muscular dystrophy.[rx] The levels are abnormal at birth, but values decline late in the disease because of inactivity and loss of muscle mass.[rx] Elevated CPK levels at birth are diagnostic indicators of Duchenne muscular dystrophy and congenital muscular dystrophy.[rx]
- Lactate Dehydrogenase (LDH) – Normal ranges from 50 to 150 U/L. Elevated in muscular dystrophy. LDH 4: 3 to 10%, LDH 5: 2 to 9%.[rx]
- Urinalysis (UA) – Glucose in urine is commonly associated with muscular dystrophy due to the high incidence of diabetes mellitus within this population.[rx] Myoglobinuria may also be present.[rx]
- Liver function tests – for transaminases, pulmonary function tests, and spinal radiographs to follow the progression of scoliosis are also important but less important. Elevations in the hepatobiliary enzymes alkaline phosphatase, gamma-glutamyl transferase (GGT), serum aspartate aminotransferase, and serum alanine aminotransferase can be seen. Elevations do not correlate with the severity of muscle weakness, disease duration, or serum levels of creatine kinase.[rx]
- Muscle imaging – Thigh and calf muscle MRIs were performed in all enrolled patients except patient III-1 (family A). The distributions of fatty infiltration were not uniform among different patients. For thigh muscles, vastus intermedius and adductor Magnus were severely affected in all the examined patients except patient III-1 (family C), in whom all thigh muscles were with diffusely mildly fatty infiltration. Other thigh muscles severely affected included semitendinosus in three patients, sartorius in two, semitendinosus in two, adductor longus in one, and gracilis in one. Rectus femoris was relatively preserved in all examined patients, while other muscles were affected differently. For calf muscles, the tibialis anterior and extensor hallucis longus were severely affected in all patients, while the soleus was severely affected in two. Other calf muscles were mildly affected or relatively preserved. Patient II-2 (family D) also did a lumbar MRI, which showed obvious fatty infiltration of paraspinal and other axial muscles.
- Genomic testing – When the diagnosis of UDM-TMD is not considered because an individual has atypical phenotypic features, comprehensive genomic testing (which does not require the clinician to determine which gene[s] are likely involved) is the best option. Exome sequencing is the most commonly used genomic testing method; genome sequencing is also possible. If exome sequencing is not diagnostic, exome array (when clinically available) may be considered to detect (multi)exon deletions or duplications that cannot be detected by sequence analysis.
- Single-gene testing – Sequence analysis of TTN detects small intragenic deletions/insertions and missense, nonsense, and splice-site variants; typically, exon or whole-gene deletions/duplications are not detected. Perform sequence analysis first. If no pathogenic variant is found gene-targeted deletion/duplication analysis be considered, although no intragenic deletions or duplications have been reported in this disorder.
-
A multigene panel – that includes TTN and other genes of interest is most likely to identify the genetic cause of the condition at the most reasonable cost while limiting identification of variants of uncertain significance and pathogenic variants in genes that do not explain the underlying phenotype.
-
(1) The genes included in the panel and the diagnostic sensitivity of the testing used for each gene vary by laboratory and are likely to change over time.
-
(2) Some multigene panels may include genes not associated with the condition discussed in this GeneReview.
-
(3) In some laboratories, panel options may include a custom laboratory-designed panel and/or custom phenotype-focused exome analysis that includes genes specified by the clinician.
-
(4) Methods used in a panel may include sequence analysis, deletion/duplication analysis, and/or other non-sequencing-based tests.
-
Radiographic Tests
- Magnetic Resonance Imaging (MRI) – Coronal T1 weighted MRI may confirm the nonuniform fatty atrophy.[rx] There will be a relatively normal sartorius. Lateral radiographs may show cavus foot deformity and diffuse osteopenia.[rx] The sagittal view will show diffuse fat replacement of the gastrocnemius & semimembranosus muscles. These changes contribute to the prominent calves typical of affected children.[rx]
- Computerized Tomography (CT) – Axial CT shows denervation hypertrophy of the tensor fascia lata. The muscle becomes enlarged with an increase in intramuscular fat.[rx]
- Brain MRI – may show ventricular dilatation, cortical atrophy, hypoplasia of the corpus callosum, and white matter abnormalities.[rx][rx][rx][rx]
Other Tests
- Chromosomal Analysis – DNA testing for common mutations and chromosomal analysis can now rule out Down syndrome, myotonic dystrophy, and other disorders. In both Becker and Duchenne dystrophies, and congenital muscular dystrophy, the DNA deletion size does not predict clinical severity.[rx] [rx]
- Electrocardiogram (ECG) – Often, patients will have annual echocardiograms to stay ahead of any developing cardiomyopathy. This study will demonstrate atrial and atrioventricular rhythm disturbances. The typical electrocardiogram shows an increased net RS in lead V1; deep, narrow Q waves in the precordial leads.[rx] A QRS complex too narrow to be right bundle branch block; and tall right precordial R waves in V1.[rx] Dominant R wave in lead V1 is the best clue to the actual diagnosis.[rx] Normal PR interval, QRS duration.
