Diabetic Ulcer is a foot that exhibits any pathology that results directly from diabetes mellitus or any long-term (or “chronic”) complication of diabetes mellitus. Due to the peripheral nerve dysfunction associated with diabetes (diabetic neuropathy), patients have a reduced ability to feel pain.
Diabetes-related foot problems are common, and negatively impact patients’ quality of life. Therefore, it is important that pharmacists and healthcare professionals are aware of symptoms and the relevant care pathways for these patients to ensure they receive the best care and education regarding how to manage their condition.
Pharmacists and healthcare professionals should be aware of symptoms and the relevant care pathways for patients with diabetes-related foot problems. This includes advising patients to check their feet daily and how they can do this.
In the UK, around 4.5 million people have diabetes and an estimated 1.1 million people are living with diabetes but have not yet been diagnosed, which means that an estimated 6% of the UK population have the disease. Of those individuals who have been diagnosed, around 90% have type 2 diabetes and around 10% have type 1 diabetes.
The financial impact of diabetes on the UK NHS equates to around £10bn, 80% of which is spent on the complications of diabetes (see Box 1: Complications of diabetes), with foot ulceration considered to be one of the most serious complications. Foot ulceration is responsible for more hospital days than all other diabetes complications combined. The annual spend for diabetic foot ulceration and amputation is estimated to be just under £1bn, most of which is spent in primary, community and outpatient settings. Around £1 in every £140 of NHS spending in England is on footcare for people with diabetes.
Diagnosis of PAD
- The ankle-brachial index: The ankle-brachial index (ABI) is a simple bed-side screening tool for the presence of PAD. PAD simply depends on the calculation of the ratio between the systolic pressure of the ankle arteries and the systolic pressure at the brachial arteries[rx]. ABI is an inexpensive method that can assess the severity of PAD as it usually correlates with the patient’s reported symptoms and functional status. The normal range is of ABI is between 0.9-1.3, falsely elevated values of ABI can result in cases of calcified, non-compressible arteries. Thus the ABI method may lead to underestimation of the severity of the disease in patients with diabetes[rx].
- The toe-brachial index: The toe-brachial index is calculated similar to the ABI, where the systolic pressure is measured using a small cuff and a Doppler probe. Measuring the toe-brachial index is helpful especially in cases of ABI values more than 1.30, as the small arteries of the lower limb are less likely to be calcified. A toe-brachial index lower than 0.70 is diagnostic for PAD[rx].
- Segmental limb pressure assessment and pulse volume recordings: The technique depends on plethysmographic cuffs situated over the brachial arteries and different points on the lower limb. The extent and location of PAD can be detected from segmental systolic pressure assessment using a Doppler probe[rx].
- Ultrasound velocity spectroscopy and imaging: The normal arterial Doppler velocity shows a triphasic signal. When an arterial obstruction is present proximal to the probe, there is loss of the normal reversed flow component on transforming the waveform associated with decreased amplitude, attenuation of all parts of the spectrum and delayed upstroke[rx].
- Duplex ultrasound – depends on combining the B-mode and the pulsed Doppler ultrasound to assess arterial flow and localized velocity information at stenotic sites. Duplex ultrasonography is widely used nowadays detecting with high sensitivity and specificity the arterial patency and extends of obstruction[rx]. Duplex ultrasound has certain limitations mainly difficulty in identifying close multiple separate lesions, some difficulty when assessing infrapopliteal, common and external iliac arteries[rx].
- Transcutaneous oximetry and laser – doppler flowmetry: These techniques are used mainly to assess cutaneous blood flow. Cutaneous blood flow is usually normal until late stages of proximal arterial ischemia of the atherosclerotic type, thus, this type of vascular evaluation is not used in every day practice[rx].
- Magnetic resonance angiography (MRA)[rx].
- Computed tomographic angiography: CTA is superior to MRA as it can detect the presence of calcification, which is advantageous on planning revascularization strategies. The ACC/AHA guidelines recommend CTA on deciding the revascularization techniques in cases of PAD, offering faster image than MRA[rx].
- Contrast angiography: Although it is the gold standard for the diagnosis of PAD, is rarely required as a diagnostic tool due to the risks associated with invasive procedures. Computer-enhanced digital subtraction angiography can be useful in patients who present with localized stenosis so as to minimize the amount of contrast material injected and for better image resolution[rx].
CLASSIFICATION
- The presence of diabetic foot ulceration is the main leading risk for amputation in patients with diabetes. Proper assessment and classification of a diabetic foot ulcer is an essential part for the management of the diabetic foot. A prompt and adequate ulcer treatment may lead to foot amputation prevention, preserving the life quality of the patient.
Several classifications have been proposed for the categorization of diabetic foot ulcers. The most important ones are described below.
