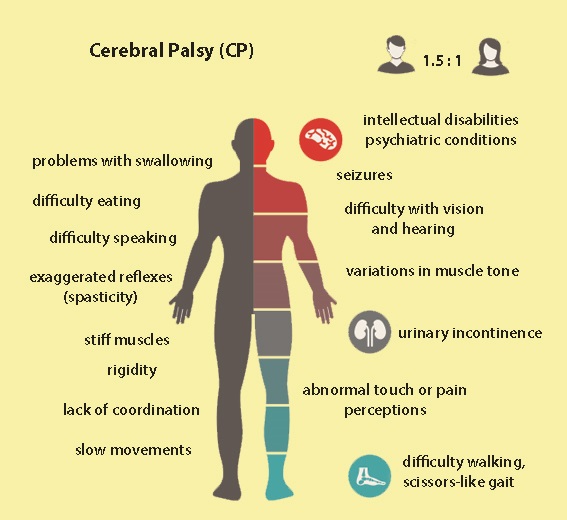
Cerebral Palsy is a group of neurological non-progressive/ permanent movement disorders that appear in early childhood or before, during or after birth due to brain injury or abnormal development of the brain or injury of brain & central nervous system. Often, symptoms include poor coordination, stiff muscles, weak muscles, and tremors and maybe the problems with sensation, vision, hearing, swallowing, and speaking.
Cerebral palsy is a broad range of static, non-progressive motor disabilities that present from birth or early childhood as a result of injury to neuromotor components of the central nervous system. Motor performance is normally coordinated via communication between the cerebral cortex, thalamus, basal ganglia, brain stem, cerebellum, spinal cord, and communicating sensory-motor pathways. This complex network lends itself to injury at many different levels. Etiologies are numerous and can occur during the prenatal, perinatal, and postnatal periods. The severity of the neurologic deficit and the clinical manifestations are varied depending on the time, location and nature of the original injury. In order to approach cerebral palsy systematically, the primary health care practitioner must be prepared to recognize neuromotor deficits, diagnose and classify the type of disorder, and implement a methodical treatment plan. The purpose of this article is to review the etiology, pathophysiology, diagnostic classification (Swedish system), clinical manifestations, and therapeutic management of cerebral palsy and prepare the advanced practice nurse to care for the individual and family.
Types of Cerebral Palsy
Geographical classification of cerebral palsy.
| Major types | Description |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Physiological classification of cerebral palsy
| Major types | Description |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Physiologically, cerebral palsy can be divided into a spastic type, which affects the corticospinal (pyramidal) tracts, and an extrapyramidal type, which affects the other regions of the developing brain. The extrapyramidal types of cerebral palsy include athetoid, choreiform, ataxia, rigid, and hypotonic.
GMFC system of cerebral palsy and approximate percentage in each group.
|
|
|
|
|
|
|
|
|
|
The Topography of Cerebral Palsy
European classification of (motor impairment in) cerebral palsy[rx]
The severity of cerebral palsy: gross motor function classification system (for children between 6 and 12 years)[rx]
www.rxharun.com
The specific forms of cerebral palsy are determined by the extent, type, and location of a child’s abnormalities. Doctors classify CP according to the type of movement disorder involved — spastic (stiff muscles), athetoid (writhing movements), or ataxic (poor balance and coordination) — plus any additional symptoms, such weakness (paresis) or paralysis (plegia). For example, hemiparesis (hemi = half) indicates that only one side of the body is weakened.Quadriplegia (quad = four) means all four limbs are afffected.
Spastic cerebral palsy – is the most common type of the disorder. People have stiff muscles and awkward movements. Forms of spastic cerebral palsy include:
- Spastic hemiplegia/hemiparesis – typically affects the arm and hand on one side of the body, but it can also include the leg. Children with spastic hemiplegia generally walk later and on tip-toe because of tight heel tendons. The arm and leg of the affected side are frequently shorter and thinner. Some children will develop an abnormal curvature of the spine (scoliosis). A child with spastic hemiplegia may also have seizures. Speech will be delayed and, at best, may be competent, but intelligence is usually normal.
- Spastic diplegia/diparesis – involves muscle stiffness that is predominantly in the legs and less severely affects the arms and face, although the hands may be clumsy. Tendon reflexes in the legs are hyperactive. Toes point up when the bottom of the foot is stimulated. Tightness in certain leg muscles makes the legs move like the arms of a scissor. Children may require a walker or leg braces. Intelligence and language skills are usually normal.
- Spastic quadriplegia/quadriparesis – is the most severe form of cerebral palsy and is often associated with moderate-to-severe intellectual disability. It is caused by widespread damage to the brain or significant brain malformations. Children will often have severe stiffness in their limbs but a floppy neck. They are rarely able to walk. Speaking and being understood are difficult. Seizures can be frequent and hard to control.
