Electrocardiography (ECG or EKG) is the process of recording the electrical activity of the heart over a period of time using electrodes placed on the skin. These electrodes detect the tiny electrical changes on the skin that arise from the heart muscle’s electrophysiologic pattern of depolarizing and repolarizing during each heartbeat. It is a very commonly performed cardiology test.
In a conventional 12-lead ECG, ten electrodes are placed on the patient’s limbs and on the surface of the chest. The overall magnitude of the heart’s electrical potential is then measured from twelve different angles (“leads”) and is recorded over a period of time (usually ten seconds). In this way, the overall magnitude and direction of the heart’s electrical depolarization is captured at each moment throughout the cardiac cycle. The graph of voltage versus time produced by this noninvasive medical procedure is an electrocardiogram.
Medical Uses
The overall goal of performing electrocardiography is to obtain information about the structure and function of the heart. Medical uses for this information are varied and generally relate to having a need for knowledge of the structure and/or function. Some indications for performing electrocardiography include:
- Suspected myocardial infarction (heart attack) or new chest pain
- Suspected pulmonary embolism or new shortness of breath
- A third heart sound, fourth heart sound, a cardiac murmur or other findings to suggest structural heart disease
- Perceived cardiac dysrhythmias either by pulse or palpitations
- Monitoring of known cardiac dysrhythmias
- Chest pain
- Atypical chest pain
- Epigastric pain
- Back, neck, jaw or arm pain without chest pain
- Palpitations
- Syncope or near syncope
- Pulmonary edema
- Exertional dyspnea
- Weakness
- Diaphoresis unexplained by ambient temperature
- Feel of anxiety or impending doom
- Suspected diabetic ketoacidosis
- Fainting or collapse
- Seizures
- Monitoring the effects of a heart medication (e.g. drug-induced QT prolongation)
- Assessing severity of electrolyte abnormalities, such as hyperkalemia
- Hypertrophic cardiomyopathy screening in adolescents as part of a sports physical out of concern for sudden cardiac death (varies by country)
- Perioperative monitoring in which any form of anesthesia is involved (e.g. monitored anesthesia care, general anesthesia); typically both intraoperative and postoperative
- As a part of a pre-operative assessment some time before a surgical procedure (especially for those with known cardiovascular disease or who are undergoing invasive or cardiac, vascular or pulmonary procedures, or who will receive general anesthesia)
- Cardiac stress testing
- Computed tomography angiography (CTA) and Magnetic resonance angiography (MRA) of the heart (ECG is used to “gate” the scanning so that the anatomical position of the heart is steady)
- Biotelemetry of patients for any of the above reasons and such monitoring can include internal and external defibrillators and pacemakers
Diagnosis
Numerous diagnoses and findings can be made based upon electrocardiography, and many are discussed above. Overall, the diagnoses are made based on the patterns. For example, an “irregularly irregular” QRS complex without P waves is the hallmark of atrial fibrillation; however, other findings can be present as well, such as a bundle branch block that alters the shape of the QRS complexes. ECGs can be interpreted in isolation but should be applied – like all diagnostic tests – in the context of the patient. For example, an observation of peaked T waves is not sufficient to diagnose hyperkalemia; such a diagnosis should be verified by measuring the blood potassium level. Conversely, a discovery of hyperkalemia should be followed by an ECG for manifestations such as peaked T waves, widened QRS complexes, and loss of P waves. The following is an organized list of possible ECG-based diagnoses.