Wagner-Meggitt classification[rx]
It is one of the earliest and most widely used classifications. It classifies the diabetic foot ulceration depending on how deep the wound is, includes 6 grades
- (1) Grade 0: The skin is intact;
- (2) Grade 1: Presence of ulcer which is superficial;
- (3) Grade 2: Presence of ulcer which is deep;
- (4) Grade 3: Deep ulcer with abscess, bone involvement or osteomyelitis;
- (5) Grade 4: Gangrene in the forefoot; and
- (6) Grade 5: Whole foot gangrene.
Wagner-Meggitt classification has shown several disadvantages
- (1) cannot address all patterns of diabetic foot ulcerations and infections;
- (2) the presence of infection is addressed in only one stage, thus, the superficial ulcers if infected or ischemic are not properly categorized in this system; and
- (3) this system does not properly assess the presence of peripheral ischemia in categorization of foot ulcers.
The university of texas system[rx]
- It classifies diabetic foot ulcers into 4 grades (0-4) according to their depth, and then stages every grade of them according to the presence or absence of infection and ischemia (A-D).
- The University of Texas Classification has been validated and has prognostic advantages as it included both infection and ischemia but showed some difficulty in application in day to day practice.
The SAD classification[rx]
This classification grades the diabetic foot ulceration according to five ulcer features (size, depth, sepsis, arteriopathy, and denervation) on a 4-point scale (0-3).
- SAD classification differs from the other earlier systems by considering both size of ulcer and the presence of neuropathy. It has been validated by demonstrating differences between baselines variable and clinical outcome. Its major drawback is the complexity in practical use.
The pedis classification[rx]
The PEDIS system has been proposed by the International Working Group on the Diabetic Foot. This system grades the wound based on five features:
- (1) perfusion (arterial blood supply);
- (2) extent (area of the ulcer);
- (3) depth of the wound;
- (4) presence of infection; and
- (5) sensation.
The Infectious Diseases Society of America guidelines[rx]
These guidelines subclassified the infected diabetic foot into three categories:
- (1) mild: Involvement is restricted to skin and subcutaneous tissues;
- (2) moderate: Involvement is more extensive or affecting deeper tissues; and
- (3) Severe: Diabetic foot ulceration is accompanied by systemic signs of infection or metabolic decompensation.
PRINCIPLES OF DIABETIC FOOT ULCERS MANAGEMENT
Wound debridement
- Debridement of diabetic foot ulcers is an important initial step in the management of the wound. Several benefits can result from proper debridement including the removal of the necrotic and non-viable tissues and keeping a healthy granular wound bed. One should be careful on the assessment of the ulcer if ischemia is suspected. A revascularization intervention may be necessary before a debridement is performed. Debridement is also stimulating the release of growth factors to promote advancing healing edges[rx]. Various methods are used for wound debridement.
- Surgical debridement: It is the gold standard method in diabetic foot ulceration. To obtain optimal results, healthy tissue loss should be minimized, foot function should be preserved, and deformities which can precipitate a recurrence of ulcers should be prevented. Surgical debridement is typically done for ulcers with a large amount of necrotic and non-viable tissues. Debridement is performed using a scalpel blade with the tip pointed in a 45-degree angle or a tissue nipper to remove all necrotic and non-viable tissues until a bleeding healthy base is obtained[rx].
- Enzymatic debridement: Enzymatic debridement is based on the application of topical agents on the ulcer. These agents are usually applied once daily. Their action is based on necrotic tissue degradation using proteolytic digestive enzymes such as streptokinases, trypsin, papain, fibrinolysin-DNase, collagenase, papain-urea and streptodornase. Data from clinical studies have shown conflicting results about the efficacy of these topical agents, thus, their additional benefits to standard wound care remain unclear. Putting into consideration the need of the longtime application, as well as, the high cost, their use is usually limited to slowly soften large eschars or debridement of some decubitus ulcerations insensate limbs. In order to improve the efficacy of these agents, a scalpel blade is applied to crosshatch eschars[rx].
- Mechanical debridement: Although it is a simple and inexpensive tool, it can remove both viable and also non-viable tissues leading to pain in the sensate foot. The wet gauze dressing is applied to the wound bed and then kept to dry. The necrotic debris embedded in the gauze is mechanically stripped from the wound bed on gauze removal[rx].
- Biological debridement (Maggot therapy): Recently the use of Maggot therapy has re-emerged showing benefits in necrotic tissue debridement, decreasing bacterial load and stimulation of wound healing. Several studies showed the efficacy of Maggot therapy[rx].
- Other modalities: Ongoing research is evaluating other methods such as low energy ultrasound mist for the debridement of diabetic foot ulcers[rx].
