Back pain is a common disorder involving the muscles, nerves, and bones of the back. Pain can vary from a dull constant ache to a sudden sharp feeling. Low back pain may be classified by duration as acute (pain lasting less than 6 weeks), sub-chronic (6 to 12 weeks), or chronic (more than 12 weeks). The condition may be further classified by the underlying cause as either mechanical, non-mechanical, or referred pain. The symptoms of low back pain usually improve within a few weeks from the time they start, with 40-90% of people completely better by six weeks.
Types of Back Pain
Low back pain can be broadly classified into four main categories
- Musculoskeletal – mechanical (including muscle strain, muscle spasm, or osteoarthritis); herniated nucleus pulposus, herniated disk; spinal stenosis; or compression fracture. Most commonly this is due to injury to the spine, intervertebral discs, or soft tissues. Fractures such as spondylolisthesis can be both an acute or chronic process. Lumbago often is labeled as acute back pain or a strain to either the quadratus lumborum muscle or the paraspinal muscles. Disc herniation is a common type of traumatic back pain. Pregnancy is also a mechanical cause of back pain.
- Degenerative – Osteoarthritis of the spine include facet joint osteoarthritis, sacroiliac joint osteoarthritis, spinal stenosis, and degenerative disc disease. Furthermore, osteoporotic compressive fractures are also a degenerative process.
- Inflammatory – HLA-B27 associated arthritis including ankylosing spondylitis, reactive arthritis, psoriatic arthritis, and inflammatory bowel disease. This is caused primarily due to inflammatory (seronegative) spondyloarthropathies such as ankylosing spondylitis. Sacroiliitis is most commonly seen. The pathophysiology of back pain depends on the etiology. Most often, it may be a part of an acute inflammatory process.
- Oncologic – This is caused by lytic lesions to the spine, cancers of the marrow, or compressive nerve phenomena from adjacent space-occupying lesions. Often presenting as a pathological fracture.
- Malignancy – bone metastasis from lung, breast, prostate, thyroid, among others
- Infectious – osteomyelitis; abscess. Infections of the spine, discs, epidural abscesses, or muscular/soft tissue abscesses
In addition, symptoms of lower back pain are usually described by the type of onset and duration
- Acute pain – This type of pain typically comes on suddenly and lasts for a few days or weeks, and is considered a normal response of the body to injury or tissue damage. The pain gradually subsides as the body heals.
- Subacute low back pain – Lasting between 6 weeks and 3 months, this type of pain is usually mechanical in nature (such as a muscle strain or joint pain) but is prolonged. At this point, a medical workup may be considered and is advisable if the pain is severe and limits one’s ability to participate in activities of daily living, sleeping, and working.
- Chronic back pain – Usually defined as lower back pain that lasts over 3 months, this type of pain is usually severe, does not respond to initial treatments, and requires a thorough medical workup to determine the exact source of the pain.
According to the body movement or spinal mechanism
Three common classifications of back pain include:
- Axial pain – Also called mechanical pain, axial pain is confined to one spot or region. It may be described a number of ways, such as sharp or dull, comes and goes, constant, or throbbing. A muscle strain is a common cause of axial back pain as are facet joints and annular tears in discs.
- Referred pain – Often characterized as dull and achy, referred pain tends to move around and vary in intensity. As an example in the lower back, degenerative disc disease may cause referred pain to the hips and posterior thighs.
- Radicular pain – Commonly described as electric shock-like or searing, radicular pain follows the path of the spinal nerve as it exits the spinal canal. This type of pain is caused by compression and/or inflammation to a spinal nerve root. In the lower back (lumbar spine), radicular pain may travel into the leg. Other terms for radicular pain are sciatica or radiculopathy (when accompanied by weakness and/or numbness). It can be caused by conditions such as a herniated disc, spinal stenosis, or spondylolisthesis.
Causes of Back Pain
- Bulging or herniated disc – A disc may bulge outward. A herniated disc occurs when the soft interior matter escapes through a crack or ruptures through the disc’s protective outer layer. Both disc problems can cause nerve compression, inflammation, and pain.
- Spinal stenosis – develops when the spinal canal or a nerve passageway abnormally narrows.
- Spinal arthritis – also called spinal osteoarthritis or spondylosis, is a common degenerative spine problem. It affects the spine’s facet joints and may contribute to the development of bone spurs.
- Spondylolisthesis – occurs when a lumbar (low back) vertebral body slips forward over the vertebra below it.
- Vertebral fractures – (burst or compression types) are often caused by some type of trauma (eg, fall).
- Osteomyelitis – is a bacterial infection that can develop in one of the spine’s bones.
- Spinal tumors – are an abnormal growth of cells ( a mass) and are diagnosed as benign (non-cancerous) or malignant (cancer).
- Sprains and strains – account for most acute back pain. Sprains are caused by overstretching or tearing ligaments, and strains are tears in tendon or muscle. Both can occur from twisting or lifting something improperly, lifting something too heavy, or overstretching. Such movements may also trigger spasms in back muscles, which can also be painful.
- Intervertebral disc degeneration – is one of the most common mechanical causes of low back pain, and it occurs when the usually rubbery discs lose integrity as a normal process of aging. In a healthy back, intervertebral discs provide height and allow bending, flexion, and torsion of the lower back. As the discs deteriorate, they lose their cushioning ability.
