www.rxharun.com
Another Name of De Quervain Tendinitis
Tendinopathy – De Quervain tendinitis; de Quervain tenosynovitis
- A tendon is thick bendable tissue that connects muscle to bone. Two tendons run from the back of your thumb down the side of your wrist. De Quervain tendinitis is caused when these tendons are swollen and irritated.
Anatomy of De Quervain Tendinitis
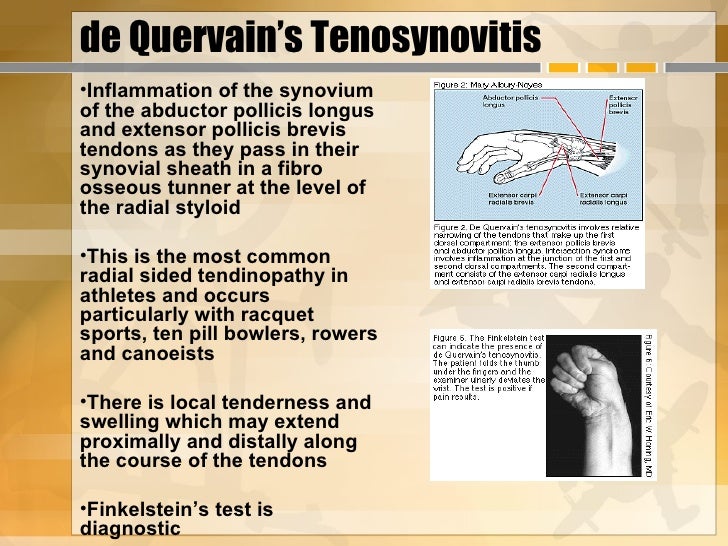
De Quervain’s tenosynovitis affects two thumb tendons. These tendons are called the abductor pollicis longus (APL) and the extensor pollicis brevis (EPB).
- Tendons connect muscle to bone. Muscles pull on tendons for movement. The muscles connected to the APL and EPB tendons are on the back of the forearm. The muscles angle toward the thumb.
- On their way to the thumb, the APL and EPB tendons travel side by side along the inside edge of the wrist. They pass through a tunnel near the end of the radiusbone of the forearm. The tunnel helps hold the tendons in place, like the guide on a fishing pole.
- This tunnel is lined with a slippery coating called tenosynovium. The tenosynovium is a slippery covering that allows the two tendons to glide easily back and forth as they move the thumb. Inflammation of the tenosynovium and tendon is called tenosynovitis. In de Quervain’s tenosynovitis, the inflammation constricts the movement of the tendons within the tunnel.
Causes of De Quervain Tendinitis
The cause of de Quervain’s tenosynovitis is idiopathic or unknown. However, there are certain risk factors that may increase your chance of developing the condition. These can include the following:
- Gender – The condition is more common in females than males.
- Age – It occurs more frequently around ages 30-50.
- Social Habits – The condition may be caused by overuse such as with frequent texting or typing on mobile devices with your thumbs.
- Work Habits – Occupations that require repetitive hand and wrist movements such as construction or playing music may increase your risk of developing the condition.
- Medical Conditions – Patients with diabetes, alcoholism, cirrhosis of the liver, and seizure disorders appear to be at increased risk of developing the condition.
Symptoms of De Quervain Tendinitis
- Pain may be felt over the thumb side of the wrist. This is the main symptoms. The pain may appear either gradually or suddenly. Pain is felt in the wrist and can travel up the forearm or down the thumb. The pain is usually worse when the hand and thumb are in use. This is especially true when forcefully grasping objects or twisting the wrist.
- Swelling may be seen over the thumb side of the wrist. This swelling may occur together with a fluid-filled cyst in this region.
- Pain and tenderness to the thumb base and wrist area near the thumb
- Swelling to the wrist area near the thumb
- The fluid-filled cyst may occur at the thumb base
- Pain may radiate up the arm
- Pain may occur gradually or suddenly
- Pain tends to increase with thumb movement
- Difficulty or inability to grip objects
- Impaired thumb function affecting daily activities
- A “catching” or “snapping” sensation may be felt when moving the thumb.