MODERN WOUND CARE MODALITIES
In the recent years, apart from the standard wound care, new diabetic ulcer treatment modalities have been developed[rx].
Wound dressings
- The ideal wound dressing[rx]: (1) should be sterile and does not contaminate the ulcer with foreign particles; (2) should be readily available, easy to use and cost effective; (3) should keep a moist environment for adequate wound healing; (4) should be able to absorb excess exudates from the wound; (5) should not adhere to the wound floor, also should be non-allergic and non-toxic; (6) should be able to protect the wound from microorganisms and also provides mechanical protection; and (7) should maintain adequate tissue gaseous exchange and control wound odor.
Topical agents
- Wet to dry dressing (simple saline dressing): Wet to dry dressing is included in standard wound care and is considered a method for mechanical debridement, since it presents a good debriding effect in removal of the necrotic tissue and wound preparation[rx]. In order to minimize irritation and discomfort, adequate moistening of the dressings with normal saline is done when treating granulating wound tissues to avoid trauma and bleeding[rx].
- Local antibacterial agents: Antibacterial agents can be used alone or in combination with other dressings except for dry necrotic ulcers. For effective anaerobic coverage, metronidazole gel is used and maintains a moist environment for wound healing[rx]. Several antibiotics have effective antibacterial action on topical application such as Neomycin, Gentamycin, and Mupirocin. Silver dressings and polyherbal topical preparations have shown good antibacterial action[rx]. For effective antibacterial action against Pseudomonas, other gram-negative bacilli, and beta hemolytic streptococci wound infections Sisomycin and acetic acid can be used. Special precautions should be considered when using povidone iodine solution dressings, iodine has been found to be toxic at high concentrations to bacteria and fungi as well as human cells[rx].
- Tulle dressings: Tulle dressings are used mainly for skin grafts and superficial wounds. They can be safely used in granulating and epithelializing tissues as they are impregnated with paraffin, having low dressing adherence properties[rx]. Evidence from several previous studies have shown better and faster re-epithelialization rates compared to dry dressing[rx].
- Hydrogel dressings: Hydrogel dressings are considered the best choice for dry wounds with necrotic eschar. Hydrogels provide fluid and good hydration to dry and slough wounds. Although they are very good at absorbing exudates, they should be avoided in diabetic foot planter ulcers as they may cause maceration of the skin surrounding the wound[rx].
- Polyurethane films: Polyurethane films are transparent films coated with a water-proof adhesive dressing. They provide permeable films allowing diffusion of gases and vapor thus an adequately moist wound environment. They have the advantage of being transparent, thus can monitor the wound progression. They also can be used for low exudates wounds, but they may cause maceration of the skin surrounding the wound[rx].
- Polyurethane foam: Polyurethane foam is highly used in diabetic foot ulcers. It can absorb large amounts of exudates in a non-adherent nature thus does not cause wound sloughing or trauma on removal. They maintain moisture environment thus allow proper preparation of wound bed and promotes better wound healing[rx].
- Alginate dressings: Two forms of alginate dressings are available; calcium alginate and calcium sodium alginate. Alginate dressings can absorb large amounts of exudates up to 20 times their weight as shown by several clinical studies[rx].
- Honey-impregnated dressings: The anti-inflammatory and anti-microbial actions have been shown in vitro studies but further studies are required to support strong evidence in vivo[rx].
Growth factors
- Growth factors have shown promising results in diabetic ulcer healing. Growth factors stimulate angiogenesis, cellular proliferation and migration, together with promoting enzymatic production. Several growth factors have been studied including; platelet-derived growth factor (PDGF), epidermal growth factor (EGF), transforming growth factor (TGF)-β, TGF-α and insulin-like growth factor…, etc.[rx]. A recombinant human (rh)-PDGF dressing is available for diabetic foot lesions when added to conventional[rx]. EGF in the form of local injections of rh-EGF showed favorable results in neuropathic vs ischemic ulceration[rx].
- The Food and Drug Administration (FDA) announced some warnings regarding the use of a recombinant human platelet-derived growth factor, which contains becaplermin. In both clinical studies and post marketing users, becaplermin was associated with malignancies distant from the application site. Also increased mortality rate from systemic malignancies was reported on using 3 or more tubes of becaplermin gel. Topical enzymes: Several prepared ointments containing enzymes such as fibrinolysin, collagenase or papain have been used in enzymatic debridement of the sloughy tissues and promoting granulation tissue formation. Papain-urea has shown better enzymatic debridement effect when compared to collagenase[rx].