- Herniated or ruptured discs – can occur when the intervertebral discs become compressed and bulge outward (herniation) or rupture, causing low back pain.
- Radiculopathy – is a condition caused by compression, inflammation and/or injury to a spinal nerve root. Pressure on the nerve root results in pain, numbness, or a tingling sensation that travels or radiates to other areas of the body that are served by that nerve. Radiculopathy may occur when spinal stenosis or a herniated or ruptured disc compresses the nerve root.
- Sciatica – is a form of radiculopathy caused by compression of the sciatic nerve, the large nerve that travels through the buttocks and extends down the back of the leg. This compression causes shock-like or burning low back pain combined with pain through the buttocks and down one leg, occasionally reaching the foot. In the most extreme cases, when the nerve is pinched between the disc and the adjacent bone, the symptoms may involve not only pain but numbness and muscle weakness in the leg because of interrupted nerve signaling.
- A traumatic injury – such as from playing sports, car accidents, or a fall can injure tendons, ligaments or muscle resulting in low back pain. Traumatic injury may also cause the spine to become overly compressed, which in turn can cause an intervertebral disc to rupture or herniate, exerting pressure on any of the nerves rooted in the spinal cord.
- Skeletal irregularities – include scoliosis, a curvature of the spine that does not usually cause pain until middle age; lordosis, an abnormally accentuated arch in the lower back; and other congenital anomalies of the spine.
- Abdominal aortic aneurysms – occur when the large blood vessel that supplies blood to the abdomen, pelvis, and legs becomes abnormally enlarged. Back pain can be a sign that the aneurysm is becoming larger and that the risk of rupture should be assessed.
- Kidney stones – can cause sharp pain in the lower back, usually on one side. Low back pain is rarely related to serious underlying conditions, but when these conditions do occur, they require immediate medical attention.
- Infections – are not a common cause of back pain. However, infections can cause pain when they involve the vertebrae, a condition called osteomyelitis; the intervertebral discs, called discitis; or the sacroiliac joints connecting the lower spine to the pelvis, called sacroiliitis
- Cauda equina syndrome – is a serious but rare complication of a ruptured disc. It occurs when disc material is pushed into the spinal canal and compresses the bundle of lumbar and sacral nerve roots, causing loss of bladder and bowel control. Permanent neurological damage may result if this syndrome is left untreated.
- Inflammatory diseases of the joints – such as arthritis, including osteoarthritis and rheumatoid arthritis as well as spondylitis, an inflammation of the vertebrae, can also cause low back pain. Spondylitis is also called spondyloarthritis or spondyloarthropathy.
- Osteoporosis – is a metabolic bone disease marked by a progressive decrease in bone density and strength, which can lead to painful fractures of the vertebrae.
- Endometriosis – is the buildup of uterine tissue in places outside the uterus.
- Fibromyalgia, – a chronic pain syndrome involving widespread muscle pain and fatigue.
Red flag historic or physical exam features that, when present, should raise the provider’s suspicion for a process that may require imaging for proper diagnosis. These differ slightly from adults to children based on the incidence of diseases in these age groups:
-
Lumbosacral muscle strains/sprains
-
Presentation: follows traumatic incident or repetitive overuse, pain worse with movement, better with rest, restricted range of motion, tenderness to palpation of muscles
-
-
Lumbar spondylosis
-
patient typically is greater than 40years old, pain may be present or radiate from hips, pain with extension or rotation, the neurologic exam is usually normal
-
-
Disk herniation
-
usually involves the L4 to S1 segments, may include paresthesia, sensory change, loss of strength or reflexes depending on severity and nerve root involved
-
-
Spondylolysis, Spondylolisthesis
-
similar to pediatrics, spondylolisthesis may present back pain with radiation to the buttock and posterior thighs, neuro deficits are usually in the L5 distribution
-
-
Vertebral compression fracture
-
localized back pain worse with flexion, point tenderness on palpation, may be acute or occur insidiously over time, age, chronic steroid use, and osteoporosis are risk factors
-
-
Spinal stenosis
-
back pain, which can be accompanied by sensory loss or weakness in legs relieved with rest (neurologic claudication), neuro exam can be within normal limits or can have progressive loss of sensation, as well as weakness.
-
-
Tumor
-
history of metastatic cancer, unexplained weight loss, focal tenderness to palpation in the setting of risk factors
-
97% of spinal tumors are metastatic disease; however, the provider should keep multiple myeloma in the differential
-
-
Infection: vertebral osteomyelitis, discitis, septic sacroiliitis, epidural abscess, paraspinal muscle abscess
-
The spinal procedure within the last 12 months, Intravenous drug use, Immunosuppression, prior lumbar spine surgery, fever, wound in the spinal region, localized pain, and tenderness
-
The granulomatous disease may represent as high as one-third of cases in developing countries.
