Electrolyte Abnormalities
Routine laboratory studies are common in the intensive care unit; abnormalities are even more common. Typically these studies include a chemistry panel (Chem 10). The differential diagnoses of the most frequent and clinically relevant electrolyte abnormalities are detailed below.
Differential Diagnosis and Evaluation of Hyponatremia
Differential Diagnosis and Evaluation of Hypernatremia
Differential Diagnosis and Evaluation of Hypokalemia
Differential Diagnosis of Hyperkalemia
Differential Diagnosis of Hypo and Hypercalcemia
Differential Diagnosis of Hypo and Hypermagnesemia
Differential Diagnosis of Hypo and Hyperphosphatemia
Hyponatremia
62M with a history of hepatitis C cirrhosis complicated by hepatocellular carcinoma s/p radiofrequency ablation presenting after referral from hepatology clinic for hyponatremia. One week ago, the patient developed abdominal distension and shortness of breath that resolved after large-volume paracentesis and was started on furosemide 40mg p.o. daily and aldactone 100mg p.o. daily.
After initiating diuretics, the patient noted worsening lower extremity edema, and increased thirst/fluid intake.
He reports two days of fatigue and intermittent confusion supported by family members who reported slowed speech. He otherwise denies abdominal pain, distension, nausea/vomiting, diarrhea/constipation, chest pain or shortness of breath. In the ED, the patient received 1L NS bolus.
PMH:
- Hepatitis C cirrhosis c/b HCC s/p RFA
- Rheumatoid arthritis, well-controlled without medications
PSH:
- None
FH:
- Non-contributory.
SHx:
- Lives with partner, denies current or prior t/e/d abuse
- HepC contracted from blood transfusions
Meds:
- Furosemide 40mg p.o. daily
- Spironolactone 100mg p.o. daily
- Rifaximin 550mg p.o. b.i.d.
Allergies
NKDA
Physical Exam
| VS: | T | 98.2 | HR | 80 | RR | 14 | BP | 95/70 | O2 | 98% RA |
| Vent: | PRVC, VT 320, RR 35, PEEP 6, FiO2 95% | |||||||||
| Gen: | Elderly female in no acute distress, alert and answering questions appropriately. | |||||||||
| HEENT: | NC/AT, PERRL, EOMI, no scleral icterus, MMM. | |||||||||
| CV: | RRR, normal S1/S2, no murmurs. JVP 8cm. | |||||||||
| Lungs: | Faint basilar crackles on bilateral lung bases. | |||||||||
| Abd: | Normoactive bowel sounds, non-distended, non-tender, without rebound/guarding. | |||||||||
| Ext: | 2+ pitting edema in lower extremities to knees bilaterally. 2+ peripheral pulses, warm and well perfused. | |||||||||
| Neuro: | AAOx3. CN II-XII intact. No asterixis. Normal gait. Normal FTN/RAM. | |||||||||
Labs/Studies
- BMP (admission): 112/5.6/88/22/28/1.1/97
- BMP (+10h): 118/5.4/93/23/26/1.0/133
- sOsm: 264
- Urine: Na <20, K 26, Osm 453
- BNP: 40
- AST/ALT/AP/TB/Alb: 74/57/91/2.4/2.2
Assessment/Plan
62M hx HepC cirrhosis, newly decompensated with e/o decompensation (new-onset ascites) and hyponatremia.
# hyponatremia: Sodium 114, likely chronic, patient currently asymptomatic without concerning findings on neurological exam. Clinical findings suggestive of hypervolemic hyponatremia 2/2 decompensated cirrhosis resulting in decreased effective arterial blood volume and volume retention. However, the recent initiation of diuretics, mild AKI and early response to isotonic fluids in the ED suggests possible hypovolemic component.
- 1L fluid restriction
- q.4.h. sodium check, goal increase of 8mEq per 24h
- hold diuretics
# hyperkalemia: Potassium 5.6, asymptomatic, AKI vs. medication-induced (aldactone). Continue monitoring.
# AKI: Elevated creatinine 1.1 from baseline 0.7. Likely pre-renal given recent initiation of diuretics. Consider hepatorenal syndrome given decompensated cirrhosis. Follow-up repeat creatinine after 1L NS bolus in ED.
# hepatitis C: decompensated with new-onset ascites. No e/o encephalopathy, continue home rifaximin.
Physiology of Hyponatremia
Differential Diagnosis of Hyponatremia
Evaluation of Hyponatremia
- Identification of onset (acute vs. chronic)
- Presence of symptoms (HA, nausea, confusion, seizures)
- Assessment of volume status (edema, JVD, skin turgor, postural BP)
- Medical history (cardiac, liver, renal disease), drug history
Hyperglycemic Crises
Blurred vision, numbness
HPI:
56 year-old male with a history of DM, questionable HTN presenting with blurred vision, numbness of fingertips/toes for 2wks. Associated symptoms include dry mouth, polydipsia/polyuria. He states that these symptoms coincide with elevated measurements of blood glucose at home (>500). He ran out of his diabetes medication (metformin) 8mo ago but states his BG was typically between 100-200 with diet/exercise until 2wks ago. He reports recent dietary indiscretions on a trip to Las Vegas.