- Vacuum-assisted closure: Vacuum-assisted devices have shown efficacy in exudates removal and edema reduction. Ideally a pressure of 125 mmHg can generate a negative topical pressure over the diabetic foot wound. It has the advantage of leaving the wound surface moist. It has several limitations; it is contraindicated in cases of osteomyelitis, ischemia, deep tissues exposure such as tendons, bones and blood vessels, presence of necrotic tissues and fistulas[rx]. Vacuum-assisted devices are also effective in promoting closure and wound healing in patients with treated infections and treated osteomyelitis[rx].
- Hyperbaric oxygen therapy, Do we have evidence A systemic treatment where oxygen is breathed but at a higher pressure than the local atmospheric pressure[rx]. HBOT has shown increased healing rates of diabetic foot ulcers, however it still controversial whether it can be used as adjuvant treatment or not[rx]. Hyperbaric oxygen therapy (HBOT) have the advantage of reduction of tissue hypoxia, edema, increase angiogenesis and erythrocytes deformability, antimicrobial effects and increase fibroblastic activity[rx]. HBOT is approved as an adjunctive treatment to be used in chronic non-healing ulcers by the Undersea and Hyperbaric Medical Society[rx]. The European Committee for Hyperbaric Medicine has set a type 2 recommendation for the use of HBOT in the management of diabetic foot ulcers including patients with ischemic wounds without a surgically treatable arterial lesion or as a complement after vascular surgery, in presence of non-healing wounds[rx].
- The role of stem cell therapy in PAD: It is worth mentioning that our skeletal muscles have a regenerative capacity as the have multipotentaial and progenitor cells. In cases of critical limb peripheral arterial disease, the transplantation of progenitor cells- derived from bone marrow- has beneficial effects on angiogenesis and ulcer healing as shown in phase I and II studies. The role therapeutic angiogenesis is a promising and a safe method for management of PAD and limb salvage[rx].
Complications of diabetic Foot
Risk factors for foot ulceration
-
Peripheral neuropathy
-
Somatic
-
Autonomic
-
Peripheral vascular disease
-
Proximal and/or distal disease
-
Past history of foot ulcers/amputation
-
Other long-term complications
-
End-stage renal disease (especially on dialysis)
-
Post-transplant (including pancreas/kidney transplant)
-
Visual loss
-
Plantar callus
-
Foot deformity
-
Ethnic background
-
Poor social background
More common contributory factors shown in bold
Plantar Callus
- Plantar callus forms under weight-bearing areas as a consequence of the dry skin (autonomic neuropathy) insensitivity and repetitive moderate stress from high foot pressures. Callus itself acts as a foreign body and can cause ulceration in the insensate foot.
Elevated Foot Pressures
- Numerous studies have confirmed the contributory role that abnormal plantar pressures play in the pathogenesis of foot ulceration (1, 2, 7, 11). Most studies used sophisticated techniques such as pedobarography to assess foot pressures, but these are not required in day to day clinical practice.
Foot Deformities
- A combination of motor neuropathy, cheiro-arthropathy and altered gait pressures is thought to result in the “high-risk” neuropathic foot with clawing of the toes, prominent metatarsal heads, high arch and small muscle wasting.
Demographics
- In Western countries, the male sex has been associated with a 1.6-fold increased risk of foot ulcers (10). There is an increased risk of foot ulceration with increasing age and duration of diabetes.
There are many short- and long-term complications that can result from diabetes. High blood sugars (hyperglycaemia) and the length of time that diabetes is present increase the risk of complications, which include:
- Damage to nerves (neuropathy);
- Damage to the eyes (retinopathy);
- Damage to the kidneys (nephropathy);
- Damage to the cardiovascular system.
There may also be an associated increased risk of infection, depression and Alzheimer’s disease.
Within the foot, complications include:
- Peripheral arterial disease (PAD);
- Neuropathy;
- Foot deformity;
- Charcot neuroarthropathy;
- Active foot problems.
Testing for these conditions forms part of the annual foot assessment that is part of a patient’s annual diabetic review, which is conducted by a suitably trained individual.
The Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Study at 30 years:
- Diabetes is the most common cause of non-traumatic limb amputations, with 80% of cases being preceded by foot ulcers and, therefore, are considered preventable. The number of people with diabetes who, in any given week, have an active foot ulceration is estimated to be around 60,000–75,000 in England, and around 5–7% of people with diabetes will experience a foot ulcer at some point in their life. Mortality rates are high, with 50% of patients dying within five years of developing a diabetic foot ulcer, which rises to 70% if the patient has an amputation because this is believed to be associated with cardiovascular disease.
- Owing to the high prevalence and financial burden of foot problems that are related to diabetes, in addition to the impact on patients’ quality of life, it is important that pharmacists and healthcare professionals are aware of symptoms and the relevant care pathways for these patients to ensure they receive the best care and education regarding how to manage their condition.