-
-
Fracture
-
Significant trauma (relative to age), Prolonged corticosteroid use, osteoporosis, and age greater than 70 years, Contusions, abrasions, tenderness to palpation over spinous processes
-
Pediatrics[rx]][rx]:
-
Tumor
-
fever, malaise, weight loss, nighttime pain, recent onset scoliosis
-
Osteoid osteoma is the most common tumor that presents with back pain – classically, the pain is promptly relieved with anti-inflammatory drugs such as NSAIDs
-
-
Infection: vertebral osteomyelitis, discitis, septic sacroiliitis, epidural abscess, paraspinal muscle abscess
-
fever, malaise, weight loss, nighttime pain, recent onset scoliosis
-
Epidural abscess should be a consideration with the presence of fever, spinal pain, and neurologic deficits or radicular pain; discitis may present with a patient refusing to walk or crawl
-
-
A herniated disk, slipped apophysis
-
Acute pain, radicular pain, positive straight leg raise test, pain with spinal forward flexion, recent onset scoliosis
-
-
Spondylolysis, spondylolisthesis, lesion or injury to the posterior arch
-
Acute pain, radicular pain, positive straight leg raise test, pain with spinal extension, tight hamstrings
-
-
Vertebral fracture
-
acute pain, other injuries, traumatic mechanism of injury, neurologic loss
-
-
Muscle strain
-
acute pain, muscle tenderness without radiation
-
-
Scheuermann’s kyphosis
-
chronic pain, rigid kyphosis
-
-
Inflammatory spondyloarthropathies
-
chronic pain, morning stiffness lasting greater than 30min, sacroiliac joint tenderness
-
-
Psychological Disorder (conversion, somatization disorder)
-
normal evaluation but persistent subjective pain
-
-
Idiopathic Scoliosis:
-
positive Adam’s test (for more significant angle curvature), most commonly asymptomatic
-
Of note, no definitive evidence that scoliosis causes pain, but patients with scoliosis have more frequently reported pain; therefore the provider should rule out other causes before attributing pain to scoliosis
-
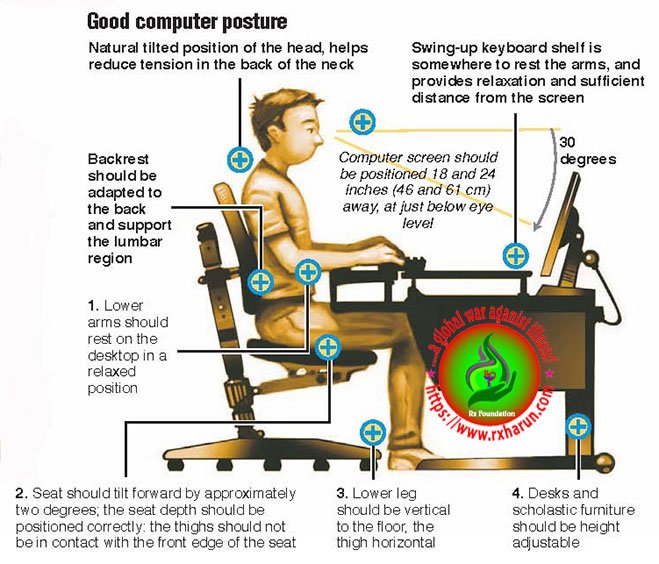
Everyday activities or poor posture.
Back pain can also be the result of some everyday activity or poor posture. Examples include:
- Bending awkwardly
- Pushing something
- Pulling something
- Carrying something
- Lifting something
- Standing for long periods
- Bending down for long periods
- Twisting
- Coughing
- Sneezing
- Muscle tension
- Over-stretching
- Straining the neck forward, such as when driving or using a computer
- Long driving sessions without a break, even when not hunched
The Symptom of Back Pain
The main symptom of back pain is, as the name suggests, an ache or pain anywhere on
- Pain in the back, and sometimes all the way down to the buttocks and legs. Some back issues can cause pain in other parts of the body, depending on the nerves affected.
- In most cases, signs, and symptoms clear up on their own within a short period. If any of the following signs or symptoms accompany back pain, people should see their doctor:
- Pain. It may be continuous, or only occur when you are in a certain position. The pain may be aggravated by coughing or sneezing, bending or twisting.
- Patients who have been taking steroids for a few months
- Drug abusers
- Patients with cancer
- Patients who have had cancer
- Patients with depressed immune systems
- Stiffness.
According to the British National Health Service (NHS), the following groups of people should seek medical advice if they experience back pain:
- Weight loss
- Elevated body temperature (fever)
- Inflammation (swelling) on the back
- Persistent back pain – lying down or resting does not help
- Pain down the legs
- Pain reaches below the knees
- A recent injury, blow or trauma to your back
- Urinary incontinence – you pee unintentionally (even small amounts)
- Difficulty urinating – passing urine is hard
- Fecal incontinence – you lose your bowel control (you poo unintentionally)
- Numbness around the genitals
- Numbness around the anus
- Numbness around the buttocks
- Dull ache,
- Numbness,
- Tingling,
- Sharp pain,
- Pulsating pain,
- Pain with movement of the spine,
- Pins and needles sensation,
- Muscle spasm,
- Tenderness,
- Sciatica with shooting pain down one or both lower extremities
- People aged less than 20 and more than 55 years
- Additionally, people who experience pain symptoms after a major trauma (such as a car accident) are advised to see a doctor. If low back pain interferes with daily activities, mobility, sleep, or if there are other troubling symptoms, medical attention should be sought.
Risk increases with
- Biomechanical risk factors.
- Sedentary occupations.