Rhythm disturbances/arrhythmias:
- Atrial fibrillation & atrial flutter without rapid ventricular response
- Premature atrial contraction (PACs) & Premature ventricular contraction (PVCs)
- Sinus arrhythmia
- Sinus bradycardia & sinus tachycardia
- Sinus pause & sinoatrial arrest
- Sick sinus syndrome: bradycardia-tachycardia syndrome
- Supraventricular tachycardia
- Atrial fibrillation (afib) with rapid ventricular response
- Atrial flutter with rapid ventricular response
- AV nodal reentrant tachycardia
- Atrioventricular reentrant tachycardia
- Junctional ectopic tachycardia
- Atrial tachycardia
- Ectopic atrial tachycardia (unicentric)
- Multifocal atrial tachycardia
- Paroxysmal atrial tachycardia
- Sinoatrial nodal reentrant tachycardia
- Torsades de pointes (polymorphic ventricular tachycardia)
- Wide complex tachycardia
- Ventricular flutter
- Ventricular fibrillation
- Ventricular tachycardia (monomorphic ventricular tachycardia)
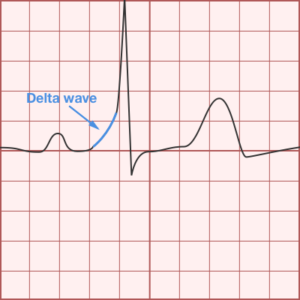
- Pre-excitation syndrome
- Lown–Ganong–Levine syndrome
- Wolff–Parkinson–White syndrome
- J wave/Osborn wave
Heart block and conduction problems:
- Aberration
- Sinoatrial block: first, second, and third-degree
- AV node
- First-degree AV block
- Second-degree AV block (Mobitz I & II; Mobitz I aka Wenckebach)
- Third-degree AV block/complete AV block
- Right bundle
- Incomplete right bundle branch block
- Complete right bundle branch block (RBBB)
- Left bundle
- Complete left bundle branch block (LBBB)
- Incomplete left bundle branch block
- Left anterior fascicular block (LAFB)
- Left posterior fascicular block (LPFB)
- Bifascicular block (LAFB plus LPFB)
- Trifascicular block (LAFP plus FPFB plus RBBB)
- QT syndromes
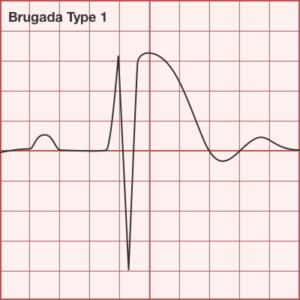
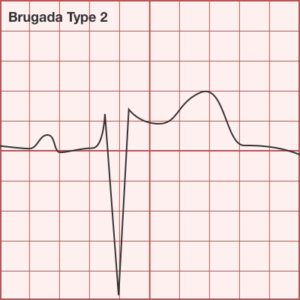
- Brugada syndrome
- Short QT syndrome
- Long QT syndromes, genetic and drug-induced
- Right and left atrial abnormality
Electrolytes disturbances & intoxication:
- Digitalis intoxication
- Calcium: hypocalcemia and hypercalcemia
- Potassium: hypokalemia and hyperkalemia
Ischemia and infarction:
- Wellens’ syndrome (LAD occlusion)
- de Winter T waves (LAD occlusion)
- ST elevation and ST depression
- High Frequency QRS changes
- Myocardial infarction (heart attack)
- Non-Q wave myocardial infarction
- NSTEMI
- STEMI
- Sgarbossa’s criteria for ischemia with a LBBB
Structural
- Acute pericarditis
- Right and left ventricular hypertrophy
- Right ventricular strain/S1Q3T3 (can be seen in pulmonary embolism)
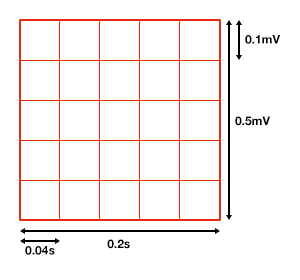
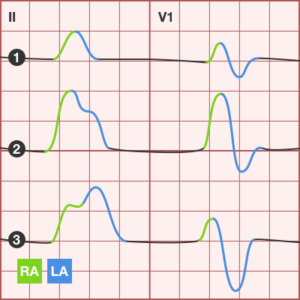
Grid and Leads
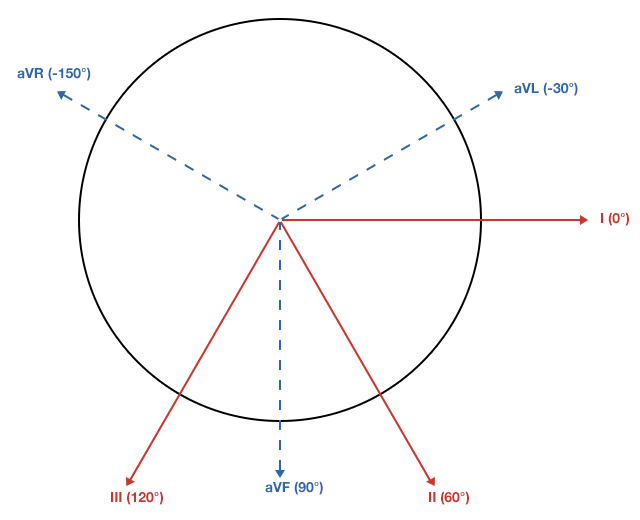
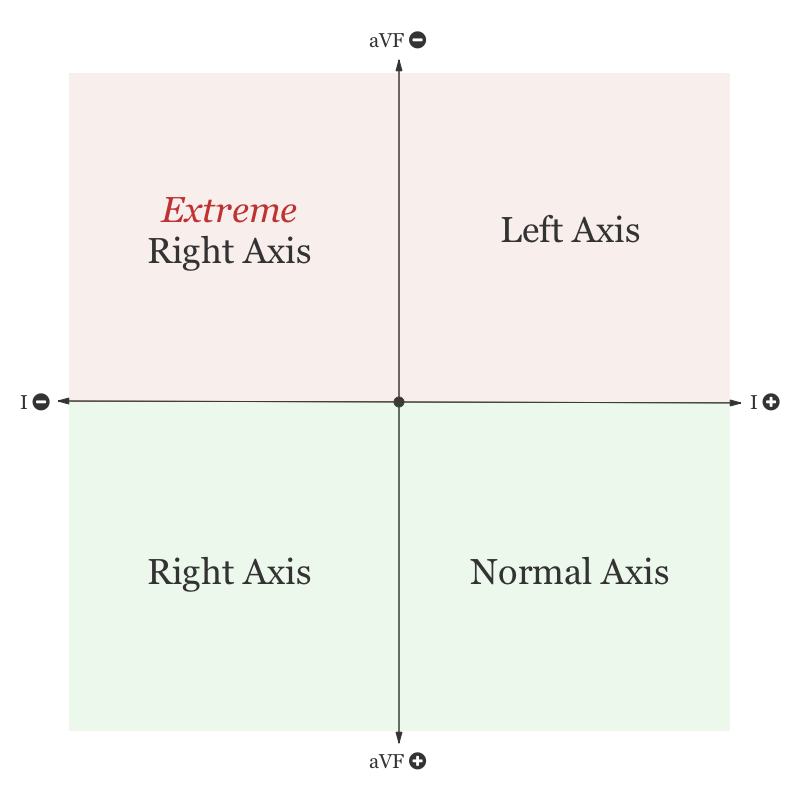
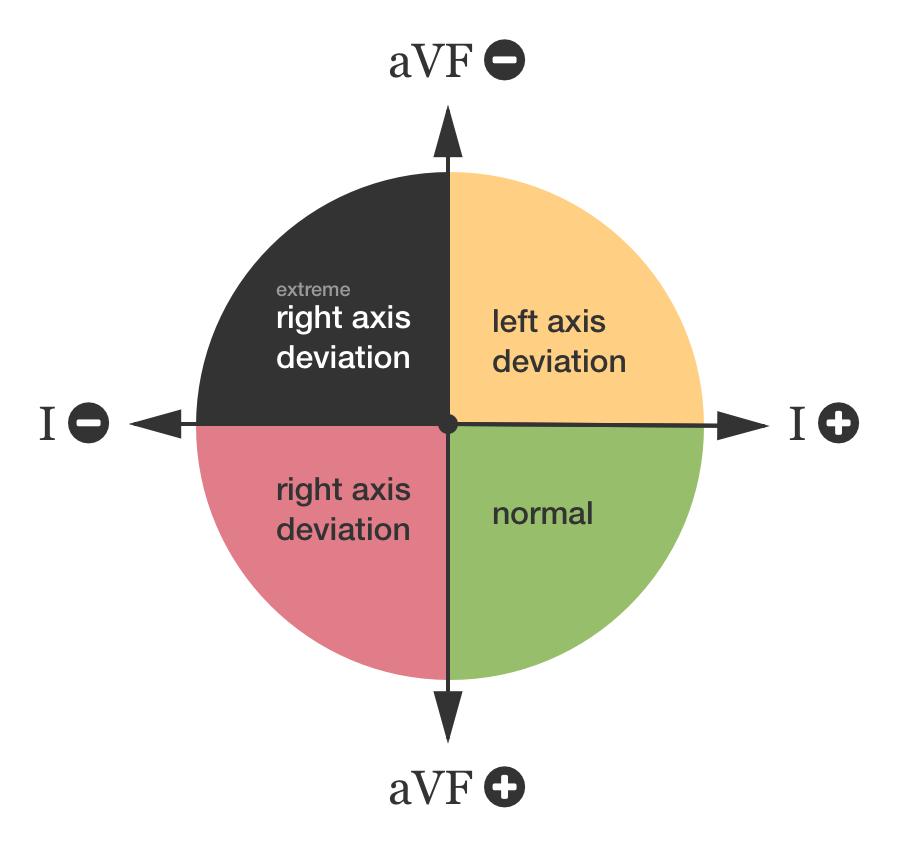
Axis
Atrial Enlargement
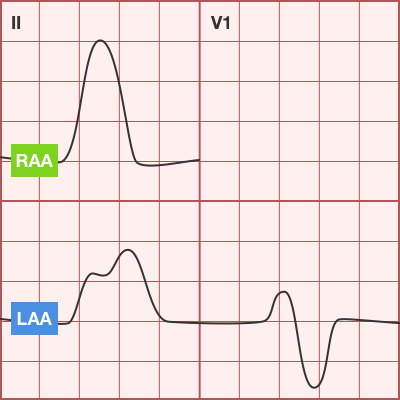
- Normal:
- First portion of deflection is RA, second is LA
- Right Atrial Enlargement:
- P-wave amplitude > 2.5mm in inferior leads
- Normal duration P-wave
- Left Atrial Enlargement:
- P-wave duration increased (terminal negative portion >0.04s)
- Amplitude of terminal negative component >1mm below isoelectric line in V1