Foot complications
Peripheral arterial disease (PAD)
- Atherosclerotic occlusive disease of the lower extremities, peripheral arterial disease (PAD) leads to inadequate blood supply to the lower limb, decreases peripheral tissue viability and increases the skin’s susceptibility to minor trauma, impairs wound healing and increases the risk of infection. If not caught early, it can result in necrosis or gangrene and loss of limb. The incidence of PAD in patients with diabetes is more severe and diffuse, often at a younger age, with calcification occurring more distally, and is related to an increased risk of mortality and impaired quality of life compared with people without diabetes.
- It has been reported that PAD is a factor in a third of foot ulcers and is a significant risk factor in re-ulceration. Information on vascular assessment of the foot is covered later.
Neuropathy

Peripheral neuropathy (PN)
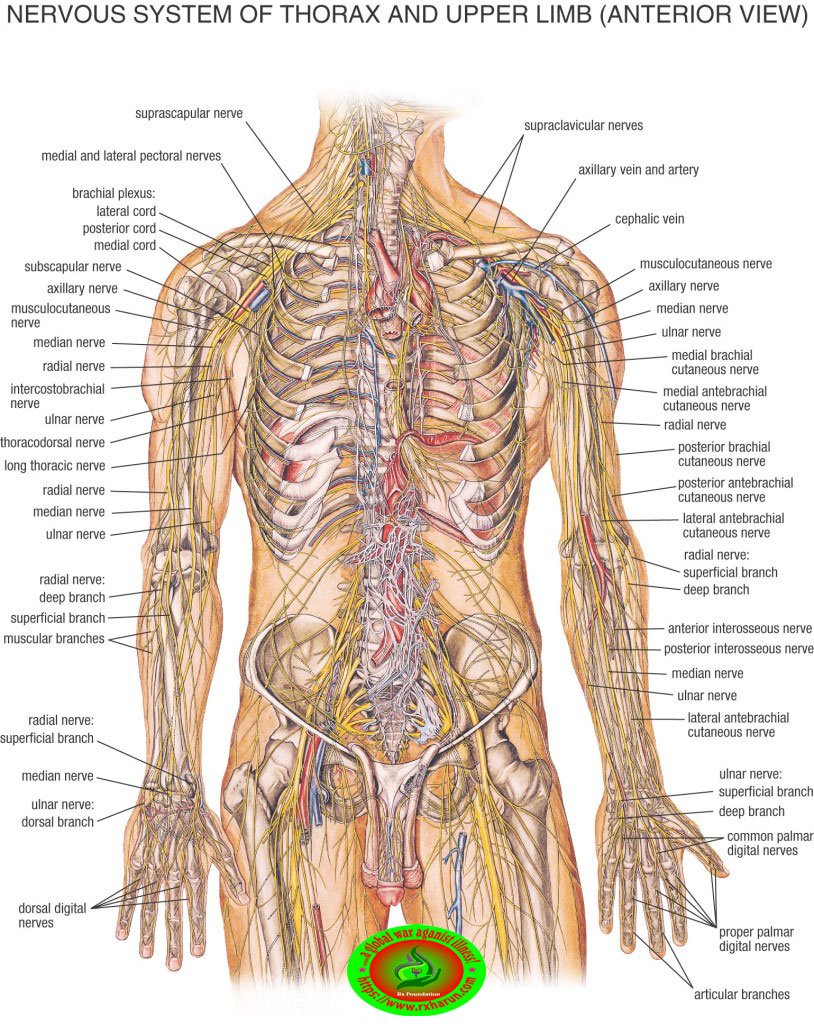
- Develops when nerves in the extremities are damaged. The exact aetiopathogenesis of PN is still not fully understood but recent evidence suggests that vascular dysfunction, with changes to the blood supply of the nerves, could be responsible.
- PN is reported to affect 50% of patients with diabetes, and its prevalence increases with age and duration of diabetes. It is present in more than 50% of patients with type 2 diabetes aged over 60 years and in more than 40% of patients who have had type 1 diabetes for 20 years.
- PN may be the most important pathological precursor of foot ulcers, with neuropathy reportedly present in 90% of patients with diabetes who also have a foot ulcer.
- The most common form of PN is distal symmetrical polyneuropathy. This involves the sensory, motor and autonomic nerve fibres, where the earliest changes tend to occur most distally (i.e. in the digits and progress proximally).
Sensory neuropathy
- Results in the loss of pain and thermal perception, and is usually asymptomatic. The patient is, therefore, unaware that they cannot appreciate the sensation of pain and, thus, are unaware that an injury has been sustained. As a result, foot pathologies such as corns, calluses, thickened nails and foot deformity (e.g. hallux abducto valgus [bunion]) all pose a risk. Without pain sensation, these pathologies may be left unnoticed (and therefore untreated), causing underlying tissue damage and ulceration.