- Gardening and other yard work.
- Sports and exercise participation, especially if infrequent.
- Obesity.
Preventive measures
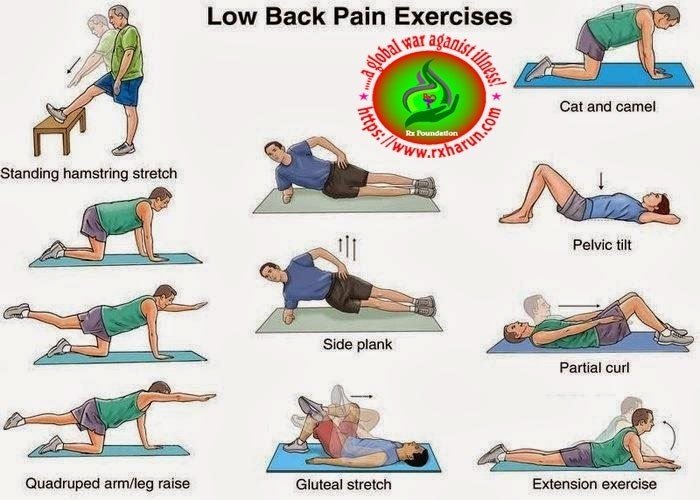
- Exercises to strengthen lower back muscles.
- Learn how to lift heavy objects.
- Sit properly.
- Back support in bed.
- Lose weight, if obese.
- Choose proper footwear.
- Wear special back support devices.
Red flag conditions indicating possible underlying spinal pathology or nerve root problemsw9
Red flags
-
Non-mechanical pain (unrelated to time or activity)
-
Thoracic pain
-
Previous history of carcinoma, steroids, HIV
-
Feeling unwell
-
Weight loss
-
Widespread neurological symptoms
-
Structural spinal deformity
Indicators for nerve root problems
-
Unilateral leg pain > low back pain
-
Radiates to foot or toes
-
Numbness and paraesthesia in the same distribution
-
The straight leg raising test induces more leg pain
-
Localized neurology (limited to one nerve root)
Diagnosis of Back Pain
Diagnosis of back pain is following
- The physical exam – is also performed similarly between the age groups as long as the patient is old enough to communicate and participate in the review. The physical exam should include inspection, palpation, the range of motion, strength testing, provocative maneuvers, and neurologic (limb strength, sensation, and deep tendon reflex) assessments. Several provocative exercises help demonstrate or decrease suspicion of different processes.
- A straight leg raise (SLR) – can be complete by raising the patient’s leg to 30 to 70 degrees. Ipsilateral leg pain at less than 60 degrees is a positive test for lumbar disk herniation. The likelihood ratio (LR) of a straight leg raise is 2, with ave likelihood ratio (NLR) of 0.5. If the pain reproduction occurs contralaterally, it is a positive test for a lumbar disk herniation with LR of 3.5 and NLR of 0.72.[rx][rx][rx]
- One leg hyperextension test/stork test – Have the patient stand on one leg and (while being supported by the provider) have them hyper-extend their back. Repeat this maneuver on both sides. Pain with hyperextension is positive for a pars interarticularis defect.[rx]
- Adam test – Have the patient bend over with feet together and arms extended with palms together. The practitioner should observe from the front. If a thoracic lump is present on one side or the other, it is an indication of scoliosis.[rx]
Radiography
Suspected disk, nerve, tendon, and other problems – X-rays or some other imaging scan, such as a CT (computerized tomography) or MRI (magnetic resonance imaging) scan may be used to get a better view of the state of the soft tissues in the patient’s back.
- Blood tests – CBC ,ESR,Hb, RBS,CRP, Serum Creatinine,Serum Electrolyte,
- Myelograms
- Discography.
- Electrodiagnostics
- Bone scans
- Ultrasound imaging
- X-rays – can show the alignment of the bones and whether the patient has arthritis or broken bones. They are not ideal for detecting problems with muscles, the spinal cord, nerves or disks.
- MRI or CT scans – these are good for revealing herniated disks or problems with tissue, tendons, nerves, ligaments, blood vessels, muscles, and bones.
- Bone scan – a bone scan may be used for detecting bone tumors or compression fractures caused by brittle bones (osteoporosis). The patient receives an injection of a tracer (a radioactive substance) into a vein. The tracer collects in the bones and helps the doctor detect bone problems with the aid of a special camera.
- Electromyography or EMG – the electrical impulses produced by nerves in response to muscles is measured. This study can confirm nerve compression which may occur with a herniated disk or spinal stenosis (narrowing of the spinal canal).
| Syndrome | Findings | Assessment/Plan |
|---|---|---|
| Facet syndrome | History and physical examination:
Radiological findings (not indicated on initial evaluation):
|
Differential diagnosis:
Treatment: |
| Sacro-iliac joint syndrome | History and physical examination:
Radiological findings (not indicated on initial evaluation):
|
Functional disturbance: muscular imbalance Treatment: stabilizing exercises, analgesics (1–3 days) if needed, manual medicine, sacroiliac joint injection if indicated |
| Myofascial pain syndrome | History and physical examination:
Radiological and histological findings:
|
Local treatment: |
| Functional instability | History and physical examination:
Radiological findings:
|
|
Treatment of Back Pain
Not all treatments work for all conditions or for all individuals with the same condition, and many find that they need to try several treatment options to determine what works best for them. The present stage of the condition (acute or chronic) is also a determining factor in the choice of treatment. Only a minority of people with back pain (most estimates are 1% – 10%) require surgery.