- Electromyography (EMG) – Allows assessment for denervation of muscle, myopathies, and myotonic dystrophy, motor neuron disease. EMG demonstrates features typical of myopathy.[rx] Clinical examination, electromyography changes are found in almost any muscle: waxing and waning of potentials termed the dive bomber effect.[rx]
- Electrodiagnostic (EDX) testing – has been the modality of choice for diagnosis prior to molecular testing. It has the capability to diagnose patients who are clinically asymptomatic or have subtle findings.[rx] Motor nerve conduction studies (NCS) show decreased amplitude with normal latency and normal conduction velocities. Sensory nerve conduction studies are typically normal. Electromyography (EMG) typically has normal insertional activity. Early recruitment with short duration and small amplitudes motor unit potentials are observed. Myotonic discharges are highly specific and consist of spontaneous discharges that have a waxing and waning of amplitude and frequency, typically from around 150/second to 20/second.[rx][rx] It is shown that evaluating distal muscles is more sensitive for detecting myotonic discharges than proximal muscles.[rx]
- Congenital genetic Testing – A definitive diagnosis of muscular dystrophy can be established with mutation analysis on peripheral blood leukocytes.[rx] Genetic testing demonstrates deletions or duplications of the dystrophin gene in 65% of patients with Becker dystrophy, which is approximately the same percentage as in Duchenne dystrophy, and congenital muscular dystrophy.[rx] [rx]
- Immunocytochemistry – A definitive diagnosis of muscular dystrophy can be established based on dystrophin deficiency in a biopsy of muscle tissue.[rx] Also, staining of muscle with dystrophin antibodies can demonstrate the absence or deficiency of dystrophin localizing to the sarcolemmal membrane.[rx] DIsease carriers may demonstrate a mosaic pattern, but dystrophin analysis of muscle biopsy specimens for carrier detection is not reliable.[rx]
- Immunofluorescence testing – can detect specific proteins such as dystrophin within muscle fibers. Following the biopsy, fluorescent markers are used to stain the sample that has the protein of interest.
- Electron microscopy – can identify changes in subcellular components of muscle fibers. Electron microscopy can also identify changes that characterize cell death, mutations in muscle cell mitochondria, and an increase in connective tissue seen in muscle diseases such as congenital muscular dystrophy. Changes in muscle fibers that are evident in a rare form of distal congenital muscular dystrophy can be seen using an electron microscope.[rx]
- Nerve conduction velocity test – measure the speed and strength with which an electrical signal travels along a nerve. A small surface electrode stimulates a nerve, and a recording electrode detects the resulting electrical signal either elsewhere on the same nerve or on a muscle controlled by that nerve. The response can be assessed to determine whether nerve damage is present. Repetitive stimulation studies involve electrically stimulating a motor nerve several times in a row to assess the function of the neuromuscular junction. The recording electrode is placed on a muscle controlled by the stimulated nerve, as is done for a routine motor nerve conduction study.[rx]
- Muscle Biopsy – The muscle biopsy shows muscle fibers of varying sizes as well as small groups of necrotic and regenerating fibers. Connective tissue and fat replace lost muscle fibers. Muscle biopsy usually shows nonspecific dystrophic features, although cases associated with FHL1 mutations have features of myofibrillar myopathy.[rx] Muscle biopsy shows muscle atrophy involving Type 1 fibers selectively in 50 percent of cases.[rx]
- Polysomnogram – Excessive daytime somnolence with or without sleep apnea is not uncommon. Sleep studies, noninvasive respiratory support (biphasic positive airway pressure [BiPAP]), and treatment with modafinil may be beneficial.[rx]
- DNA banking Test – is the storage of DNA (typically extracted from white blood cells) for possible future use. Because it is likely that testing methodology and our understanding of genes, allelic variants, and diseases will improve in the future, consideration should be given to banking the DNA of affected individuals.
- Slit Lamp – An examination for cataracts that may be present in patients with muscular dystrophy.[rx]
- Western Blot – A diagnosis of Duchenne dystrophy can also be made by Western blot analysis of muscle biopsy specimens, revealing abnormalities in the quantity and molecular weight of dystrophin protein. On Western blot, Becker muscular dystrophy individuals dystrophin levels will appear normal, although the protein itself is abnormal; this is in comparison to Duchenne muscular dystrophy affected individuals who have a significantly decreased dystrophin on Western blot.[rx]
-
Muscle histopathology – shows nonspecific myopathic or dystrophic changes, including variation in fiber size, increase in internal nuclei, increase in endomysial connective tissue, and necrotic fibers. Electron microscopy may reveal specific alterations in nuclear architecture [rx]. Inflammatory changes may also be found in LMNA-related myopathies including EDMD [rx]. Muscle biopsy is now rarely performed for diagnostic purposes because of the lack of specificity of the dystrophic changes observed.