- Healthcare professionals will test a patient’s foot sensations as part of their diabetic annual foot assessment (see later section on assessing a diabetic foot at risk) However, it is imperative to inform patients about the importance of wearing shoes that fit properly — sensory loss renders an individual unable to detect rubbing or trauma from an ill-fitting shoe. In fact, people with neuropathy may actually wear shoes that are too small, as they perceive them to be a good fit.
Diabetic peripheral neuropathic pain (DPNP)
- It is estimated to affect between 16% and 26% of all people with diabetes. It is under-reported and undertreated, with 80% of patients experiencing moderate to severe pain. Patients complain of paraesthesia, shooting pains down the legs, lancinating pains, burning, hyperaesthesia, allodynia, metatarsalgia, and sensations of cold or warmth, more commonly at night.
- Its aetiology is unknown but there is some evidence that age, duration of diabetes, nephropathy, PAD and an increased waist circumference can be possible predictors for the development of painful neuropathy.
- The National Institute for Health and Care Excellence (NICE), England’s health technology assessment body, recommends duloxetine as first-line treatment for DPNP, with further recommendations for the combination of drugs if duloxetine monotherapy fails. However, first-line treatment is not always possible because of polypharmacy, with patients already being on a number of medicines.
Motor neuropathy
- Affects the nerves that control movement. This results in wasting of the intrinsic muscles of the foot. One study, using magnetic resonance imaging, found that small muscle wasting is common in a neuropathic foot, leading to a cavoid foot type This typically presents as a high arched foot with clawed toes, causing increased pressure to be placed on metatarsal heads and apices of digits, which results in callus formation and, thus, further pressure distribution, disruption, and risk.
Autonomic neuropathy
- Affects involuntary functions, such as thermo-regulation and sweat production. Damage to these nerves leads to lack of adequate moisture in the skin, which results in loss of elasticity, dry skin, callus and fissuring It also results in arterio-venous shunting where oxygen bypasses capillary beds and sends oxygenated blood into the venous system, resulting in deprivation of oxygen and nutrients to tissues
Assessment and identification of a diabetic foot at risk
- A standard clinical examination will identify most patients at risk of foot ulceration. To assess a patient’s risk status of developing a foot ulcer, healthcare professionals look for the following: neuropathy, PAD, ulceration, callus, infection and/or inflammation, deformity, gangrene and Charcot arthropathy.
- Patients with diabetes should receive an annual foot check-up as part of their care. However, Diabetes UK reports that only 36% of diabetic patients receive a full annual assessment and patients are not getting a good quality foot check or being advised of their risk status for developing foot ulcers.
- Assessment not only includes examination of the lower limbs and feet, but of the patient as a whole, including their history, foot pathology, and vascular and neurological assessment. Patients should be reminded to have their feet checked by a relevant healthcare professional at least once a year.
Taking the patient’s history
- Long-term studies on people with type 1 and type 2 diabetes have shown that the longer the person has had diabetes or if they have poorly controlled diabetes, they are at an increased risk of complications, such as PAD and neuropathy.
- Therefore, duration and the patient’s diabetes control status are an important part of the history taking, as well as lifestyle factors such as smoking (which is considered to be the greatest modifiable factor in reducing the incidence of PAD).
- Other co-morbidities may provide clues to the potential development of foot complications. Furthermore, poor eyesight reduces the ability to self-care and renders the individual unable to conduct daily visual checking of their own feet. Foot ulceration is more common in those with a previous history of ulceration or amputation, with rates of re-ulceration as much as 40% within 1 year, 60% at 3 years, and as high as 65% at 5 years.
- Indeed, it has been argued that the term ‘remission’ should be used rather than ‘healed’ when a foot ulcer is resolved. An individual with diabetes who is on dialysis (renal replacement therapy) has an increased risk of lower limb complications and are, therefore, considered high-risk Patients at increased or high risk should be referred to the Foot Protection Service.
Podiatric observation and assessment
Early intervention and treatment of any foot pathology can reduce a patient’s risk of developing a foot problem that has the potential to become ulcerative. When assessing the foot, the following should be checked:
- Are the nails thickened or discoloured?
- What condition is the skin in?
The most common condition reported on a person’s skin with diabetes are cutaneous infections (mainly fungal), followed by dry skin, which has been shown to be more prevalent with poor diabetes control.
If these conditions are observed in a patient with diabetes, it is important to refer them to an appropriate healthcare professional (e.g. podiatrist or GP) for advice/treatment to prevent simple pathologies causing tissue breakdown.
Vascular assessment
- The pulses in the foot must be tested. The dorsalis pedis (DP) is found dorsally between the first and second metatarsal shafts and the tibialis posterior (PT) is found behind the medial malleolus. However, the absence of pulses alone may not indicate the presence of PAD. Further tests need to be carried out and an onwards referral should be made.