Non-medical
Treatment for back pain generally depends on how long your pain lasts
Acute (short-term) back pain – usually gets better on its own. Exercises or surgery are usually not recommended for this type of pain. There are some things you may try while you wait for your pain to get better:
- Acetaminophen, aspirin, or ibuprofen will help ease the pain.
- Get up and move around to ease stiffness, relieve pain, and have you back doing your regular activities sooner.
Chronic (long-term) back pain – is typically treated with non-surgical options before surgery is recommended.
Nonsurgical Treatments
- Pain relievers – that are taken by mouth or applied to the skin. Examples include acetaminophen and aspirin. Your doctor may suggest steroid or numbing shots lessen your pain. Involves using pulleys and weights to stretch the back, which may allow a bulging disk to slip back into place. Your pain may be relieved while in traction, although pain returns once you aren’t in traction.
- Practice healthy habits – such as exercise, relaxation, regular sleep, proper diet, and quitting smoking.
- Manipulation – Professionals use their hands to adjust or massage the spine or nearby tissues.
- Compression packs – Many people with back pain find that using either hot or cold compression packs helps reduce pain. You can make you own cold compression pack by wrapping a bag of frozen food in a towel. Hot compression packs are often available from larger pharmacies. You may find it useful to use one type of pack after the other.
- Acupressure – A therapist applies pressure to certain places in the body to relieve pain. Acupressure has not been well studied for back pain. Move your body properly while you do daily activities, especially those involving heavy lifting, pushing, or pulling. Back pain is generally treated with non-pharmacological therapy first, as it typically resolves without the use of medication. Superficial heat and massage, acupuncture, and spinal manipulation therapy may be recommended.
- Heat therapy – is useful for back spasms or other conditions. A review concluded that heat therapy can reduce symptoms of acute and sub-acute low-back pain.
- Regular activity and gentle stretching exercises – are encouraged in uncomplicated back pain, and are associated with better long-term outcomes. Physical therapy to strengthen the muscles in the abdomen and around the spine may also be recommended.
- These exercises – are associated with better patient satisfaction, although it has not been shown to provide functional improvement. However, one study found that exercise is effective for chronic back pain, but not for acute pain. If used, they should be performed under the supervision of a licensed health professional.
- Massage therapy – may give short-term pain relief, but not functional improvement, for those with acute lower back pain. It may also give short-term pain relief and functional improvement for those with long-term (chronic) and sub-acute lower pack pain, but this benefit does not appear to be sustained after 6 months of treatment. There does not appear to be any serious adverse effects associated with massage.
- Acupuncture – may provide some relief for back pain. However, further research with stronger evidence needs to be done.
- Spinal manipulation – is a widely-used method of treating back pain, although there is no evidence of long-term benefits.
- Back school – is an intervention that consists of both education and physical exercises. A 2016 Cochrane review found the evidence concerning back school to be very low quality and was not able to make generalizations as to whether back school is effective or not.
The Medication
If non-pharmacological measures are not effective, medications may be tried.
- NSAIDs – Prescription-strength drugs that reduce both pain and inflammation. Pain medicines and anti-inflammatory drugs help to relieve pain and stiffness, allowing for increased mobility and exercise. There are many common over-the-counter medicines called non-steroidal anti-inflammatory drugs (NSAIDs). They include mainly or first choice etodolac, then aceclofenac, etoricoxib, ibuprofen, and naproxen.
- Muscle Relaxants – These medications provide relief from spinal muscle spasms. Muscle relaxants, such as baclofen, tolperisone, eperisone, methocarbamol, carisoprodol, and cyclobenzaprine, may be prescribed to control muscle spasms.
- Neuropathic Agents – Drugs(pregabalin & gabapentin) that address neuropathic—or nerve-related—pain. This includes paresthesia, radiating pain with numbness, diabetic neuropathy pain, myalgia, burning, numbness, and tingling sensation
- Calcium & vitamin D3 – To improve bone health and healing fracture. As a general rule, men and women age 50 and older should consume 1,200 milligrams of calcium a day, and 600 international units of vitamin D a day.
- Vitamin B1, B6, and B12 – It is essential for neuropathic pain management, pernicious anemia, with vitamin b complex deficiency pain, paresthesia, numbness, itching with diabetic neuropathy pain, myalgia, etc.
- Skeletal muscle relaxers – may also be used. Their short term use has been shown to be effective in the relief of acute back pain. However, the evidence of this effect has been disputed, and these medications do have negative side-effects.
- In people with nerve root pain and acute radiculopathy – there is evidence that a single dose of steroids, such as dexamethasone, may provide pain relief.
- Epidural corticosteroid injection – (ESI) is a procedure in which steroid medications are injected into the epidural space. The steroid medications reduce inflammation and thus decrease pain and improve function. ESI has long been used to both diagnose and treat back pain, although recent studies have shown a lack of efficacy in treating low back pain.