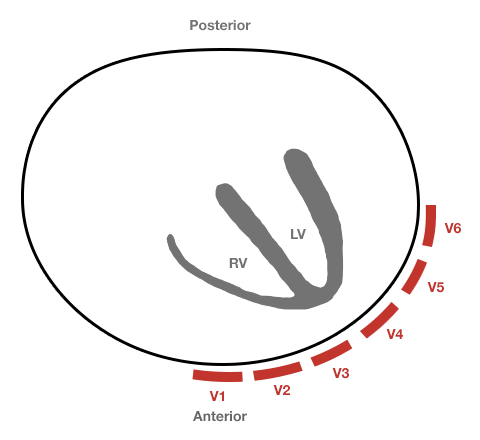
Ventricular Hypertrophy
- Right Ventricular Hypertrophy:
- Right axis deviation
- Abnormal R-wave progression
- Increased R-wave amplitude in leads overlying the right ventricle (V1)
- Increased S-wave amplitude in leads overlying the left ventricle (V6)
- Criteria
- V1: R>S
- V6: S>R
- Left Ventricular Hypertrophy:
- Left axis deviation
- Increased R-wave amplitude in leads overlying the LV (I, aVL, V5, V6)
- Increased S-wave amplitude in leads overlying the RV (V1)
- Criteria:
- Precordial Leads
- R-wave in V5/V6 + S-wave in V1/V2 > 35mm
- R-wave in V5 > 26mm
- R-wave in V6 > 20mm
- Limb Leads
- R-wave in aVL > 11mm
- R-wave in aVF > 20mm
- Combined
- R-wave in aVL + S-wave in V3 > 20mm (F), 28mm (M)
- Precordial Leads
Secondary Repolarization Abnormalities
- Downsloping ST-segment depression
- Asymmetric T-wave inversion
Bundle Branch Blocks
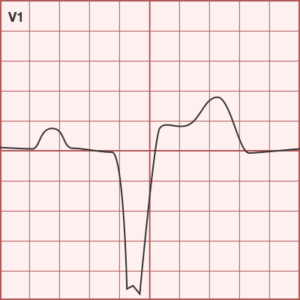
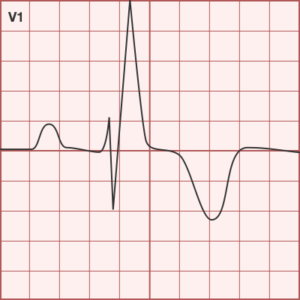
Left Bundle Branch Block
- QRS duration > 0.12s (3 boxes)
- Broad or notched R-wave with prolonged upstroke in I, aVL, V5, V6
- Associated ST-segment depression and T-wave inversion
- Reciprocal changes in V1, V2 (deep S-wave)
- Possible LAD
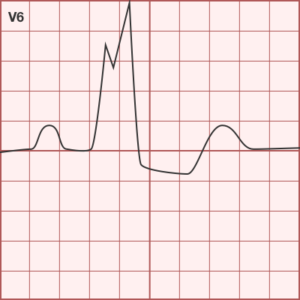
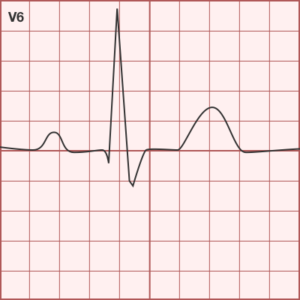
Right Bundle Branch Block
- QRS duration > 0.12s (3 boxes)
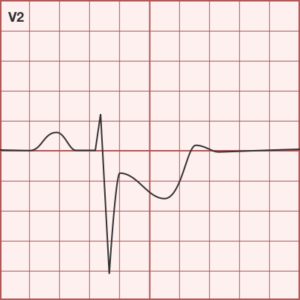
- RSR’ in V1, V2
- Reciprocal changes in I, aVL, V5, V6 (deep S-wave)
Hemiblocks
Other Blocks
- Non-specific intraventricular conduction delay: QRS >0.10s without BBB
- Incomplete BBB: LBBB/RBBB pattern with non-prolonged QRS
- Bifascicular block: RBBB + LAFB/LPFB (by axis deviation)
Ischemia and Infarction
- Hyperacute T-waves
- T-wave inversion: Symmetric, compared to TWI associated with repolarization abnormalities
- ST-elevation: Unlike J-point elevation, ST-segment merges with T-wave
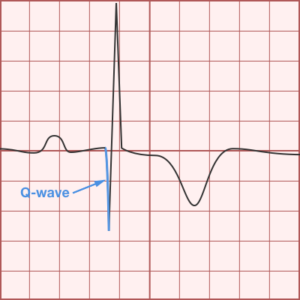
- Q-waves
- Duration > 0.04s
- Amplitude > 1/3 R-wave
- Normal in aVR
Coronary Artery Territories
| DISTRIBUTION | CORONARY ARTERY | LEADS | RECIPROCAL CHANGES |
|---|---|---|---|
| 1. Inferior | RCA, PDA | II, III, aVF | Anterior, Lateral |
| 2. Lateral | LCx | I, aVL, V5, V6 | Inferior |
| 3. Anterior | LAD | V1-V6 | Inferior |
| 4. Posterior | RCA | Posterior | Anterior (esp. V1) |
ECG Guide: Pediatrics
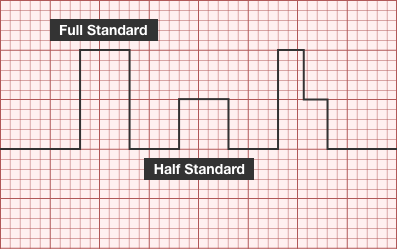
ECG Standard
- Full standard: no adjustment
- Half-standard: commensurate reduction in amplitude (usually 50%)
- Mixed: reduction in amplitude of precordial leads
Axis
- Anatomical dominance of right ventricle until approximately 6mo
- RAD normal
- eRAD suggests AV canal defect
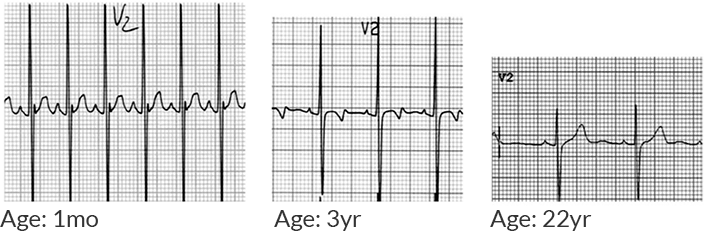
T-waves
- 1st week of life: Upright
- Adolescent: Inverted
- Adult: Upright
Ventricular Hypertrophy
- Right Ventricular Hypertrophy
- R-wave height >98% for age in lead V1
- S-wave depth >98% for age in lead V6
- T-wave abnormality (ex. upright in childhood)
- Causes: pHTN, PS, ToF
- Left Ventricular Hypertrophy
- R-wave height >98% for age in lead V6
- S-wave depth >98% for age in lead V1
- Adult-pattern R-wave progression in newborn (no large R-waves and small S-waves in right precordial leads)
- Left-axis deviation
- Causes: AS, coarctation, VSD, PDA
Examples
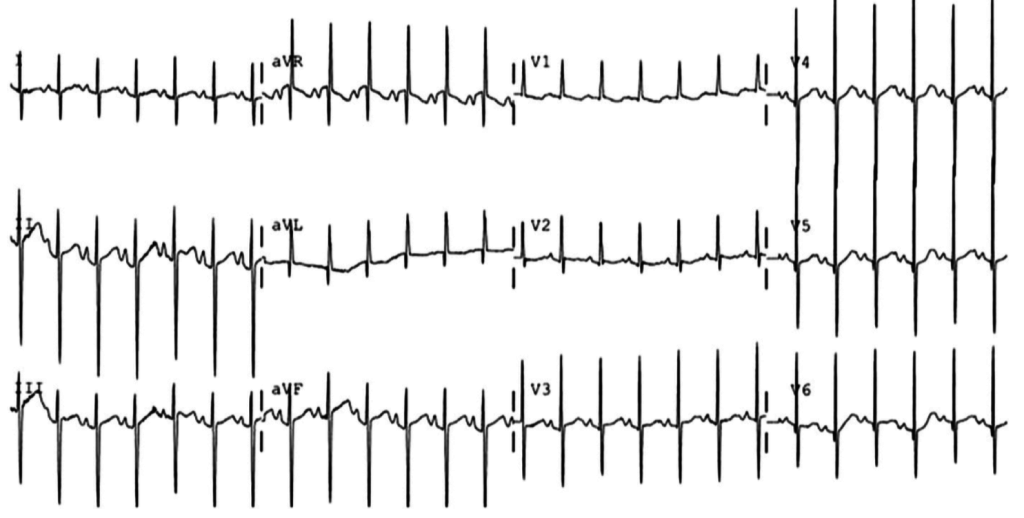
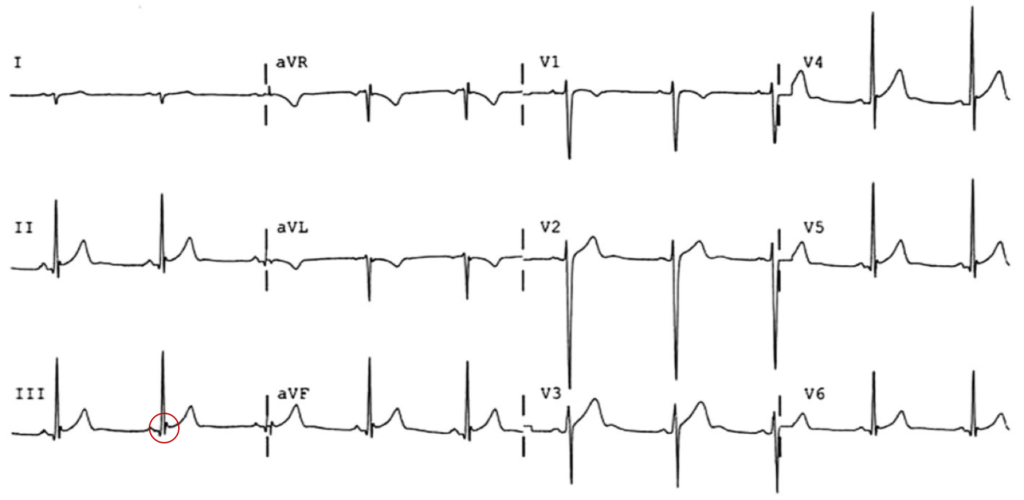
- 2mo old
- RAD
- Inverted T-waves (normal)
- Tall R-waves in V1-V3
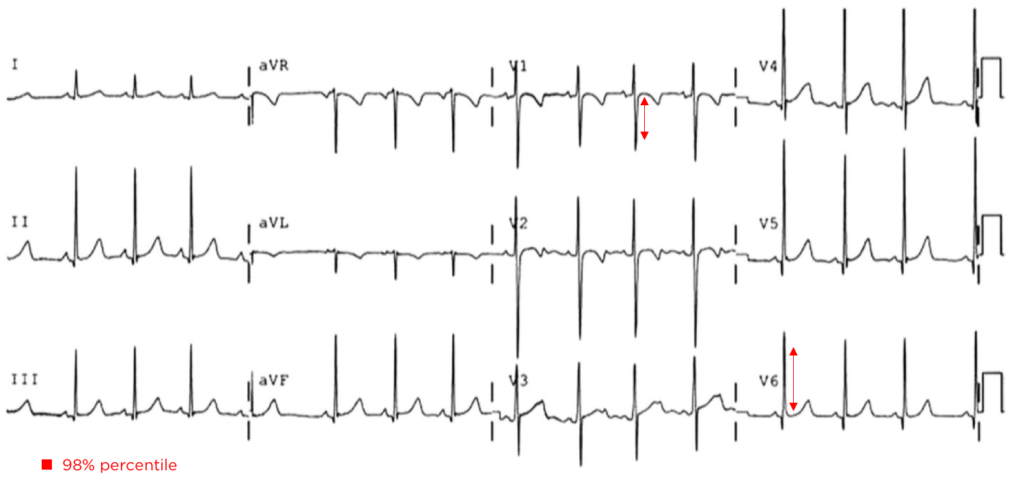