-
Immunodetection of emerin – In normal individuals, the protein emerin is ubiquitously expressed on the nuclear membrane. Emerin can be detected by immunofluorescence and/or by western blot in various tissues: exfoliative buccal cells, lymphocytes, lymphoblastoid cell lines, skin biopsy, or muscle biopsy [rx].
-
In individuals with XL-EDMD, emerin is absent in 95% [rx].
-
In female carriers of XL-EDMD, emerin is absent in varying proportions in nuclei, as demonstrated by immunofluorescence. However, the western blot is not reliable in carrier detection because it may show either a normal or a reduced amount of emerin, depending on the proportion of nuclei expressing emerin.
-
In individuals with AD-EDMD, emerin is normally expressed.
-
-
Immunodetection of FHL1 – In controls, the three FHL1 isoforms (A, B, and C) are ubiquitously expressed in the cytoplasm as well as in the nucleus. The isoforms can be detected by immunofluorescence and/or western blot in fresh muscle biopsy or myoblasts, fibroblasts, and cardiomyocytes [rx].
-
In individuals with FHL1-related XL-EDMD, FHL1 is absent or significantly decreased [rx].
-
In female carriers of FHL1-related XL-EDMD, FHL1 is expected to be variably expressed.
-
- Immunodetection of lamins A/C – Lamins A/C are expressed at the nuclear rim (i.e., nuclear membrane) and within the nucleoplasm (i.e., nuclear matrix). Depending on the antibody used, lamins A/C can be localized to both the nuclear membrane and matrix or to the nuclear matrix only. However, this test is not reliable for confirmation of the diagnosis of AD-EDMD because in AD-EDMD lamins A/C is always present due to the expression of the wild-type allele at the nuclear membrane and in the nuclear matrix. Western blot analysis for lamin A/C may contribute to the diagnosis, but yields normal results in many affected individuals[rx].
- Radionuclide angiography – using MUGA (multi–gated acquisition) scan reveals the deteriorating ventricular function with reduction of the left ventricular ejection fraction followed by reduction of the right ventricle ejection fraction.
- Heart muscle biopsies – (taken from 2 individuals) showed increased interstitial fibrosis compatible with dilated cardiomyopathy [rx]. Oxidative staining was normal without focal oxidative defects or significant disarray of the cardiomyocyte structure, in contrast to the classic observation in hypertrophic cardiomyopathy.
- Heterozygotes – In contrast to individuals with heterozygous pathogenic variants in TTN associated with add distal myopathy, the heterozygous parents of individuals with Salih myopathy remain asymptomatic with no cardiac or muscle disorder
Treatment of Distal Myopathy and Dysferlinopathy
Clinicians should refer patients with muscular dystrophy to a clinic that has access to multiple specialties (e.g., physical therapy, occupational therapy, respiratory therapy, speech and swallowing therapy, cardiology, pulmonology, orthopedics, and genetics) designed specifically to care for patients with muscular dystrophy and other neuromuscular disorders in order to provide efficient and effective long-term care
Non-Pharmacological Treatment
- Assisted ventilation – is often needed to treat respiratory muscle weakness that accompanies many forms of myotonic dystrophy, especially in the later stages. Air that includes supplemental oxygen is fed through a flexible mask (or, in some cases, a tube inserted through the esophagus and into the lungs) to help the lungs inflate fully. Since respiratory difficulty may be most extreme at night, some individuals may need overnight ventilation. Many people prefer non-invasive ventilation, in which a mask worn over the face is connected by a tube to a machine that generates intermittent bursts of forced air that may include supplemental oxygen. Some people with myotonic dystrophy/congenital muscular dystrophy, especially those who are overweight, may develop obstructive sleep apnea and require nighttime ventilation. Individuals on a ventilator may also require the use of a gastric feeding tube.
- Supportive Bracing – This helps to maintain normal function as long as possible proper wheelchair seating is essential. Molded ankle-foot orthoses help stabilize gait in patients with foot drop.[rx] Lightweight plastic ankle-foot orthoses (AFOs) for footdrop are extremely helpful. Footdrop is easily treatable with AFOs.[rx] Bracing may be performed for function; for example, dorsiflexion of the feet with ankle-foot orthotics to prevent tripping or to provide support and comfort.[rx]
- Supportive Counseling – Some forms of muscular dystrophy/ myotonic dystrophy may be arrested for prolonged periods, and most patients remain active with a normal life expectancy.[rx] Thus, vocational training and supportive counseling are important to provide the information necessary to plan their future.