- Carisoprodol – This muscle relaxant was investigated in two high-quality studies on acute low back pain. The first study compared carisoprodol with diazepam [rx]. Carisoprodol was superior in performance on all the outcome parameters measured. A comparison of carisoprodol with cyclobenzaprine‐hydrochloride in the second study revealed no statistically significant differences between the two treatments [rx].
- Chlorzoxazone – This muscle relaxant was compared with tizanidine in one high-quality study in a very small sample of patients with degenerative lumbar disc disease [rx]. No differences were found between the treatments.
- Cyclobenzaprine‐hydrochloride – Cyclobenzaprine was compared with diazepam in a low-quality trial on chronic low back pain, but no significant differences between the treatments were identified [rx]. There was also no significant difference between cyclobenzaprine and carisoprodol in one high-quality study on acute low back pain [rx].
- Diazepam – In comparison with carisoprodol, diazepam was found to be inferior in performance on muscle spasm, global efficacy and functional status in a high-quality trial on acute low back pain [rx]. In a very small high-quality trial (30 people) comparing diazepam with tizanidine, there were no differences in pain, functional status and muscle spasm after seven days [rx].
- Tizanidine – This muscle relaxant was compared with chlorzoxazone and diazepam in two very small high quality [rx]. Both trials did not find any differences in pain, functional status and muscle spasm after 7 days.
- Pridinol mesylate – One low-quality trial showed no differences between this muscle relaxant and thiocolchicoside on pain relief and global efficacy.
Surgery of Back Pain
Surgery for back pain is typically used as a last resort when the serious neurological deficit is evident. A 2009 systematic review of back surgery studies found that, for certain diagnoses, surgery is moderately better than other common treatments, but the benefits of surgery often decline in the long term. Surgery may be an option to treat cases of chronic back pain when:
- there is an identifiable cause, such as a ruptured hernia,
- the symptoms have not responded to other forms of treatment, and
- the symptoms are getting progressively worse.
The type of surgery that will be recommended will depend on the cause of your back pain. Some surgical options are listed below.
NIH’s National Institute of Neurological Disorders and Stroke (NINDS) lists the following as some of the surgical options for low back pain. But NINDS also cautions that “there is little evidence to show which procedures work best for their particular indications.”
- Vertebroplasty and kyphoplasty – These procedures are used to repair compression fractures of the vertebrae caused by osteoporosis. Both procedures include the injection of glue-like bone cement that hardens and strengthens the bone.
- Spinal laminectomy/spinal decompression – This is performed when spinal stenosis causes a narrowing of the spinal canal that results in pain, numbness, or weakness. The surgeon removes the bony walls of the vertebrae and any bone spurs, aiming to open up the spinal column to remove pressure on the nerves.
- Discectomy – This procedure is used to remove a disk when it has herniated and presses on a nerve root or the spinal cord. Laminectomy and discectomy are frequently performed together.
- Foraminotomy – In this procedure, the surgeon enlarges the bony hole where a nerve root exits the spinal canal to prevent bulging discs or joints thickened with age from pressing on the nerve.
- Nucleoplasty also called plasma disk decompression – This laser surgery uses radiofrequency energy to treat people with low back pain associated with a mildly herniated disk. The surgeon inserts a needle into the disk. A plasma laser device is then inserted into the needle and the tip is heated, creating a field that vaporizes the tissue in the disk, reducing its size and relieving pressure on the nerves.
- Spinal fusion – The surgeon removes the spinal disk between two or more vertebrae, then fuses the adjacent vertebrae using bone grafts or metal devices secured by screws. Spinal fusion may result in some loss of flexibility in the spine and requires a long recovery period to allow the bone grafts to grow and fuse the vertebrae together.
- Artificial disk replacement – This is considered an alternative to spinal fusion for the treatment of people with severely damaged disks. The procedure involves the removal of the disk and its replacement by a synthetic disk that helps restore height and movement between the vertebrae.
Some surgical treatments are not recommended by NINDS, which cautions, for example, that intradiscal electrothermal therapy is “of questionable benefit.” NINDS notes that radiofrequency denervation provides only temporary pain relief and that “evidence supporting this technique is limited.”
As with all surgical procedures, spinal surgery carries some risks. For example, following surgery, there is a 10% chance of infection. If this occurs, further surgery may be required to clean out the infection, although some cases can be treated with antibiotics.
In the case of fusion surgery, there is a 1-2% chance of the vertebrae failing to fuse into place. If this occurs, further surgery will be required.
There is a very low risk that your spinal cord will be damaged during surgery. The chances of this happening are estimated to be six in 1,000 (0.6%). In the rare situation that the spinal cord is damaged during surgery, it could result in problems ranging from some muscle weakness to total paralysis. Your bladder and bowel control may also be affected.
Before having back surgery, your surgeon will be able to fully discuss the risks and benefits of the procedure with you.
Lower back pain exercises
A series of exercise routines you can do to help reduce any lower back pain (occasionally referred to as low back pain), including tension, stiffness, and soreness. These exercises from physiotherapists and BackCare expert Nick Sinfield help to stretch, strengthen and mobilize the lower back. When starting out, go gently to get used to the movements and work out how far you can go into each position without feeling pain.
Aim to do this routine at least once a day if the pain allows. You can complement this routine with walking, cycling and water-based activities. You are advised to seek medical advice before starting these back pain exercises and to stop immediately if you feel any pain.