- The capillary filling time following pressure applied to the skin on the apices of digits, enough to blanch and a return of normal colour, should occur within five seconds. Slower rates may indicate inadequate blood flow. No blanching in a cyanotic foot is a dangerous sign and gangrene may follow. The reliability of this test has been questioned, but it does form part of the suggested PAD examination within the NICE guidance and is widely used.
Colour of the skin (e.g. white, brick red, cyanotic); absence of hair; loss of tissue viability and elasticity; atrophy; and dry skin are all indicators of potential vascular impairment and should form part of a vascular foot assessment.
Neurological assessment
Screening for neuropathy in patients with diabetes is vital as the vast majority of neuropathic patients are asymptomatic. Various tests can be used and assessment can be divided into three categories: small, large and motor fibre tests. Small fibres are responsible for sensations such as pain and temperature perception, whereas large fibres are responsible for vibration, light touch and pressure.
- The 10g monofilament – is the most commonly used tool for screening of neuropathy in the foot. The monofilament should avoid areas of callus, with various combinations of test sites recommended (from 3 to 10), but no agreed consensus. However, the plantar metatarsal pad and terminal phalanges of toes are common areas for neuropathic ulceration and are the areas that are tested whether it is 3 points or 10 points that are tested. Combining the monofilament testing with clinical examination for deformity and palpation of pulses enables the identification of patients who are 32-times more likely to ulcerate More information can be found here
- The Ipswich touch test – was devised to be able to assess for neuropathy without the use of aids (e.g. a monofilament), which could be a barrier for testing for neuropathy in some areas. Using the index finger, light touch is applied to the apex of the first, third and fifth toes on both feet. If two or more sites are not felt, the patient is considered to have neuropathy.
Risk status and referral
Following a full assessment, a patient’s risk status is determined using the NICE guidance
| Table 1: Assessing a patient’s risk status for developing a diabetic foot problem | |
|---|---|
| Risk status | Recommended review |
| Low risk
No risk factors present except callus |
Annual |
Moderate risk
|
3–6 months with foot protection service |
High risk
|
1–2 months or 1–2 weeks if have a concern with foot protection service |
Active diabetic foot problem
|
Refer the person within 1 working day to the multidisciplinary foot care service or foot protection service (according to local protocols and pathways; also see recommendation) for triage within 1 further working day |
Active ulceration/Charcot neuroarthropathy
- Often referred to as ‘Charcot foot’, Charcot neuroarthropathy affects the bones/joints and soft tissues of the foot, which in the first stages presents as inflammation (i.e. a hot, red and swollen foot; sometimes painful; see Figure 1). It is found where there is neuropathy, of which diabetes is the most common aetiology.
- It is a potentially devastating condition that can lead to severe deformity of the affected foot, the most common of which is the ‘rocker-bottom type foot’, where there is a ‘disorganisation’ of bone leading to deformity as shown in Figure 1.
- If suspected, urgent referral within one working day to a multidisciplinary team is recommended to provide non-weight bearing treatment until a diagnosis is made
Figure 1: Charcot foot
- X-ray of later stage Charcot foot, described as ‘rocker-bottom type foot’, where there is ‘disorganisation’ of the bone that results in deformity. The inset image shows the initial stages of Charcot foot, where the foot presents as red, hot and swollen.
- If a foot ulcer is detected either by a healthcare professional or patient, a referral should be made within 24 hours to a multidisciplinary diabetic foot team, as shown in table 1.
- Ulcers can be neuropathic (60–70%), often occurring on the apex of toes and plantar aspect of the foot; ischaemic (15–20%), which are often found on the lateral medical borders of the foot as a result of rubbing; or a combination of both, which is known as neuroischaemic (15–20%).
NICE also recommends that healthcare professionals should be aware that if a person with diabetes fractures their foot or ankle, it may progress to Charcot arthropy.