- Genetic Counseling — Genetic counseling is recommended.[rx] With X-linked inheritance, male siblings of an affected child have a 50% chance of being affected, and female siblings have a 50% chance of being carriers. If the affected individual marries and has children, all daughters will be carriers of this X-linked recessive disorder. Genetic counseling should be offered to the mother, female siblings, offspring, and any maternal relatives.
- Cell-based therapy – The muscle cells of people with congenital muscular dystrophy often lack a critical protein, such as dystrophin in congenital muscular dystrophy, myotonic dystrophy, or sarcoglycan in some of the limb-girdle myotonic dystrophy. Scientists are exploring the possibility that the missing protein can be replaced by introducing muscle stem cells capable of making the missing protein in new muscle cells. Such new cells would be protected from the progressive degeneration characteristic of congenital muscular dystrophy and potentially restore muscle function in affected persons.
- Gene replacement therapy – Gene therapy has the potential for directly addressing the primary cause of congenital muscular dystrophy by providing for the production of the missing protein. Hurdles to be overcome include determining the timing of the therapy (to possibly overcome the genetic defect), avoiding or easing potential immune responses to the replacement gene, and, in the case of myotonic dystrophy the large size of the gene to be replaced. For that myotonic dystrophy with central nervous system consequences (congenital muscular dystrophy and myotonic dystrophy), researchers are developing and fine-tuning gene therapy vectors (a way to deliver genetic materials to cells) that can cross the protective blood-brain barrier.
- Myoblast transplantation – A case series evaluating myoblast transplantation into the tibialis anterior in 3 male participants with BMD pretreated with cyclosporine A provided insufficient evidence to determine the efficacy of myoblast transfer in BMD.
- Neutralizing antibody to myostatin – A phase 1 randomized controlled study of a neutralizing antibody (MYO-029) to an endogenous inhibitor of muscle growth (myostatin) performed in 116 participants with different types of muscular dystrophies provided evidence that MYO-029 is probably safe and tolerable in patients with BMD, LGMD2A–E, and LGMD2I. The study was not designed to assess the efficacy or long-term safety.
- Growth hormone for BMD – A randomized study evaluating the effects of subcutaneous growth hormone (sGH) in 10 patients with BMD provided insufficient evidence to support or refute the use of sGH to improve cardiac and pulmonary function in patients with BMD.
- Hand training program in Welander distal myopathy – A case series of a hand training program in 12 patients with Welander distal myopathy provided insufficient evidence to support or refute the benefit of the exercise program.
- Endurance training – Two case series studying the effect of endurance training in 9 ambulatory patients with LGMD2I and 11 men with BMD provided insufficient evidence to determine the benefit of endurance training to improve maximal oxygen uptake, maximal workload, and other patient-reported outcomes.
- Strength training and aerobic exercise training – The evidence base regarding the effectiveness of rehabilitation management of muscular dystrophies is limited. However, the available evidence suggests that this population would benefit from strengthening and aerobic fitness training programs. Due to the muscle degeneration in muscular dystrophy, there may be some risk of exercise-induced muscle damage, myoglobinuria, and subsequent overwork weakness following supramaximal, high-intensity exercise. There have been several randomized or quasirandomized controlled trials comparing strength training programs, aerobic exercise programs, or both to non-training controls in patients with a variety of neuromuscular disorders
- Nutrition – Patients with muscular dystrophy may have difficulty receiving adequate oral intake due to dysphagia or the inability to feed themselves due to arm weakness. Maintaining adequate nutrition and body weight is important for optimizing strength, function, and quality of life. When oral intake is inadequate, other means of maintaining intake (e.g., gastrostomy or jejunostomy feeding tubes) may be needed to maintain optimal nutrition. There is evidence from related conditions (amyotrophic lateral sclerosis [ALS]) that maintenance of nutrition and bodyweight prolongs survival.
Supportive Physiotherapy
Treatment may include physical therapy, respiratory therapy, speech therapy, orthopedic appliances used for support, and corrective orthopedic surgery. Treatment includes supportive physiotherapy to prevent contractures and prolong ambulation.[rx] Maintaining function in unaffected muscle groups for as long as possible is the primary goal. Although activity fosters maintenance of muscle function, strenuous exercise may hasten the breakdown of muscle fibers.[rx]
- Physical therapy can help prevent deformities, improve movement, and keep muscles as flexible and strong as possible. Options include passive stretching, postural correction, and exercise. A program is developed to meet the individual’s needs. Therapy should begin as soon as possible following diagnosis before there is joint or muscle tightness.