Bottom to heels stretch
Stretches and mobilizes the spine
Start position: Kneel on all fours, with your knees under hips and hands under shoulders. Don’t over-arch your lower back. Keep your neck long, your shoulders back and don’t lock your elbows.
Action: Slowly take your bottom backward, maintaining the natural curve in the spine. Hold the stretch for one deep breath and return to the starting position.
Repeat 8 to 10 times.
Tips:
- Avoid sitting back on your heels if you have a knee problem.
- Ensure correct positioning with the help of a mirror.
- Only stretch as far as feels comfortable.
Knee rolls
Stretches and mobilizes the spine
Start position: Lie on your back. Place a small flat cushion or book under your head. Keep your knees bent and together. Keep your upper body relaxed and your chin gently tucked in.
Action: Roll your knees to one side, followed by your pelvis, keeping both shoulders on the floor. Hold the stretch for one deep breath and return to the starting position.
Repeat 8 to 10 times, alternating sides.
Tips:
- Only move as far as feels comfortable.
- Place a pillow between your knees for comfort.
Back extensions
Stretches and mobilizes the spine backward
Start position: Lie on your stomach, and prop yourself on your elbows, lengthening your spine. Keep your shoulders back and neck long.
Action: Keeping your neck long, arch your back up by pushing down on your hands. You should feel a gentle stretch in the stomach muscles as you arch backward. Breathe and hold for 5 to 10 seconds. Return to the starting position.
Repeat 8 to 10 times.
Tips:
- Don’t bend your neck backward.
- Keep your hips grounded.
Deep abdominal strengthening
Strengthens the deep supporting muscles around the spine
Start position: Lie on your back. Place a small, flat cushion or book under your head. Bend your knees and keep your feet straight and hip-width apart. Keep your upper body relaxed and your chin gently tucked in.
Action: As you breathe out, draw up the muscles of your pelvis and lower abdominals, as though you were doing up an imaginary zip along your stomach. Hold this gentle contraction while breathing from your abdomen for 5 to 10 breaths, and relax.
Repeat 5 times.
Tips:
- This is a slow, gentle tightening of the lower abdominal region. Don’t pull these muscles in using more than 25% of your maximum strength.
- Make sure you don’t tense up through the neck, shoulders or legs.
Pelvic tilts
Stretches and strengthens the lower back
Start position: Lie on your back. Place a small, flat cushion or book under your head. Bend your knees and keep your feet straight and hip-width apart. Keep your upper body relaxed and your chin gently tucked in.
Action: Gently flatten your low back into the floor and contract your stomach muscles. Now tilt your pelvis towards your heels until you feel a gentle arch in your lower back, feeling your back muscles contracting and return to the starting position.
Repeat 10 to 15 times, tilting your pelvis back and forth in a slow rocking motion.
Tips:
- Keep your deep abdominals working throughout.
- Don’t press down through the neck, shoulders or feet.
Modification
- Place one hand on your stomach and the other under your lower back to feel the correct muscles working
Prevention
Preventing back pain
To avoid back pain, you must reduce excess stresses and strains on your back and ensure that your back is strong and supple.
If you have persistent, recurring bouts of back pain, the following advice may be useful:
- Lose any excess weight
- Practise the Alexander technique.
- Wear flat shoes with cushioned soles, as these can reduce the stress on your back.
- Avoid sudden movements or muscle strain.
- Try and reduce any stress, anxiety and tension.
Posture
How you sit, stand and lie down can have an important effect on your back. The following tips should help you maintain a good posture:
- Standing – you should stand upright, with your head facing forward and your back straight. Balance your weight evenly on both feet and keep your legs straight.
- Sitting – you should be able sit upright with support in the small of your back. Your knees and hips should be level and your feet should be flat on the floor (use a footstool if necessary). Some people find it useful to use a small cushion or rolled-up towel to support the small of the back. If you use a keyboard, make sure your forearms are horizontal and your elbows are at right angles.
- Driving – make sure your lower back is properly supported. Correctly positioning your wing mirrors will prevent you from having to twist around. Foot controls should be squarely in front of your feet. If driving long distances, take regular breaks so you can stretch your legs.
- Sleeping – your mattress should be firm enough to support your body while supporting the weight of your shoulders and buttocks, keeping your spine straight. If your mattress is too soft, place a firm board – ideally 2cm thick – on top of the base of your bed and under the mattress. Support your head with a pillow, but make sure your neck isn’t forced up at a steep angle.
Exercise
Exercise is both an excellent way of preventing back pain and reducing any back pain you might have. However, if you have chronic back pain (back pain that has lasted more than three months), you should consult your GP before starting any exercise programme.
Exercises like walking or swimming strengthen the muscles that support your back without putting any strain on it, or subjecting it to a sudden jolt.
Activities like yoga or pilates can help improve the flexibility and the strength of your back muscles. It is important that you carry out these activities under the guidance of a properly qualified instructor.
There are also a number of simple exercises you can do in your own home to help prevent or relieve back pain:
- Wall slides – stand with your back against a wall with your feet shoulder-width apart. Slide down into a crouch so your knees are bent to about 90 degrees. Count to five and then slide back up the wall. Repeat five times.