- Neonate with Down syndrome
- Isoelectric in I, Negative in aVF negative in II mean QRS vector -87°
- Extreme RAD suggestive of AV canal defect
- Unrepaired Coarctation
- Deep S-wave in V1 (>98%)
- Tall R-wave in V6 (>98%)
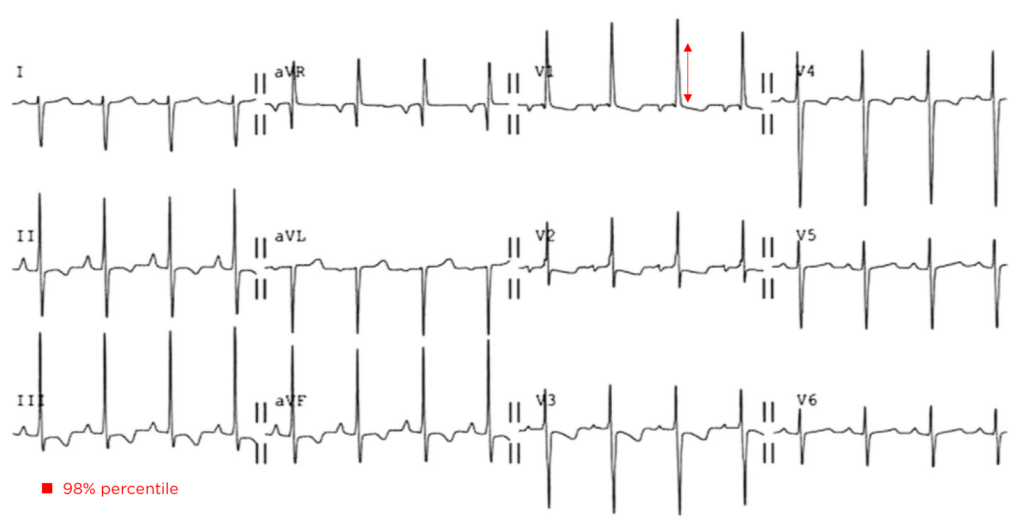
- 10 year-old boy with pulmonary Hypertension
- RAD after expected age for normal RAD
- Tall R-waves in V1 (>98%)
- Deep S-wave in V6 (>98%)
- ALCAPA (anomalous origin of the left coronary artery from the pulmonary artery): coronary artery arises anomalously from the pulmonary artery; as pulmonary arterial pressure falls during the first 6 months of infancy, prograde flow through the left coronary artery ceases and may even reverse.
- HLHS (hypoplastic left heart syndrome): coronary arteries are perfused from a hypoplastic, narrow aorta that is susceptible to flow disruption
- Orthotopic heart transplant with allograft vasculopathy
- Kawasaki: coronary artery aneurysm with subsequent thrombosis
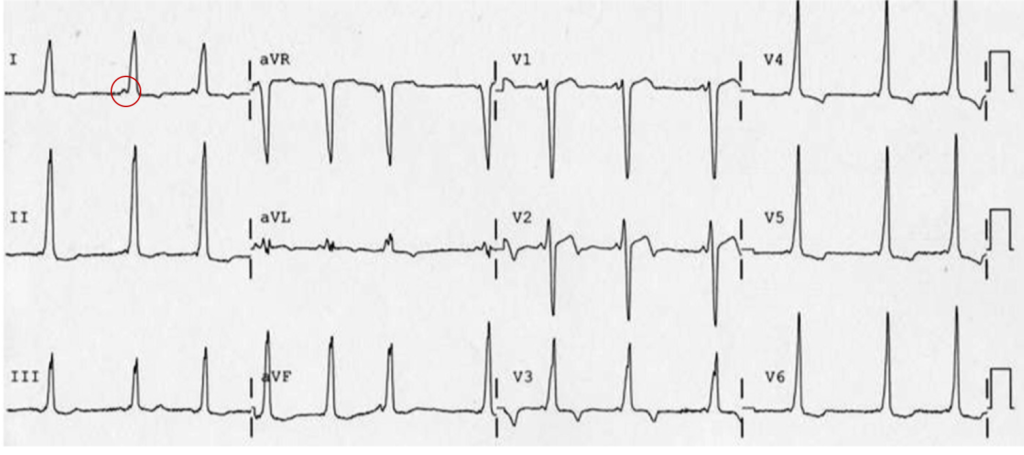
- 14 year-old male
- Concave ST-segment elevation
- 9mo female with mitral insufficiency
- Broad biphasic P-wave in V1
- Tall, notched P-wave in II
- 18-year-old female
- Familial long QT syndrome and a history of cardiac arrest
- Delta wave, shortened PR interval
ECG Guide: Part II
STEMI
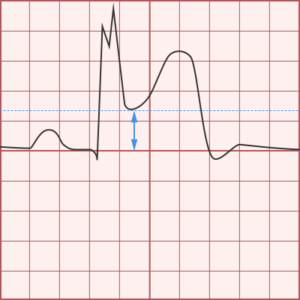
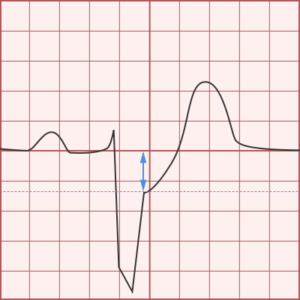
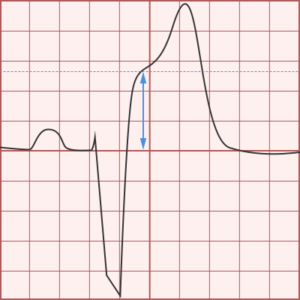
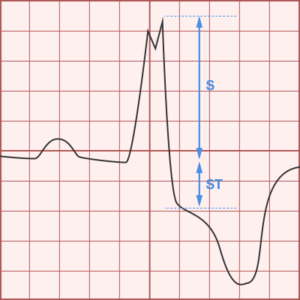
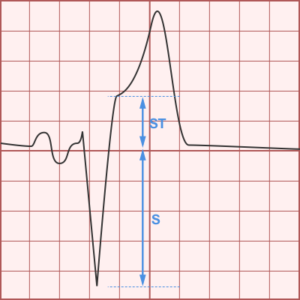
Sgarbossa Criteria
- Evaluation for STEMI in LBBB or paced rhythm
- Normal: ST-segment discordant with QRS
- QRS associated with ST-segment depression
- QRS associated with (commensurate) ST-segment elevation
- Score ≥ 3 98% specific for MI
Modified Sgarbossa Criteria
- ST:S ratio ≥ 0.25 in any lead
- Presence of any criterion is positive
Other Causes of ST-segment Elevation
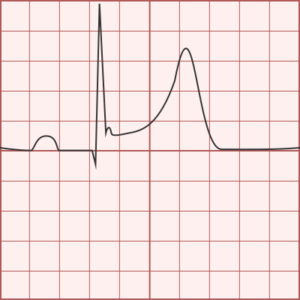
Benign Early Repolarization
- Concave ST-segment elevation
- Notch at J-point
- Asymmetric T-waves (steeper descent)
Pericarditis
- Diffuse ST-segment elevation (except aVR)
- PR-segment depression
- Ratio: ST-elevation to T-wave amplitude ≥ 0.25 in V6 suggests pericarditis
Ischemia and Prior Infarcts
Syncope
Other
Atrial Abnormalities
- Normal
- RAA: P-wave amplitude > 2.5mm in inferior leads
- LAA: P-wave duration increased (terminal negative portion >0.04s), amplitude of terminal negative component >1mm below isoelectric line in V1
Left Bundle Branch Block
- QRS duration > 0.12s (3 boxes)
- Broad or notched R-wave with prolonged upstroke in I, aVL, V5, V6
- Associated ST-segment depression and T-wave inversion
- Reciprocal changes in V1, V2 (deep S-wave)
- Possible LAD
Axes
Bradycardia
Brief H&P
A 38 year-old male with no medical history presents to the emergency department with abdominal pain. He had one episode each of non-bloody emesis followed by watery, non-bloody diarrhea and cited several sick contacts at home with similar symptoms. Vital signs were notable for bradycardia with a heart rate ranging from 38-46bpm though he was normotensive. The examination including abdominal examination was benign. A 12-lead electrocardiogram was obtained which demonstrated sinus bradycardia. The patient was asymptomatic during episodes of bradycardia and his heart rate responded appropriately during activity and on further history reported that he was an endurance athlete and runs multiple marathons each year. He was discharged after symptomatic improvement with anti-emetics.