Wound assessment and management
Different wound classifications systems are used to evaluate a wound for communication between healthcare professionals and to evaluate and improve outcomes. Both the University of Texas Wound Classification System and the SINBAD Wound Classification System are recommended by NICE
| Table 2: University of Texas Wound Classification System | |
|---|---|
| Grade | |
| 0 | Completely epithelialised pre-or post-ulcerative lesions |
| 1 | Superficial wounds penetrating through the epidermis only or both the epidermis and dermis |
| 2 | Wounds penetrating into tendon or capsule but not bone |
| 3 | Wounds penetrating to bone or into joint |
| Stage | |
| A | No infection or ischaemia |
| B | Infection only present |
| C | Ischaemia only present |
| D | Both infection and ischaemia present |
| Table 3: SINBAD Wound Classification System | ||
|---|---|---|
| Site | Forefoot
Midfoot and hindfoot |
0
1 |
| Ischaemia | Pedal blood flow evident (one pulse present)
Clinical evidence of reduced blood flow |
0
1 |
| Neuropathy | Protective sensation intact
Protective sensation absent |
0
1 |
| Bacterial infection | None
Present |
0
1 |
| Area | Ulcer <1cm2
Ulcer >1cm2 |
0
1 |
| Depth | Ulcer affects cutaneous tissue
Ulcer reaching tendon; muscle or deeper |
0
1 |
| Total possible score | 6 | |
- The classic signs of infection may not be present in a diabetic foot ulcer because of the high incidence of PAD and neuropathy. Therefore, healthcare professionals need to be more mindful of subtle signs: increase in wound exudate, friable granulation tissue, malodour and undermining of the wound
Treatment
- Offloading has been shown to significantly heal more neuropathic ulcers; the gold standard of which is a total contact cast. However, it is not advocated where there is PAD and/or infection, and alternative treatment strategies should be sought, such as a heel offloading device until revascularisation allows for a cast.
Dressings
- There is no strong evidence on wound care for a diabetic foot ulcer, and NICE recommends that further good quality research is needed in this area
Health education
- Structured patient education has shown to improve diabetes control however, there is no evidence that the same is true for foot health education. Although it is considered that it is an important part of prevention and treatment of diabetic foot ulceration.
- Patients should be provided with both written and oral information on basic foot care advice (including footwear), the importance of foot care, foot emergencies and who to contact, and their individual risk of developing a foot problem. Leaflets are available on various websites, such as.
- A recent study identified that diabetes increases the risk for cognitive dysfunction and dementia, and people with a diabetic foot ulcer struggle even more with their ability to retain health information. This may explain non-adherence, which is important for a good clinical outcome. However, further research is needed to support this.
The role of pharmacists and other healthcare professionals
In June 2017, NHS England published the ‘RightCare pathway’ for diabetes, which includes “core components of an optimal diabetes service”.
- Seven key areas have been identified providing guidance for commissioners on improving outcomes for individuals with diabetes. One of the key areas identified was a reduction of major amputations (above or below the knee). It recommends that there is a triage to specialist services (30% of hospitals do not have a multidisciplinary team); a Root Cause Analysis of amputations with an outcome measure of a reduction in major amputations.
- The ‘National diabetes foot care audit’, published in March this year, demonstrated that delayed referral was associated with an increased risk of amputation and that those individuals who self-referred (30%) were less likely to have severe ulceration.
- With this in mind, it is important that pharmacists and healthcare professionals know their local diabetic foot pathways (e.g. are there any podiatry drop-in clinics or multi-disciplinary diabetic foot clinics in their area) for individuals who are at risk of developing a foot ulcer or who have an active foot ulceration.
- Pharmacists and healthcare professionals should also consider what local guidance is available, such as specific guidance for antibiotics prescribing for diabetic foot ulceration, especially if they are a non-medical prescriber.
Simple measures for all pharmacists and healthcare professionals who come into contact with people with diabetes include:
- Advising patients to check their feet daily;
- Advising patients to apply moisturising cream to dry areas but not between the toes;
- Advising patients to choose footwear that accommodates the shape and size of the foot to prevent rubbing or shearing;
- Advising patients never to walk barefoot (to prevent standing on anything that could traumatise or injure the foot);
- Advising patients to seek early advice as soon as a foot problem is identified (the National Diabetic Foot Care Audit demonstrates that this leads to shorter healing times and reduces the likelihood of amputation);
- Asking the patient if they have had a recent foot check as part of their annual assessment and, if they have not, advising them to have one, as well as how to perform daily foot checks themselves (see Box 2: Daily foot checks and footwear advice).
Box 2: Daily foot checks and footwear advice
- Check feet daily;
- For patients with reduced mobility or flexibility, using a mirror can be helpful to check the foot for changes. Alternatively, asking a friend or relative can be beneficial;
- Be aware of loss of sensation;
- Look for changes in the shape of the foot;
- Look for discolouration of the foot;
- Do not use corn removing plasters or blades;
- Look after toenails and ensure these are cut straight across;
- Wear shoes that fit properly;
- Examine shoes for sharp objects or stones before putting them on and replace ruffled innersole linings;
- Avoid socks, stockings or tights with wrinkles or prominent seams, or socks with holes or darned areas;
- Garters and stockings or socks with elastic tops should be avoided because they may restrict the circulation;
- Attend annual foot reviews.
Assessment, education and early appropriate intervention are key components in preventing and treating diabetic foot ulceration. As 80% of amputations are preceded by ulcers, it is hoped that appropriate early intervention can reduce this number.
References