- Leg raises – lie flat on your back on the floor. Lift each heel in turn just off the floor while keeping your legs straight. Repeat five times.
- Bottom lifts – lie flat on your back on the floor. Bend your knees so your feet are flat on the floor. Then lift your bottom in the air by tightening your stomach muscles while keeping your back straight. Repeat five times.
At first, you should do these exercises once or twice a day, and then gradually increase to doing them six times a day, as your back allows.
These exercises are also useful for ‘warming up’ your back. Many people injure their back when doing everyday chores at home or work, such as lifting, gardening, or using a vacuum cleaner. ‘Warming up’ your back before you start these chores can help prevent injury.
Lifting and handling
One of the biggest causes of a back injury, especially at work, is lifting or handling objects incorrectly. Learning and following the correct method for lifting and handling objects can help prevent back pain.
- Think before you lift – can you manage the lift? Are there any handling aids you can use? Where is the load going?
- Start in a good position – your feet should be apart with one leg slightly forward to maintain balance. When lifting, let your legs take the strain – bend your back, knees and hips slightly but don’t stoop or squat. Tighten your stomach muscles to pull your pelvis in. Don’t straighten your legs before lifting as you may strain your back on the way up.
- Keep the load close to your waist – keep the load as close to your body for as long as possible with the heaviest end nearest to you.
- Avoid twisting your back or leaning sideways – especially when your back is bent. Your shoulders should be level and facing in the same direction as your hips. Turning by moving your feet is better than lifting and twisting at the same time.
- Keep your head up – once your have the load secure, look ahead, not down at the load.
- Know your limits – there is a big difference between what you can lift and what you can safely lift. If in doubt, get help.
- Push, don’t pull – if you have to move a heavy object across the floor, it is better to push it rather than pull it.
- Distribute the weight evenly – if you are carrying shopping bags or luggage, try to distribute the weight evenly on both sides of your body.
Homeopathy Treatment for Back Pain
- Aesculus – Pain in the very low back (the sacral or sacroiliac areas) that feels worse when standing up from a sitting position, and worse from stooping, may be eased with this remedy. Aesculus is especially indicated for people with low back pain who also have a tendency toward venous congestion and hemorrhoids.
- Arnica montana – This remedy relieves lower back aches and stiffness from overexertion or minor trauma.
- Bryonia – This remedy is indicated when back pain is worse from even the slightest motion. Changing position, coughing, turning, or walking may bring on sharp, excruciating pain. This remedy can be helpful for back pain after injury and backaches during illness.
- Calcarea carbonica – This is often useful for low back pain and muscle weakness, especially in a person who is chilly, flabby or overweight, and easily tired by exertion. Chronic low back pain and muscle weakness may lead to inflammation and soreness that are aggravated by dampness and cold.
- Calcarea phosphorica – Stiffness and soreness of the spinal muscles and joints, especially in the neck and upper back, may be relieved by this remedy. The person feels worse from drafts and cold, as well as from exertion. Aching in the bones and feelings of weariness and dissatisfaction are often seen in people who need this remedy.
- Natrum muriaticum – Back pain that improves from lying on something hard or pressing a hard object (such as a block or book) against the painful area suggests a need for this remedy. The person often seems reserved or formal but has strong emotions that are kept from others. Back pain from suppressed emotions, especially hurt or anger may respond to Natrum muriaticum.
- Nux vomica – This remedy is indicated for muscle cramps or constricting pains in the back. Discomfort is made worse by cold and relieved by warmth. The pain usually is worse at night, and the person may have to sit up in bed to turn over. Backache is also worse during constipation, and the pain is aggravated when the person feels the urge to move the bowels.
- Rhus Toxicodendron – This remedy can be useful for pain in the neck and shoulders as well as the lower back, when the pain is worse on initial movement and improves with continued motion. Even though in pain, the person finds it hard to lie down or stay still for very long, and often restlessly paces about. Aching and stiffness are aggravated in cold damp weather and relieved by warm applications, baths or showers, and massage.
- Sulfur – This remedy is often indicated when a person with back pain has a slouching posture. The back is weak and the person feels much worse from standing up for any length of time. Pain is also worse from stooping. Warmth may aggravate the pain and inflammation.
Other Remedies
- Cimicifuga (also called Actaea racemosa) – Severe aching and stiffness in the upper back and neck, as well as the lower back—with pains that extend down the thighs or across the hips — may be eased with this remedy. It isoften helpful for back pain during menstrual periods, with cramping, heaviness, and soreness. A person who needs this remedy typically is talkative and energetic, becoming agitated or depressed when ill.
- Dulcamara – If back pain sets in during cold damp weather, along with catching a cold, or after getting wet and chilled, this remedy may be indicated. Stiffness and chills can be felt in the back, and pain is usually worse from stooping.
- Ignatia – Back pains related to emotional upsets—especially grief—will often respond to this remedy. The muscles of the lower back may spasm, and twitches, drawing pains, and cramps often occur in other areas.
- Kali carbonicum – Kali Carbonicum is a homeopathic medicine for lower back pain with the feeling that the knees are going to “give in.”
- Hypericum perforatum – This homeopathic remedy relieves lower back pain with sharp throbbing pain.
- Ruta graveolens – This is used to relieve lower back pain caused or worsened by staying immobile.
References