Bradycardia
- Definition: heart rate <60bpm
- Sinus rhythm: upright P-wave in I, II, aV; inverted P-wave in aVR
Electrocardiographic Findings
- Sinus bradycardia
- Potentially asymptomatic and present in healthy individuals
- Sinoatrial node dysfunction (sick sinus syndrome, SSS)
- Sinus bradycardia
- Sinus arrest
- Tachy-brady syndrome (sinus bradycardia/arrest interspersed with SVT)
- Atrioventricular block
- 1st degree: PR prolongation, rarely symptomatic
- 2nd degree: Intermittent interruption of conduction of atrial impulses to ventricles
- Type 1: progressive PR prolongation leading to interrupted conduction
- Type 2: fixed PR interval with interrupted conduction
- 3rd degree: atrioventricular dissociation
- Slow atrial fibrillation
- Irregular RR interval without recognizable P-wave
Epidemiology
- Analysis of 277 patients presenting to the emergency department with “compromising” bradycardia.
- Symptoms
- Syncope (33%)
- Dizziness (22%)
- Angina (17%)
- Dyspnea/Heart Failure (11%)
- ECG
- High-grade AV block (48%)
- Sinus bradycardia (17%)
- Sinus arrest (15%)
- Slow atrial fibrillation (14%)
- Cause
- Primary (49%)
- Drug (21%)
- Ischemia/Infarction (14%)
- Pacemaker failure (6%)
- Intoxication (6%)
- Electrolyte disorder (4%)
Important Historical Features
- Fever/travel
- Chest pain
- Cold intolerance, weight gain
- Headache, AMS, trauma
- Abdominal pain/distension
- Medication changes
Important Examination Findings
- Perfusion (temperature, capillary refill)
- Presence of fistula or hemodialysis catheter
- Existing device (malfunction)
Workup
- ECG
- Continuous telemetry monitoring
- Labs
- Potassium
- Digoxin level
- TFT
- Infection titers (RPR, Lyme)
- Cardiac enzymes
Management
- Unstable
- Airway
- Atropine 0.5mg IV q3-5min (maximum 3mg)
- Dopamine/epinephrine infusion
- Temporary pacemaker (transcutaneous, transvenous) with blood-pressure preserving sedation
- Admission and evaluation for permanent pacemaker placement
- Stable (outpatient evaluation)
- Event monitor
- Stress test (chronotropic incompetence)
Algorithm for the Evaluation and Management of Bradycardia
Case Presentation
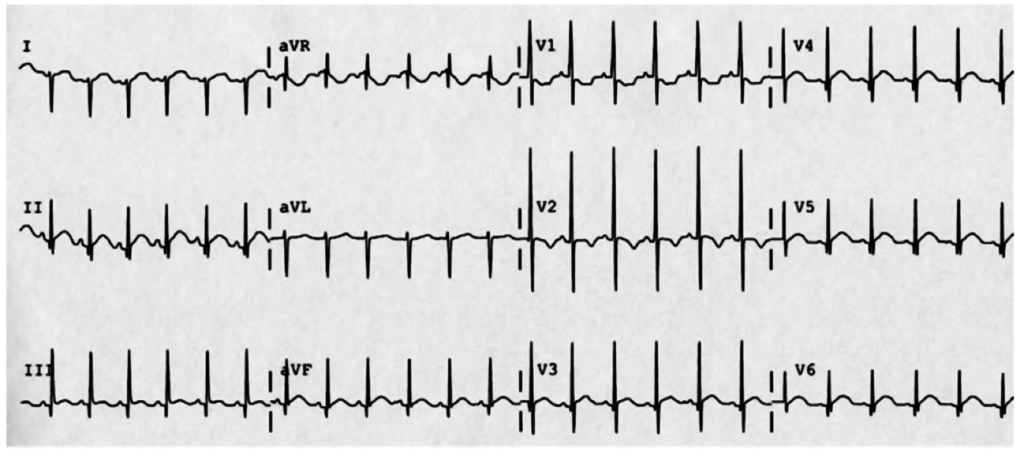
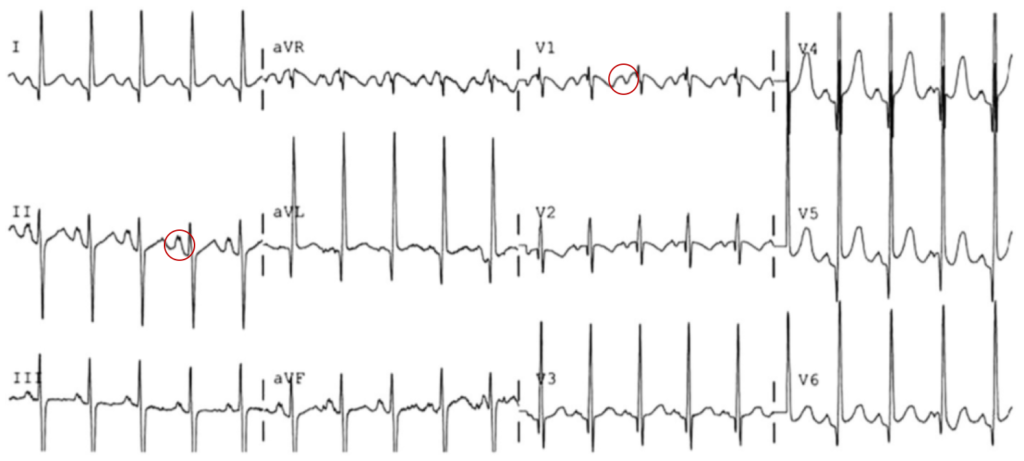
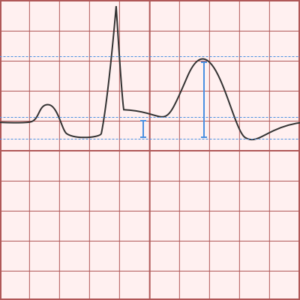
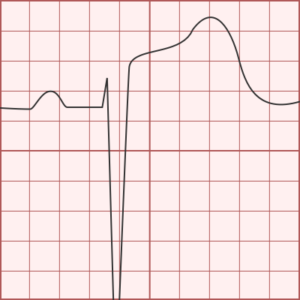
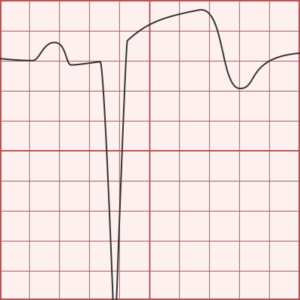
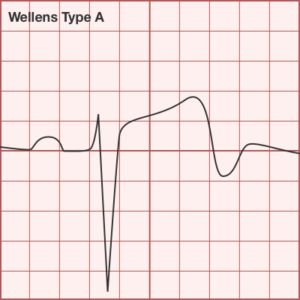
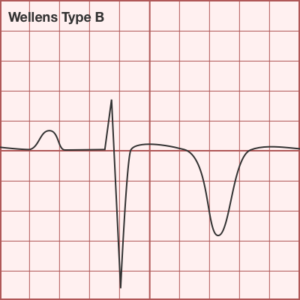
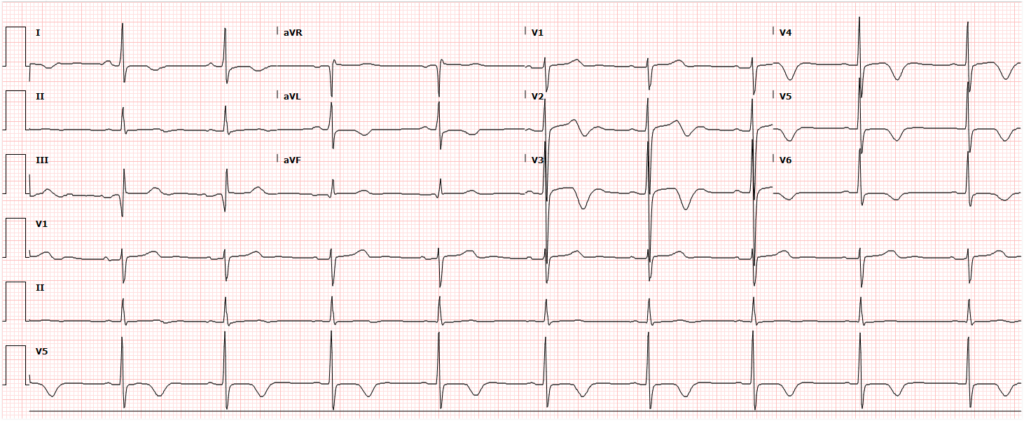
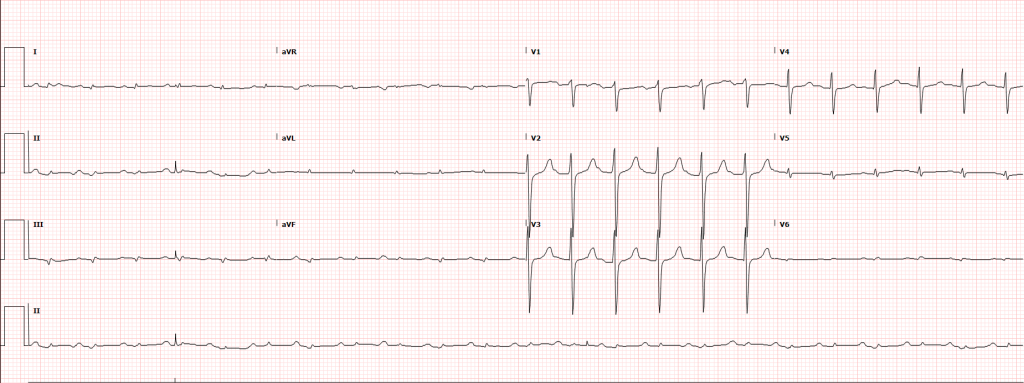
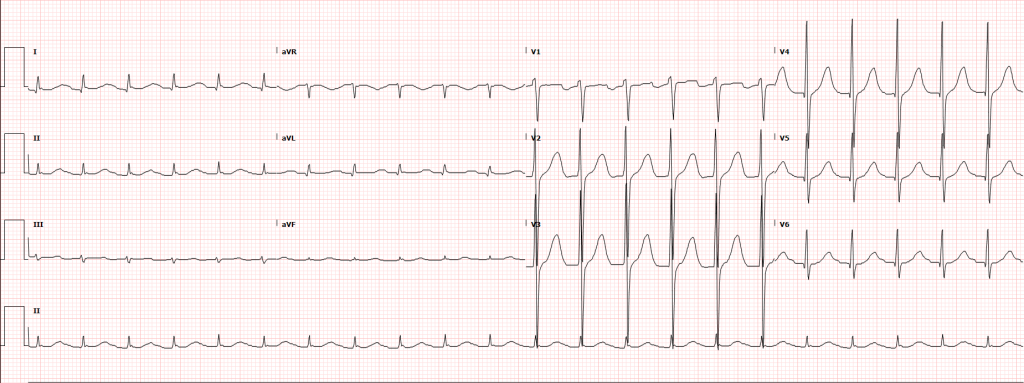