- Pain and swelling may make it difficult to move the thumb and wrist
Diagnosis of De Quervain Tendinitis
Plain Radiograph
Plain radiographs are non-diagnostic of the condition but may show non-specific signs and can help exclude other causes of pain such as fracture, carpometacarpal arthritis, and osteomyelitis. Signs include:
- Soft-tissue swelling over the radial styloid
- Focal abnormalities of the radial styloid including cortical erosion, sclerosis or periosteal reaction
Ultrasound
Ultrasound is very often diagnostic. Findings include
- Oedematous tendon thickening of APL and EPB at the level of radial styloid (compare with a contralateral side)
- Increased fluid within the first extensor tendon compartment tendon sheath
- Thickening of overlying retinaculum and the synovial sheath
- Peritendinous subcutaneous edema resulting in a hypoechoic halo sign
- Peritendinous subcutaneous hyperemia on Doppler imaging
It is important to assess for an intertendinous septum which can usually be identified if present. Ultrasound is often used to guide corticosteroid injections into the tendon compartment to treat the condition.
MRI
- MRI is very sensitive and specific and useful for detecting mild disease where ultrasound may be equivocal. Presence or absence of intertendinous septum can be assessed. Findings include :
Tenosynovitis
- Increased fluid within tendon sheath (high T2, low-intermediate T1)
- Bebris within sheath (intermediate T1 signal)
- Thickened oedematous retinaculum
- Peritendinous subcutaneous edema
- Peritendinous subcutaneous contrast enhancement
Tendinosis
- Tendon enlargement maximal at radial styloid and often greater at the medial aspect of the tendon
- Slightly increased intratendinous T1 and T2 signal compared to other tendons
- Striated appearance of tendons due to multiple enlarged slips
- Longitudinal tendon tear
- Linear high T2 signal due to the fluid within a split
- More common in all treatment
Treatment of De Quervain Tendinitis
Conservative Treatment Options
Your surgeon will recommend conservative treatment options to treat your condition if you are experiencing pain and are having difficulty using your hands for everyday activities. Treatment options will vary depending on the severity of the condition. Conservative treatment options may include the following
- Immobilization – Splints may be applied to rest the affected wrist and thumb and prevent movement until the condition heals.
- Ice – Applying ice to the affected area over a towel for 20 minutes 3-4xdaily may help with the pain and swelling.
- Medications – Non-steroidal anti-inflammatory medications (NSAID’s) may be prescribed to decrease the swelling and discomfort.
- Therapy – Physical therapy may be ordered to reduce the pain & inflammation
Medicine
- Analgesics – Prescription-strength drugs that relieve pain but not inflammation.
- Antidepressants – A Drugs that block pain messages from your brain and boost the effects of endorphins (your body’s natural painkillers).
- Medication – Common pain remedies such as aspirin, acetaminophen, ibuprofen, and naproxen can offer short-term relief. All are available in low doses without a prescription. Other medications, including muscle relaxants and anti-seizure medications, treat aspects such as muscle spasms and damaged nerves.
- Corticosteroid injections – Your doctor will inject a steroid such as prednisone into your thumb joints. Steroids make inflammation go down. However, because of side effects, they are used sparingly.
- Anesthetics – Used with precision, an injection of a “nerve block” can stop the pain for a time.
- Muscle Relaxants: These medications provide relief from spinal muscle spasms.
- Neuropathic Agents – Drugs(pregabalin & gabapentin) that address neuropathic—or nerve-related—pain. This includes burning, numbness, and tingling.
- Opioids – Also known as narcotics, these medications are intense pain relievers that should only be used under a doctor’s careful supervision.
- Topical Medications – These prescription-strength creams, gels, ointments, patches, and sprays help relieve pain and inflammation through the skin.