- Passive stretching can increase joint flexibility – and prevent contractures that restrict movement and cause loss of function. When done correctly, passive stretching is not painful. The therapist or other trained health professional slowly moves the joint as far as possible and maintains the position for about 30 seconds. The movement is repeated several times during the session. Passive stretching on children may be easier following a warm bath or shower. [rx]
- Regular, moderate exercise -can help people with congenital muscular dystrophy maintain range of motion and muscle strength, prevent muscle atrophy, and delay the development of contractures. Individuals with a weakened diaphragm can learn coughing and deep breathing exercises that are designed to keep the lungs fully expanded.
- Postural correction – is used to counter the muscle weakness, contractures, and spinal irregularities that force individuals with congenital muscular dystrophy into uncomfortable positions. When possible, individuals should sit upright, with feet at a 90-degree angle to the floor. Pillows and foam wedges can help keep the person upright, distribute weight evenly, and cause the legs to straighten. Armrests should be at the proper height to provide support and prevent leaning.
- Support aids – such as wheelchairs, splints and braces, other orthopedic appliances, and overhead bed bars (trapezes) can help maintain mobility. Braces are used to help stretch muscles and provide support while keeping the person ambulatory. Spinal supports can help delay scoliosis. Night splints, when used in conjunction with passive stretching, can delay contractures. Orthotic devices such as standing frames and swivel walkers help people remain standing or walking for as long as possible, which promotes better circulation and improves calcium retention in bones. [rx]
- Repeated low-frequency bursts of electrical stimulation – to the thigh muscles may produce a slight increase in strength in some boys with congenital muscular dystrophy, though this therapy has not been proven to be effective. [rx]
- Occupational therapy – may help some people deal with progressive weakness and loss of mobility. Some individuals may need to learn new job skills or new ways to perform tasks while other persons may need to change jobs. Assistive technology may include modifications to home and workplace settings and the use of motorized wheelchairs, wheelchair accessories, and adaptive utensils.[rx]
- Speech therapy – may help individuals whose facial and throat muscles have weakened. Individuals can learn to use special communication devices, such as a computer with a voice synthesizer.[rx]
- Dietary changes – have not been shown to slow the progression of congenital muscular dystrophy. Proper nutrition is essential, however, for overall health. Limited mobility or inactivity resulting from muscle weakness can contribute to obesity, dehydration, and constipation. A high-fiber, high-protein, low-calorie diet combined with recommended fluid intake may help. Feeding techniques can help people with congenital muscular dystrophy who have a swallowing disorder and find it difficult to pass from or liquid from the mouth to the stomach. [rx]
Medication
There is no specific treatment to stop or reverse any form of congenital muscular dystrophy. The U.S. Food and Drug Administration (FDA) has approved injections of the drugs golodirsen and viltolarsen to treat Duchenne muscular dystrophy (DMD) patients who have a confirmed mutation of the dystrophin gene that is amenable to exon 53 skipping.
- Anti-Arrhythmics – The pharmacological treatment of patients with a prevalent involvement of the cardiac tissue conduction relies on the use of ACE-inhibitors and appropriate antiarrhythmic drugs. In the case of atrial arrhythmias, the preference is for drugs such as antiarrhythmics (flecainide, propafenone) and beta-blockers. [rx]
- Anti-Epileptics – Children need to be followed closely by neurologists. Management of epilepsy is necessary for some patients.[rx]
- Anti-Myotonics – The pain associated with muscle rigidity is greatly alarming in the patient.[rx] When myotonia is disabling, treatment with a sodium channel blocker such as phenytoin (100 mg orally three times daily), procainamide (0.5–1 g orally four times daily), or mexiletine (150 to 200 mg orally three times daily) may prove helpful, but the associated side effects, particularly for antiarrhythmic medications, are often limiting.[rx]
- Endocrine Management – In case of impaired growth and delayed puberty, advice from endocrinologists plays a crucial role in the development of the child.[rx] Progressive scoliosis and contracture require surgical intervention to prolong ambulation.[rx]
- Corticosteroid – deflazacort at a dose of 0.9mg/kg/day has been the mainstay of treatment.[rx][rx][rx] Corticosteroids should be started before physical disability and continue even after the loss of ambulation and in more severe cases.[rx] It is beneficial for improving pulmonary function, delays scoliosis (decreases the need for surgery), delaying the onset of cardiomyopathy, and prolongs survival.[rx][rx] Corticosteroid dose should be reduced by 25% to 33% in case of side effects.[rx]
- Nitric oxide – has become the drug of treatment in some cases to increase the blood supply to muscles through vasodilation.