49M with a history of hypertension who presented to his primary physician for routine follow-up and was referred to the ED for an abnormal ECG. He denied chest pain, shortness of breath, or any limitation to baseline exercise tolerance. His vital signs were notable for systolic hypertension and his examination was unremarkable. A chest x-ray showed no acute cardiopulmonary findings. His initial ECG demonstrated a biphasic T-wave in V2 and deep, symmetric T-wave inversions in V3-V6. His initial serum troponin was markedly elevated at 3.499. He was admitted and urgent coronary angiography revealed proximal LAD stenosis (70%), mid-LAD stenosis (85%) and 1st right posterolateral stenosis (85%) which were stented. He was discharged on post-procedure day one and has remained asymptomatic at outpatient follow-up.
Initially described in 1982 where a subset of patients who did poorly with medical management of “impending myocardial infarction” (essentialy unstable angina) were found to have characteristic ECG changes. These patients were noted to be at increased risk for extensive anterior wall myocardial infarctions due to proximal LAD stenosis.
Criteria
- History of chest pain
- Normal or slightly-elevated cardiac enzymes
- No precordial Q-waves
- Isoelectric or <1mm ST-segment elevation
- Pattern present in pain-free state
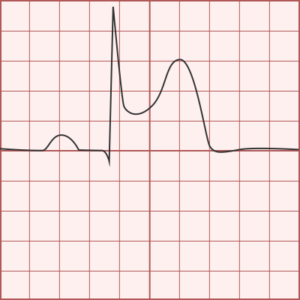
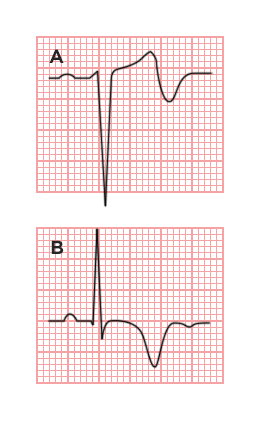
- Type A (25%): Biphasic T-wave in V2/V3
- Type B (75%): Deep, symmetrically inverted T-waves in V2/V3
Clinical Significance
Wellens Syndrome (or LAD coronary T-wave syndrome) represents a “pre-infarction” stage of coronary artery disease manifested by critical LAD stenosis. The natural history includes progression to extensive anterior wall myocardial infarction, often associated with severe left ventricular systolic dysfunction, cardiogenic shock and death. These changes may be mistaken for “non-specific” T-wave changes (which in the presence of a non-concerning history and typically non-elevated cardiac markers) may lead providers to inappropriate dispositions such a stress testing which is contraindicated. Recognition of this pattern and its appropriate management (urgent coronary angiography) is critical.
Case Summary
The case presented above is atypical. The patient had no history of chest pain and cardiac enzymes were significantly elevated – two features which are uncommon in Wellens Syndrome. However, the patient’s elevated cardiac biomarkers led to admission and angiography with identification of the characteristic proximal LAD stenosis (and other disease).
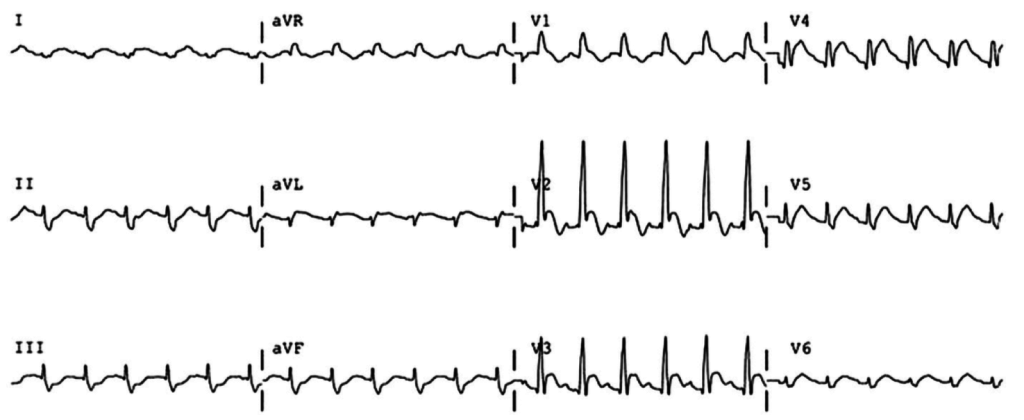
Nonsustained Ventricular Tachycardia
Case 1
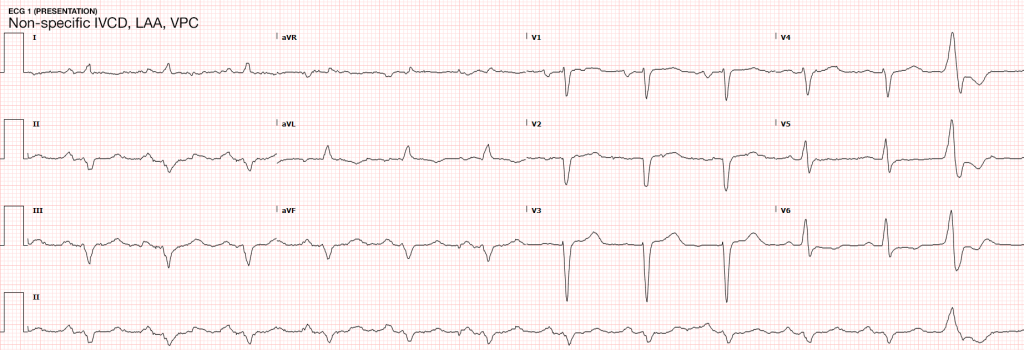
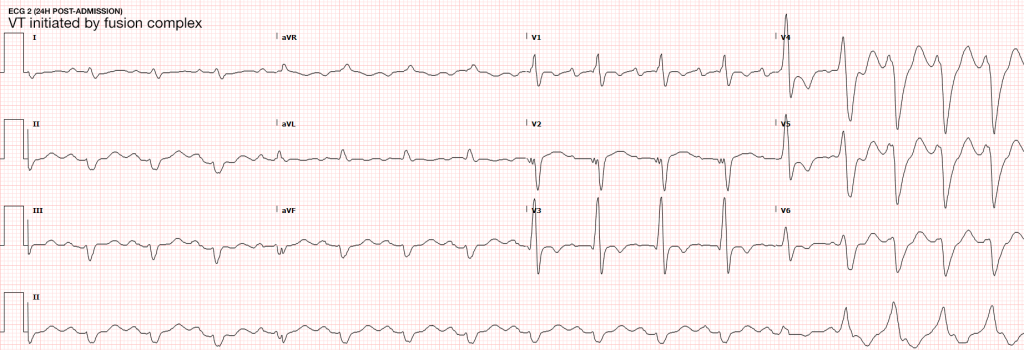
64M with a history of HFrEF (LVEF 20-25%), CAD, AICD (unknown indication), COPD, CKD III presenting with gradual onset shortness of breath, progressive bilateral lower extremity edema.