- Calcium & vitamin D3 – to improve bones health and healing fracture.
- Glucosamaine & diacerine – can be used to tightening the loose tenson and regenerate cartilage or inhabit the further degeneration of cartilage.
- Injections – Corticosteroids injections to the affected tendon sheath may be done to relieve local inflammation and pain
Surgery of De Quervain Tendinitis
If all else fails, you may need surgery. The goal of surgery is to give the tendons more space so they no longer rub on the inside of the tunnel. To do this, the surgeon performs a surgical release of the roof of the tunnel.
- This surgery can usually be done on an outpatient basis, which means that you won’t have to spend the night in the hospital. It can be done using a general anesthetic, which puts you to sleep, or a regional anesthetic. A regional anesthetic blocks the nerves going to only a certain part of the body. Injection of medications similar to novocaine can block the nerves for several hours.
- In surgery for de Quervain’s tenosynovitis – you may get an axillary block, which puts the arm to sleep, or a wrist block, which puts only the hand to sleep. It is even possible to perform the surgery by simply injecting novocaine around the area of the incision.
- Once you have anesthesia – your surgeon will make sure the skin of your forearm and wrist is free of infection by cleaning the skin with a germ-killing solution. The first step in the surgical release is to make a small incision along the thumb side of the wrist.
- The surgeon moves aside other tissues and locates the tendons and the tunnel. An incision is made to split the roof, or top, of the tunnel. This allows the tunnel to open up, creating more space for the tendons. The tunnel will eventually heal closed, but it will be larger than before. Scar tissue will fill the gap where the tunnel was cut.
The skin is then stitched together, and your hand is wrapped in a bulky dressing.
Post-Operative Care of De Quervain Tendinitis
After surgery, your surgeon will give you guidelines to follow. Common post-operative guidelines include:
- Keep the surgical incision clean and dry. Cover the area with plastic wrap when bathing or showering.
- Ice packs to the surgical area may be used to reduce pain and swelling.
- The bandage is usually removed after a couple days.
- Your surgeon may recommend occupational therapy for strengthening exercises and measures to prevent recurrence.
- Eating a healthy diet and not smoking will promote healing.
Risks and Complications
As with any major surgery, there are potential risks involved. The majority of patients suffer no complications following tendon release surgery; however, complications can occur and include:
- Complications from nerve blocks such as infection or nerve damage
- Serious medical problems can lead to ongoing health concerns, prolonged hospitalization, or rarely death.
- Infection
- Nerve damage causing weakness, paralysis, or loss of feeling in the hand area.
- Injury to the arteries of the fingers/hand
- Cond–ition recurs
After Surgery of De Quervain Tendinitis
Rehabilitation is more involved after surgery. Full recovery could take several months. Pain and symptoms generally begin to improve after surgery, but you may have tenderness in the area of the incision for several months.
- Take time during the day to support your arm with your hand elevated above the level of your heart. You should move your fingers and thumb occasionally during the day. Keep the dressing on your hand until you return to the surgeon. Avoid getting the stitches wet. Your stitches will be removed 10 to 14 days after surgery.
- You will probably need to attend occupational or physical therapy sessions for six to eight weeks. You’ll begin doing active hand movements and range-of-motion exercises. Therapists also use ice packs, soft-tissue massage, and hands-on stretching to help with the range of motion. When the stitches are removed, you may start carefully strengthening your hand and thumb by squeezing and stretching putty. Therapists also use a series of gentle stretches to encourage the thumb tendons to glide easily within the tunnel.
- As you progress, your therapist will give you exercises to help strengthen and stabilize the muscles and joints in the hand and thumb. Other exercises are used to improve fine motor control and dexterity. Some of the exercises you’ll do are designed to get your hand working in ways that are similar to your work tasks and sports activities.
- Your therapist will help you find ways to do your tasks that don’t put too much stress on your thumb and wrist. Before your therapy sessions end, your therapist will teach you a number of ways to avoid future problems.
References