- Non-Steroidal Anti-Inflammatory Drugs – Treatment involves the administration of non-steroidal anti-inflammatory drugs to decrease pain and inflammation.[rx]
- Glucocorticoids – administered as prednisone in a dose of 0.75 mg/kg per day, significantly slow progression of muscular dystrophy for up to 3 years.[rx] Some patients cannot tolerate glucocorticoid therapy; weight gain and increased risk of fractures, in particular, represent a significant deterrent.[rx] There is recent evidence that oral steroids early in the disease can lead to dramatically improved outcomes.[rx]
- Golodirsen (SRP-4053) – This drug is an antisense therapy used for the treatment of Duchenne muscular dystrophy. Patients need to have a confirmed mutation of the dystrophin gene to facilitate exon 53 skipping. It is FDA approved, but the evidence to support its use is not yet well established.[rx][rx]
Medication should not be used
Avoidance of specific agents, including
- Inhaled sedation (halothane),
- IV sedation (thiopentone),
- Muscle relaxants (succinylcholine, vecuronium),
- Neostigmine, and
- Some chemotherapy is essential.
- Propofol-induced pain can induce myotonia.[rx]
Surgical Treatment
- Contracture Release – Surgical release of contracture deformities is used to maintain normal function as long as possible.[rx] Massage and heat treatments also may be helpful.
- Defibrillator or Cardiac Pacemaker – Cardiac function requires monitoring, and pacemaker placement may be a consideration if there is evidence of heart block.[rx] Individuals with either Emery-Dreifuss or myotonic dystrophy may require a pacemaker at some point to treat cardiac problems. Management of cardiomyopathy and arrhythmias may be life-saving.[rx] In patients with severe syncope, established conduction system disorders with second-degree heart block previously documented, or tri-fascicular conduction abnormalities with significant PR interval lengthening, consideration needs to be given towards placement of a cardiac pacemaker.[rx] An advanced cardiac block is also an indication to install a pacemaker.[rx]
- Shoulder Surgery – Individuals with facioscapulohumeral muscular dystrophy may benefit from surgery to stabilize the shoulder.[rx]
- Spinal Correction – Scoliotic surgery is an option when curves exceed 20 degrees to prolong respiratory function or walking ability or both.[rx]
- Tendon or muscle-release surgery – is recommended when a contracture becomes severe enough to lock a joint or greatly impair movement. The procedure, which involves lengthening a tendon or muscle to free movement, is usually performed under general anesthesia. Rehabilitation includes the use of braces and physical therapy to strengthen muscles and maintain the restored range of motion. A period of immobility is often needed after these orthopedic procedures, thus the benefits of the procedure should be weighed against the risk of this period of immobility, as the latter may lead to a setback.
- Surgery to reduce the pain and postural imbalance – caused by scoliosis may help some individuals. Scoliosis occurs when the muscles that support the spine begin to weaken and can no longer keep the spine straight. The spinal curve, if too great, can interfere with breathing and posture, causing pain. One or more metal rods may need to be attached to the spine to increase strength and improve posture. Another option is spinal fusion, in which bone is inserted between the vertebrae in the spine and allowed to grow, fusing the vertebrae together to increase spinal stability.
- Tracheostomy – and assisted ventilation are needed for patients with respiratory failure, and treatment of cardiomyopathy with ACE inhibitors and beta-blockers can help prolong survival.[rx]
- Cataract surgery – involves removing the cloudy lens to improve the person’s ability to see.
Novel Therapies
-
Antisense Oligonucleotides (AONs) – work by degrading the CUG expansion, or by binding to CUG expansion to inhibit RNA sequestration and sites for abnormal MBNL binding.
-
Recombinant Adeno-associated viral (rAAV) – stimulates overexpression of MBNL1, to prevent sequestration. Inhibition of CUG-BP1 activity via small molecules (pentamidine) or by inhibiting protein kinase C (involved in activating CUG-BP1) can also prevent sequestration.
-
Clustered regularly interspaced short palindromic repeats (CRISPR/Cas) – cleave and degrade CUG mRNA expansion.
The following recommendations are acquired from Consensus-based care recommendations for congenital and childhood-onset myotonic dystrophy type 1 published in 2019,[rx], and 2- Consensus Statement on Standard of Care for Congenital Muscular Dystrophies, published in 2014.[rx]
- Neurology – disclosure of diagnosis should address five items: diagnosis, prognosis, recurrence risk, treatment plan, and family/community support. Patients should be followed by an experienced multidisciplinary team in the neuromuscular clinic. Routine surveillance every 3 to 4 months for infants less than 12 months, and 4 to 6 months in toddlers of more than 12 months. Allied health teams include nurses, physical and occupational therapists, speech and language therapists, social workers, and genetic counselors. Focusing on the financial burden and psychosocial aspects is vital. Referral to ophthalmology and other services, as discussed below, is recommended.