Examination consistent with severe acute decompensated heart failure presumed secondary to left ventricular dysfunction.
Telemetry monitoring with multiple episodes of nonsustained ventricular tachycardia.
In the ED, the patient developed worsening respiratory failure despite initiation of therapy, requiring endotracheal intubation. Continuous cardiac monitoring revealed persistent salvos of NSVT, progressing to slow ventricular tachycardia without device intervention.
Device interrogation revealed multiple events, 3 shocks, several ATP’s over the recorded period.
Evaluation and Management:
- NSVT with known (severe) ischemic heart disease
- For repetitive monomorphic ventricular tachycardia: amiodarone, beta-blockade (if tolerated), procainamide (IIA, C)
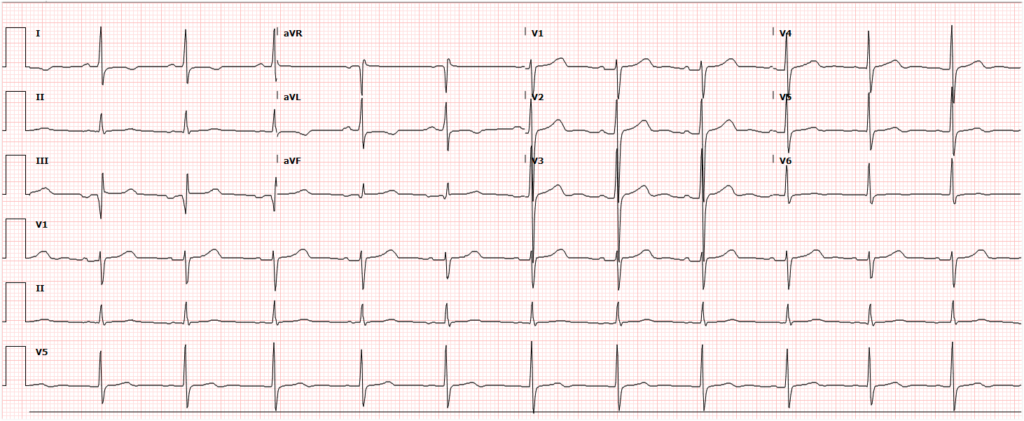
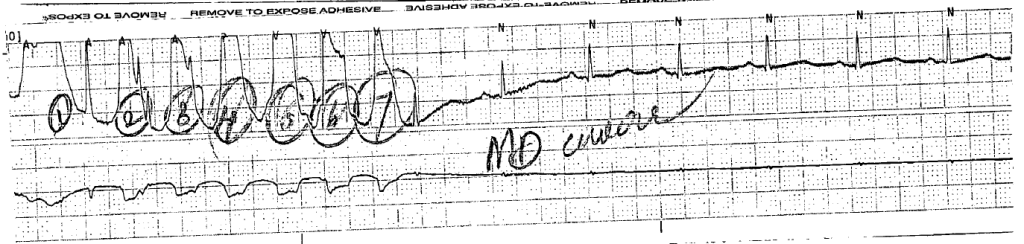
ECG’s
Case 2
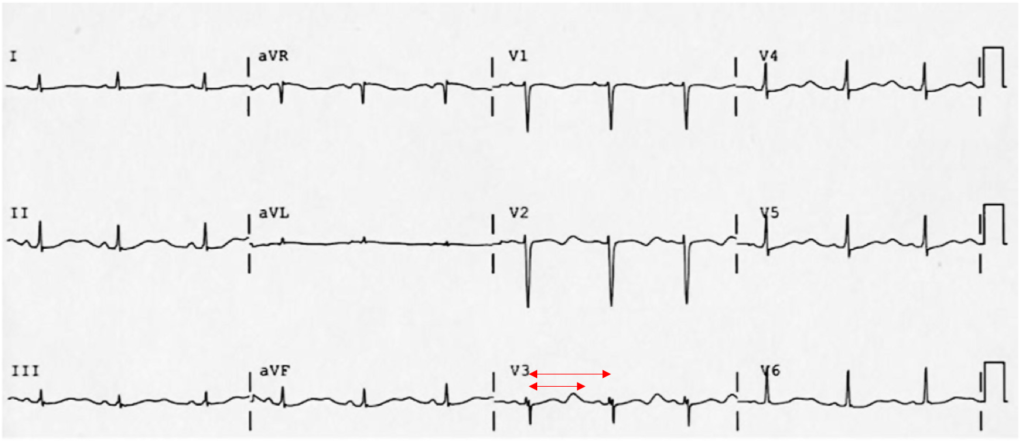
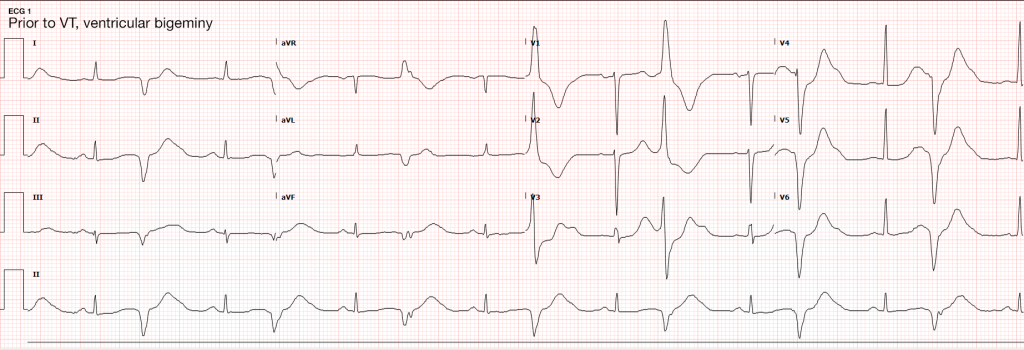
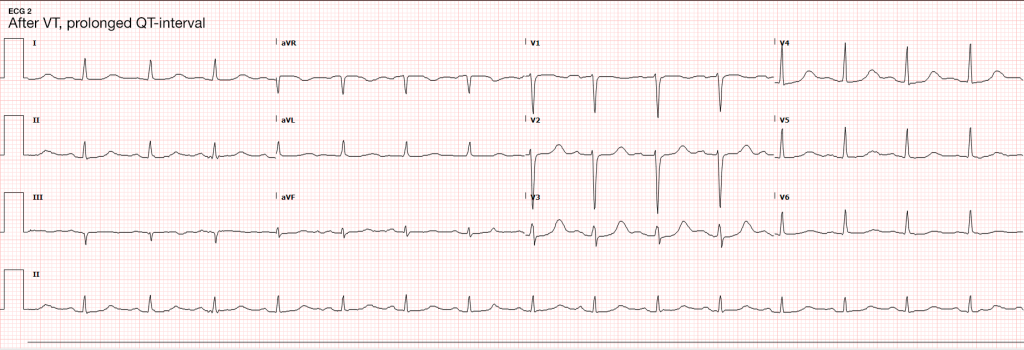
31F with the autoimmune polyglandular syndrome (adrenal, thyroid and endocrine pancreatic insufficiency), presenting with fever and cough.
Evaluation consistent with sepsis presumed secondary to the pulmonary source.
Telemetry monitoring initially with ventricular bigeminy, then nonsustained ventricular tachycardia.
In the ED, the patient developed pulseless ventricular tachycardia – apparently polymorphic. Chest compressions and epinephrine produced the return of spontaneous circulation with recovery to baseline neurologic function.
ECG revealed prolonged QTc and chemistry panel notable for critical hypokalemia/hypomagnesemia.