He denies fevers/chills, CP/SOB, cough, abdominal pain, N/V, or dysuria.
PMH:
- DM II
- HTN
PSH:
None
FH:
Several maternal family members with DM.
SHx:
- No tobacco/drug use
- 5-6 alcoholic drinks/wk
Meds:
- Metformin 500mg p.o. b.i.d.
Allergies:
NKDA
Physical Exam
| VS: | T 37.8 HR 60 RR 14 BP 165/90 O2 99% RA |
| Gen: | Well-appearing, no acute distress, obese |
| HEENT: | PERRL, EOMI, optic discs sharp b/l, no abnormalities visualized |
| CV: | RRR, normal S1/S2, no M/R/G, no additional heart sounds |
| Lungs: | CTAB, no wheezes/crackles |
| Abd: | +BS, soft, NT/ND, no rebound/guarding |
| Ext: | Warm, well-perfused, 2+ pulses, no clubbing/cyanosis/edema |
| Neuro: | AAOx3, CN II-XII intact |
Labs/Studies
- BMP: 135/3.8/102/24/18/1.1/378
- CBC: 7.4/14.1/42.0/403
- UA: + glucose, – ketones
Assessment/Plan
56M, hx DM with poor medication adherence presenting with vision changes and stocking/glove paresthesias for 2wks after reported dietary indiscretion found to be hyperglycemic. DKA/HHS unlikely given stable vital signs, normal metabolic panel with exception of isolated hyperglycemia (slight hyponatremia likely related to osmotic effect of elevated serum glucose). Also, no evidence of concerning precipitates for hyperglycemic crisis (no CP/SOB, no F/C, no cough, no abdominal pain, no change in mental status). Patient was discharged home with education on importance of medication adherence, refill of metformin, and follow-up with primary care physician for further management of DM and possible hypertension.
Evaluation of hyperglycemic crises in patients with diabetes
Key signs/symptoms of HHS/DKA
- Both: Polyuria, polydipsia, weight loss, hypovolemia (dry MM, skin turgor, tachycardia, hypotension)
- DKA: Short course (<24h), N/V, diffuse abdominal pain, Kussmaul respirations
- HHS: Longer course (days/weeks), altered mental status (lethargy, coma, seizure)
Admission Laboratory Data of Patients with HHS vs. DKA
| DKA | HHS | |
|---|---|---|
| Glucose (mg/dl) | 616 | 930 |
| pH | 7.12 | 7.30 |
| 3-β-hydroxybutyrate (mmol/l) | 9.1 | 1.0 |
| Serum osmolality | 323 | 380 |
| Delta gap (AG-12) | 17 | 11 |
| Na (mEq/l) | 134 | 149 |
| K (mEq/l) | 4.5 | 3.9 |
| Bicarbonate (mEq/l) | 9 | 18 |
Delirium, ID
A 70 year-old female with a PMH of HTN, DM, hyperlipidemia and stage I breast cancer s/p lumpectomy with sentinel LN biopsy several years ago presented for elective surgery complicated by post-operative bleeding. She is now 4 days post-op and was found to be confused, somnolent and occasionally agitated.
HPI:
The patient could not be interviewed.
PE:
- VS: Stable and within normal limits
- General: unremarkable except for crackles in bilateral lung bases
- MSE: only arouses to sternal rub and becomes agitated, moving all four extremities spontaneously and symmetrically.
- Reflexes: corneal and gag reflexes present, suppresses eye movements with head turn, deep tendon reflexes 3+ throughout UE/LE bilaterally.
Assessment
70 year-old woman with a history of HTN, DM, hyperlipidemia and breast cancer presents with worsening confusion, somnolence and occasional agitation four days after surgery. The combination of significantly altered consciousness and absence of focal neurological findings, all in the setting of a complicated surgical course suggest delirium.