- Respiratory – the primary goal is to monitor respiratory function, decrease secretions, and manage assisted ventilation. There is often an improvement in respiratory strength over time, and consideration for tracheostomy should be careful. Maintenance pulmonary therapy includes cough assist, breathe staking, etc. Pulmonary function testing includes vital capacity (<40% predict nocturnal hypoventilation), spirometry (>20% difference between sitting and supine vital capacity indicates diaphragmatic weakness and is a predictor of nocturnal hypoventilation). Other tests include peak cough flow, polysomnography, and blood gases. Pneumococcal and influenza vaccines are recommended, and palivizumab against RSV for children under two years of age.
- Cardiology – arrhythmias, myopathies, and structural cardiac diseases can present with lethargy, dyspnea, pallor, palpitations, and syncope. A twice-yearly assessment is required with closer follow-ups in symptomatic patients.
- Gastroenterology – serial monitoring of nutrition and growth, feeding, GI motility (GERD, dysmotility, constipation), and oral care is recommended. Feeding tubes with or without Nissen fundoplication, laxatives, antacids, proton pump inhibitors, antiemetics, and probiotics are advisable to consider.
- Malocclusion – teeth crowding, caries, and gingival hyperplasia (prolonged NPO) should prompt an orthodontist evaluation.
- Orthopedics and Rehabilitation – conservative or surgical interventions are required to manage joint contractures, scoliosis, foot, and spine deformities. Bracing, serial splinting, and assisting devices to include walkers, orthotics, scooters, and wheelchairs, might be required to facilitate standing/walking/sitting. Yearly evaluation is recommended, more frequent in younger children to assess motor development and function. Physical activity is essential as children will experience progressive improvements in proximal muscle strength.
- Pain Management – Patients with CMD are prone to developing contractures and can lead to painful spasms and joint pain. Adequate management of pain is important to achieve a good quality of life.[rx][rx][rx]
- Psychiatry – Patients with CMD with their disability are prone to develop depression and anxiety and must have a psychiatry/psychologist referral as part of multidisciplinary care.[rx]
Prevention
-
Yearly influenza vaccine
-
Pneumococcal vaccine (PPS 23)[rx]
-
Assess for, in the presence of corticosteroid intake, weight gain, dysphagia, constipation, malnutrition or prior main surgeries
-
Physical therapy to prevent muscle contractures. Promote daily or regular exercise, but if there is muscle pain, reduce activity intensity or frequency
-
Monitor for serum calcium, phosphorus, alkaline phosphatase, 25-hydroxyvitamin D (per semester), magnesium, PTH, urine calcium, and creatinine; Dual-energy x-ray absorptiometry at age three and annually; spine x-rays; bone age, especially if under corticosteroid therapy[rx]
-
Consider biphosphonates if there is a history of symptomatic vertebral fractures, not as prophylaxis
-
Baseline pulmonary function tests and biannually along with pediatric pulmonologist if the patient uses a wheelchair, age 12, or has a reduction of vital capacity of less than 80%
-
Family members or caregivers should be educated regarding manual ventilation bags, mechanical insufflation-insufflation devices.
Complications
The CTG expansions of DM affect multiple organ systems in addition to the musculoskeletal system and is associated with several complications.
Central Nervous System
-
Intellectual disabilities can be seen in all types but are not universal for all types of DM. Most commonly seen in the congenital form of DM.
-
Cerebrovascular accidents can occur secondary to DM-associated atrial fibrillation.
-
Anxiety and depression due to the loss of functional status
-
Hypersomnia and sleep apnea are common due to sleep cycle dysfunctions.
-
Ventriculomegaly is seen in congenital DM.
Ophthalmologic
-
Cataracts are almost universal in all patients with DM and are seen early with typical onset in the ’40s. Hyperopia and astigmatism can also occur.
Cardiac
-
Atrial arrhythmias, conduction system slowing, ventricular arrhythmias, cardiomyopathy, and early-onset heart failure.
Pulmonary
-
Pneumonia is common due to progressive loss of lung function and reduced lung volumes as a result of progressive neuromuscular-associated respiratory failure.
-
Increased risk of anesthesia-related pulmonary complications[rx]
Gastrointestinal
-
Facial diplegia and oropharyngeal dysphagia can result in dysphagia and an increased risk of aspiration.
-
There is also an increased incidence of gallstones and cholecystitis due to a hypertonic gallbladder sphincter.
-
Transaminitis and liver enzyme elevations are seen for unknown reasons.
-
Increased risk of post-anesthesia aspiration due to the weakness of pharyngeal musculature.[rx]
Endocrine
-
Insulin insensitivity can be seen
-
The loss of the seminiferous tubules results and testicular atrophy results in male infertility.