- Dyskinetic cerebral palsy (also includes athetoid, choreoathetoid, and dystonic cerebral palsies) – is characterized by slow and uncontrollable writhing or jerky movements of the hands, feet, arms, or legs. Hyperactivity in the muscles of the face and tongue makes some children grimace or drool. They find it difficult to sit straight or walk. Some children have problems hearing, controlling their breathing, and/or coordinating the muscle movements required for speaking. Intelligence is rarely affected in these forms of cerebral palsy.
- Athetoid – Athetoid cerebral palsy or dyskinetic cerebral palsy (sometimes abbreviated ADCP) is primarily associated with damage to the basal ganglia in the form of lesions that occur during brain development due to bilirubin encephalopathy and hypoxic-ischemic brain injury. ADCP is characterized by both hypertonia and hypotonia, due to the affected individual’s inability to control muscle tone. Clinical diagnosis of ADCP typically occurs within 18 months of birth and is primarily based on motor function and neuroimaging techniques. Athetoid dyskinetic cerebral palsy is a non-spastic, extrapyramidal form of cerebral palsy. Dyskinetic cerebral palsy can be divided into two different groups; choreoathetoid and dystonic. Choreoathetotic CP is characterized by involuntary movements most predominantly found in the face and extremities. Dystonic ADCP is characterized by slow, strong contractions, which may occur locally or encompass the whole body.
- Ataxic cerebral palsy – affects balance and depth perception. Children with ataxic CP will often have poor coordination and walk unsteadily with a wide-based gait. They have difficulty with quick or precise movements, such as writing or buttoning a shirt, or a hard time controlling voluntary movement such as reaching for a book.
- Mixed types – of cerebral palsy refer to symptoms that don’t correspond to any single type of CP but are a mix of types. For example, a child with mixed CP may have some muscles that are too tight and others that are too relaxed, creating a mix of stiffness and floppiness.
Causes of Cerebral Palsy
Muscle control takes place in a part of the brain called the cerebrum. The cerebrum is the upper part of the brain. Damage to the cerebrum before, during, or within 5 years of birth can cause cerebral palsy.
- The cerebrum is also responsible for memory, ability to learn, and communication skills. This is why some people with cerebral palsy have problems with communication and learning. Cerebrum damage can sometimes affect vision and hearing.
- Some newborns are deprived of oxygen during labor and delivery. In the past, it was thought that this lack of oxygen during birth led to the brain damage.
- However, during the 1980s, research showed that fewer than 1 in 10 cases of cerebral palsy stem from oxygen deprivation during birth. Most often, the damage occurs before birth, probably during the first 6 months of pregnancy.
There are at least three possible reasons for this.
Periventricular leukomalacia (PVL)
- PVL is a kind of damage that affects the brain’s white matter because of a lack of oxygen in the womb. It may occur if the mother has an infection during pregnancy, such as rubella or German measles, low blood pressure, preterm delivery, or if she uses an illegal drug.
Abnormal development of the brain
- Disruption of brain development can affect the way the brain communicates with the body’s muscles and other functions. During the first 6 months of pregnancy, the brain of the embryo or fetus is particularly vulnerable. Damage can stem from mutations in the genes responsible for brain development, certain infections such as toxoplasmosis, a parasite infection, herpes and herpes-like viruses, and head trauma.
Intracranial hemorrhage
- Sometimes, bleeding inside the brain happens when a fetus experiences a stroke. Bleeding in the brain can stop the supply of blood to vital brain tissue, and this tissue can become damaged or die. The escaped blood can clot and damage surrounding tissue.
Several factors can cause a stroke in a fetus during pregnancy
- A blood clot in the placenta that blocks the flow of blood
- A clotting disorder in the fetus
- Interruptions in arterial blood flow to the fetal brain
- Untreated pre-eclampsia in the mother
- Inflammation of the placenta
- Pelvic inflammatory infection in the mother
During delivery, the risk is increased by the following factors:
- Emergency cesarean
- The second stage of labor is prolonged
- Vacuum extraction is used during delivery
- Fetal or neonatal heart anomalies
- Umbilical cord abnormalities
Anything that increases the risk of preterm birth or low birth weight also raises the risk of cerebral palsy.
Factors that may contribute to a higher risk of cerebral palsy include:
- Multiple births, for example, twins
- Damaged placenta
- Sexually transmitted infections (STIs)
- Consumption of alcohol, illegal drugs, or toxic substances during pregnancy
- Malnourishment during pregnancy
- Random malformation of the fetal brain
- Small pelvis in the mother
- Breech delivery
Brain damage after birth
- A small proportion of cases happen because of damage after birth. This can happen because of an infection such as meningitis, a head injury, a drowning accident, or poisoning.