Evaluation and Management:
- NSVT progressing to VT
- Initially attributed to electrolyte disturbances. However, serial ECG’s continued to show prolonged QTc (possibly acquired, home medications included metoclopramide and erythromycin). Early echocardiography demonstrated global hypokinesis with EF 30-35% attributed to severe sepsis and recurrent defibrillation. Cardiac CT after resolution of acute illness showed persistently depressed ejection fraction without coronary atherosclerosis. The presence of NICM associated with malignant dysrhythmias warranted ICD placement.
- Cardioversion for hemodynamic compromise (I, B), B-blockade (I, B), amiodarone if no LQTS (I, C), urgent angiography if ischemia not excluded (I, C)1
- Correction of electrolyte abnormalities (specifically hypokalemia) may decrease progression to VF.
ECG’s
- > 3-5 consecutive beats originating below the AV node
- Rate > 100bpm
- Duration <30s
Epidemiology
-
- Occurs in 0-4% of ambulatory patients
- Increased frequency in males and with increasing age
In some patients, NSVT is associated with an increased risk of sustained tachyarrhythmias and sudden cardiac death. In others, it is of little prognostic significance.
Evaluation
- In all patients:History: including arrhythmogenic medications/substances, pertinent family historyPhysical examinationECG/CXRTTEIn selected patients exercise-testing advanced imaging (CT/C-MR)Electrophysiologic studies genetic testing
NSVT in the absence of structural heart disease
NSVT in Idiopathic Ventricular Tachycardia
- Ventricular outflow arrhythmias:
- RVOT: 70-80%, LBBB pattern
- LVOT: 20-30%, RBBB pattern
- Mechanism:
- Adrenergically mediated
- Occur during exercise, resolve as heart-rate increases, recur during recovery
- Management:
- Exclude arrhythmogenic right ventricular cardiomyopathy (imaging, myocardial biopsy)
- If symptomatic, beta-blockade, ± IC anti-arrhythmic, CCB (verapamil) for ILVT
- Prognosis:
- Good, rare tachycardia-induced cardiomyopathy, rare SCD
NSVT in Polymorphic Ventricular Tachycardia
- Mechanism
- LQTS (acquired or inherited)
- Familial catecholaminergic polymorphic VT
- Management
- Symptomatic (ex. syncope, cardiac arrest): ICD
- Asymptomatic QTc > 550ms: consider ICD
- Prognosis
- Increased risk SCD
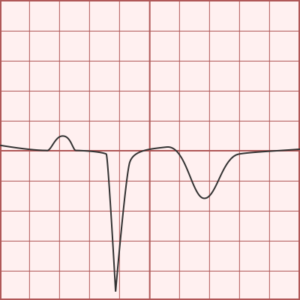
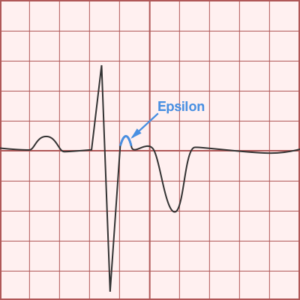
Arrhythmogenic Right Ventricular Cardiomyopathy
- Mechanism
- Fibrosis, fibro-fatty replacement of myocardium in RVIT/RVOT/RV apex
- May occur with only subtle structural abnormalities of the right ventricle
- LBBB morphology
- Management
- Anti-arrhythmias of limited utility
- Catheter ablation, ICD backup
- Prognosis
- Increased risk SCD
NSVT with apparent structural heart disease1
Hypertension and LVH
- Mechanism
- Stretch-induced abnormal automaticity
- Fibrotic tissue
- Presence of NSVT correlates with the degree of hypertrophy and subendocardial fibrosis
- Management
- Evaluation for ischemic heart disease
- Aggressive medical management of hypertension (including beta-blockade)
- Prognosis
- Unclear
Valvular Disease
- Mechanism
- High incidence in AS, severe MR (25%)
- Mechanical stress from dysfunctional valvular apparatus
- Management
- Beta-blockade if symptomatic
- Prognosis
- No evidence that NSVT is an independent predictor of SCD.
Ischemic Heart Disease9-14
- Mechanism
- Monomorphic VT associated with re-entry at the borders of ventricular scars
- Ischemia induces polymorphic NSVT/VF
- Management
- Revascularization, beta-blockade, statin, ACE/ARB
- MADIT I, MUSTT: ICD for ICM LVEF <40%, NSVT, EPS inducible VT
- MADIT II, SCD-HeFT: ICD for moderate-to-severe LV dysfunction irrespective of NSVT or EPS findings
- Prognosis
- NSTEMI with NSVT >48h after admission 2x risk SCD (MERLIN-TIMI 36)
- STEMI with NSVT common, not as predictive of ACM or SCD as LVEF (CARISMA)
- NSVT <24h after admission for NSTEMI/STEMI not of prognostic significance.
Hypertrophic Cardiomyopathy
- Mechanism
- Genetic myocardial disease
- Myocyte disarray, fibrosis, ischemia result in arrhythmogenic substrate
- Management
- (NSVT, LV thickness, FH SCD, syncope, abnormal BP response to exercise)
- Beta-blockade, anti-arrhythmic for symptoms
- Prognosis
- Increased risk SCD (1% annual)
Restriction of physical activity
Other Conditions
- Non-ischemic dilated cardiomyopathy
- Giant-cell myocarditis
- Repaired TOF
- Amyloidosis
- Sarcoidosis
- Chagas cardiomyopathy
Algorithm for the Evaluation of NSVT
Low Voltage ECG
The format of this article is atypical for the structure and concept of the website – but it’s always been about learning. Here is a simplified guide to ECG interpretation with a focus on the aspects I find more challenging to understand or recall.
Grid and Leads
Axis
Atrial Enlargement
- Normal:
- First portion of deflection is RA, second is LA
- Right Atrial Enlargement:
- P-wave amplitude > 2.5mm in inferior leads
- Normal duration P-wave
- Left Atrial Enlargement:
- P-wave duration increased (terminal negative portion >0.04s)
- Amplitude of terminal negative component >1mm below isoelectric line in V1
Ventricular Hypertrophy
- Right Ventricular Hypertrophy:
- Right axis deviation
- Abnormal R-wave progression
- Increased R-wave amplitude in leads overlying the right ventricle (V1)
- Increased S-wave amplitude in leads overlying the left ventricle (V6)
- Criteria
- V1: R>S
- V6: S>R
- Left Ventricular Hypertrophy:
- Left axis deviation
- Increased R-wave amplitude in leads overlying the LV (I, aVL, V5, V6)
- Increased S-wave amplitude in leads overlying the RV (V1)
- Criteria:
- Precordial Leads
- R-wave in V5/V6 + S-wave in V1/V2 > 35mm
- R-wave in V5 > 26mm
- R-wave in V6 > 20mm
- Limb Leads
- R-wave in aVL > 11mm
- R-wave in aVF > 20mm
- Combined
- R-wave in aVL + S-wave in V3 > 20mm (F), 28mm (M)
- Precordial Leads
Secondary Repolarization Abnormalities
- Downsloping ST-segment depression
- Asymmetric T-wave inversion
Bundle Branch Blocks
Left Bundle Branch Block
- QRS duration > 0.12s (3 boxes)
- Broad or notched R-wave with prolonged upstroke in I, aVL, V5, V6
- Associated ST-segment depression and T-wave inversion
- Reciprocal changes in V1, V2 (deep S-wave)
- Possible LAD
Right Bundle Branch Block
- QRS duration > 0.12s (3 boxes)
- RSR’ in V1, V2
- Reciprocal changes in I, aVL, V5, V6 (deep S-wave)
Hemiblocks
Other Blocks
- Non-specific intraventricular conduction delay: QRS >0.10s without BBB
- Incomplete BBB: LBBB/RBBB pattern with non-prolonged QRS
- Bifascicular block: RBBB + LAFB/LPFB (by axis deviation)
Ischemia and Infarction
- Hyperacute T-waves
- T-wave inversion: Symmetric, compared to TWI associated with repolarization abnormalities
- ST-elevation: Unlike J-point elevation, ST-segment merges with T-wave
- Q-waves
- Duration > 0.04s
- Amplitude > 1/3 R-wave
- Normal in aVR
Coronary Artery Territories
| DISTRIBUTION | CORONARY ARTERY | LEADS | RECIPROCAL CHANGES |
|---|---|---|---|
| 1. Inferior | RCA, PDA | II, III, aVF | Anterior, Lateral |
| 2. Lateral | LCx | I, aVL, V5, V6 | Inferior |
| 3. Anterior | LAD | V1-V6 | Inferior |
| 4. Posterior | RCA | Posterior | Anterior (esp. V1) |
References













Visitor Rating: 5 Stars