-
In women, there is an increased risk of abortion, miscarriage, pre-term birth rates, and dysmenorrhea.
Dermatologic
-
Androgenic alopecia with frontal balding and increased risk of basal cell carcinoma and pilomatrixoma.[rx]
Musculoskeletal
-
There is a progressive loss of motor function with increased wheelchair dependency towards the end of life.
-
Impairments in activities of daily living (ADLs) due to distal muscle weakness of the hands and ankle dorsiflexion.
-
Myalgias are very commonly noted.
Nutrition/gastrointestinal
-
Bulbar dysfunction is universal in individuals with SMA I; the bulbar dysfunction eventually becomes a serious problem for persons with SMA II and only very late in the course of disease for those with SMA III.
-
Gastrointestinal issues may include constipation, delayed gastric emptying, and potentially life-threatening gastroesophageal reflux with aspiration.
-
Growth failure can be addressed with gastrostomy tube placement as needed.
-
Nonambulatory individuals with SMA II and III are at risk of developing obesity [rx].
Respiratory
Children with SMA I and II (and more rarely, type III) who are treated with supportive care only have a progressive decline in pulmonary function due to a combination of weak respiratory muscles, reduced chest wall, and lung compliance, and a reduction in alveolar multiplication[rx].
-
Respiratory failure is the most common cause of death in SMA I and II.
-
Decreased respiratory function leads to impaired cough with inadequate clearance of lower airway secretions, hypoventilation during sleep, and recurrent pneumonia.
-
Noninvasive ventilation, such as BiPAP, and airway clearance techniques are commonly used to improve respiratory insufficiency in those with SMA.
Orthopedic
Scoliosis, hip dislocation, and joint contractures are common complications in individuals with SMA. Scoliosis is a major problem in most persons with SMA II and in half of those with SMA III. With supportive care only:
-
Approximately 50% of affected children (especially those who are nonambulatory) develop spinal curvatures of more than 50 degrees (which require surgery) before age ten years;
-
Later in the disease course, nonambulatory individuals can develop thoracic kyphosis [rx];
-
Progressive scoliosis impairs lung function and if severe can cause decreased cardiac output [rx].
Metabolic
An unexplained potential complication of SMA is severe metabolic acidosis with dicarboxylic aciduria and low serum carnitine concentrations during periods of intercurrent illness or prolonged fasting [rx].
Consultations
Neurology and Physical Medicine and Rehabilitation
-
Oversee the patient’s non-primary medical care and help direct and coordinate care and needs
-
Should evaluate the patient annually for swallowing difficulties and functional mobility and durable medical equipment (DME) needs
-
Assess if therapy is required to improve functional mobility
-
Medications to help treat myotonia and pain
-
Electrodiagnostic testing if indicated
Cardiology
-
Indicated for those with cardiac symptoms, an abnormal annual 12-lead ECG, or those without a previous cardiac evaluation who are older than 40 years of age.[rx]
-
Due to the high incidence of cardiac involvement, cardiology referral should be considered as part of the routine multidisciplinary treatment.
Pulmonology
-
Symptoms of respiratory insufficiency, recurrent pulmonary infections, or less than 50% of predicted FVC
Ophthalmology
-
Annual eye exam that includes a slit-lamp examination
High-Risk Obstetrics and Gynecology
-
Indicated for those pregnant or considering pregnancy due to miscarriage, preterm delivery, and respiratory difficulties during pregnancy
Genetic Counseling
-
Indicated for those with a diagnosis of myotonic dystrophy and considering procreation
Physical, Occupational Therapy, and Speech-Language Pathology (SLP)
-
Indicated for impaired function, DME evaluation, and myalgias and chronic pain
-
SLP is indicated for concerns for dysphagia or dysarthria
![]()
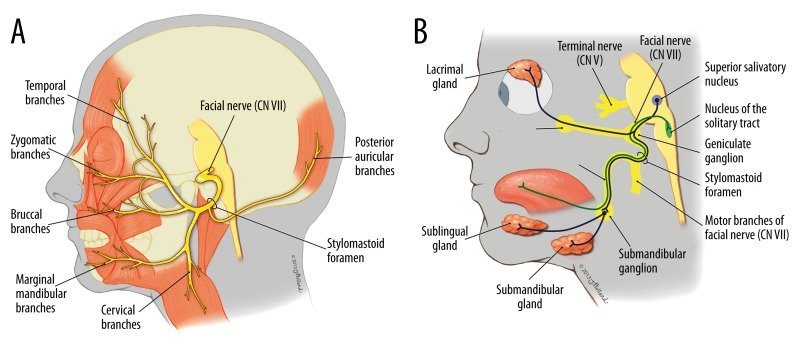

About the author