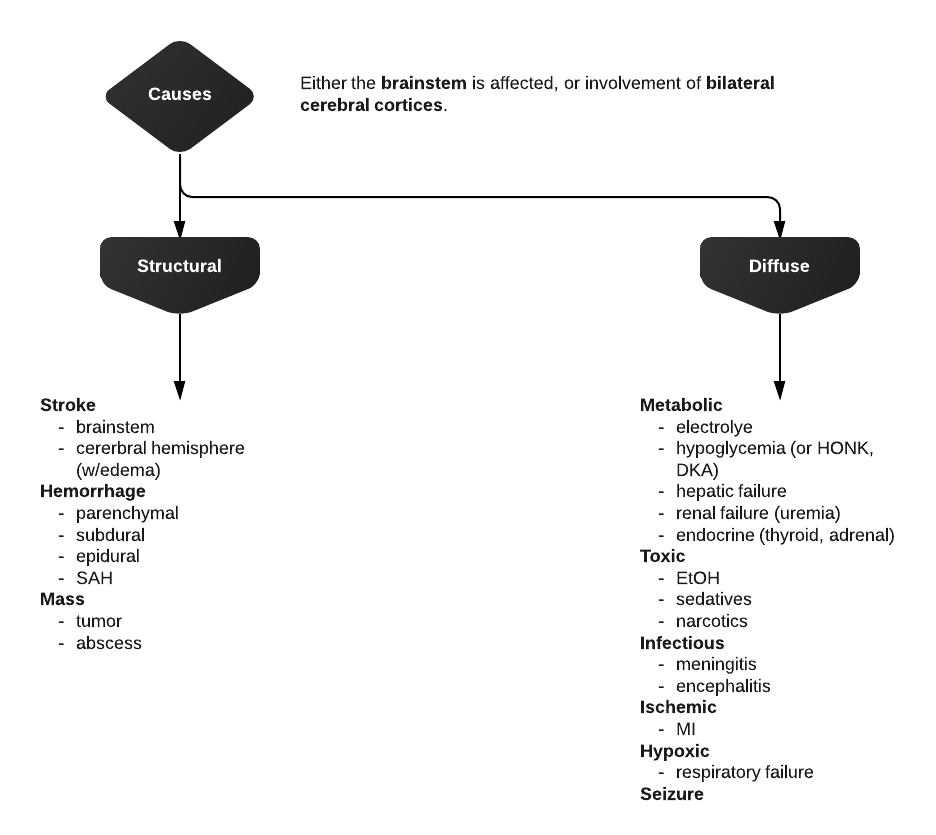
Differential Diagnosis of Altered Mental Status
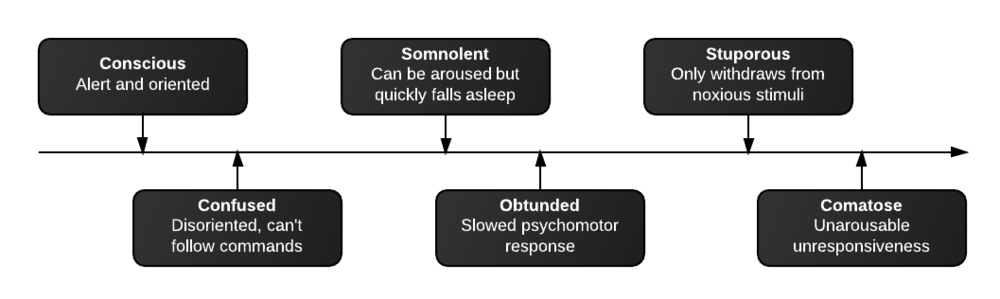
Levels of consciousness
There are different levels of consciousness, they are named in the diagram below but are better described by the characteristics observed.
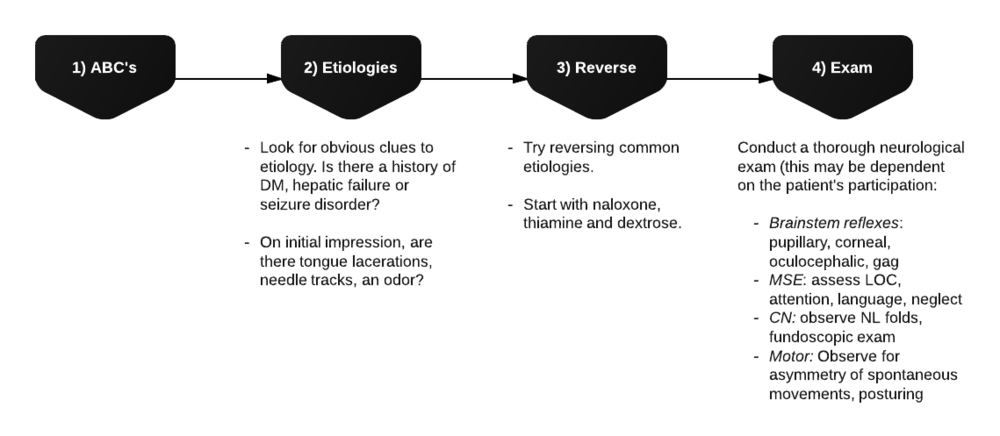
Initial assessment
Differential Diagnosis for Altered Mental Status
References













Visitor Rating: 5 Stars
Visitor Rating: 5 Stars