- When damage occurs, it will do so soon after the birth. With age, the human brain becomes more resilient and able withstand more damage.
Symptoms of Cerebral Palsy
www.rxharun.com
Signs and symptoms can vary greatly. Movement and coordination problems associated with cerebral palsy may include:
- Variations in muscle tone, such as being either too stiff or too floppy
- Stiff muscles and exaggerated reflexes (spasticity)
- Stiff muscles with normal reflexes (rigidity)
- Lack of muscle coordination (ataxia)
- Tremors or involuntary movements
- Slow, writhing movements (athetosis)
- Delays in reaching motor skills milestones, such as pushing up on arms, sitting up alone or crawling
- Favoring one side of the body, such as reaching with only one hand or dragging a leg while crawling
- Difficulty walking, such as walking on toes, a crouched gait, a scissors-like gait with knees crossing, a wide gait or an asymmetrical gait
- Excessive drooling or problems with swallowing
- Difficulty with sucking or eating
- Delays in speech development or difficulty speaking
- Difficulty with precise motions, such as picking up a crayon or spoon
- Seizures
The disability associated with cerebral palsy may be limited primarily to one limb or one side of the body, or it may affect the whole body. The brain disorder causing cerebral palsy doesn’t change with time, so the symptoms usually don’t worsen with age. However, muscle shortening and muscle rigidity may worsen if not treated aggressively.
Brain abnormalities associated with cerebral palsy also may contribute to other neurological problems. People with cerebral palsy may also have:
- Difficulty with vision and hearing
- Intellectual disabilities
- Seizures
- Abnormal touch or pain perceptions
- Oral diseases
- Mental health (psychiatric) conditions
- Urinary incontinence
Treatment of Cerebral Palsy
- Cerebral palsy can’t be cured – but treatment will often improve a child’s capabilities. Many children go on to enjoy near-normal adult lives if their disabilities are properly managed. In general, the earlier treatment begins, the better chance children have of overcoming developmental disabilities or learning new ways to accomplish the tasks that challenge them.
- There is no standard therapy – that works for every individual with cerebral palsy. Once the diagnosis is made, and the type of CP is determined, a team of health care professionals will work with a child and his or her parents to identify specific impairments and needs, and then develop an appropriate plan to tackle the core disabilities that affect the child’s quality of life.
- Occupational therapy – focuses on optimizing upper body function, improving posture, and making the most of a child’s mobility. Occupational therapists help individuals address new ways to meet everyday activities such as dressing, going to school, and participating in day-to-day activities.
- Recreation therapy – encourages participation in art and cultural programs, sports, and other events that help an individual expand physical and cognitive skills and abilities. Parents of children who participate in recreational therapies usually notice an improvement in their child’s speech, self-esteem, and emotional well-being.
- Speech and language therapy – can improve a child’s ability to speak, more clearly, help with swallowing disorders, and learn new ways to communicate—using sign language and/or special communication devices such as a computer with a voice synthesizer, or a special board covered with symbols of everyday objects and activities to which a child can point to indicate his or her wishes.
- Treatments for problems with eating and drooling – are often necessary when children with CP have difficulty eating and drinking because they have little control over the muscles that move their mouth, jaw, and tongue. They are also at risk for breathing food or fluid into the lungs, as well as for malnutrition, recurrent lung infections, and progressive lung disease.
Therapies used to manage spasticity in cerebral palsy
|
studies (patients studied) | randomized trials ( patients randomized) | Conclusions |
|---|---|---|---|
|
3 (52) | 3 (52) | no strong controlled evidence found to support or refute the use of Botulinum toxin type A for the treatment of leg spasticity (1) |
|
Not provided | 4 (183) | Botulinum toxin type A superior to placebo for improvement of gait (2) |
|
2 (44) | 2 (44) | one of the two randomized trials reported promising results in support of reduced muscle tone following Botulinum toxin A injections; evidence not sufficient to support or refute the use of this therapy as an adjunct to managing the upper limb in children with spastic cerebral palsy (3) |
|
3 (90) | 3 (90) | selective’ dorsal rhizotomy (SDR) plus physiotherapy reduces spasticity in children with spastic diplegia slightly improves gross motor function (4) |
|
21 (473) | 9 (238) | No randomized trials available comparing protocols of casting in current use with no treatment; no strong and consistent evidence that combining casting and Botulinum toxin A is superior to using either intervention along; no evidence that the order of these two treatments affects the outcome (5) |
- Ade-Hall RA, Moore AP. Cochrane Collaboration. 2000.
- Cardoso ES, Rodrigues BM, Barroso M, Menezes CJ, Lucena RS, Nora DB et al. Ped Neurol 2006; 34:106-109.
- Wasiak J, Hoare B, Wallen M. Cochrane Collaboration . 2004.
- McLaughlin J, Bjornson K, Temkin N, Steinbok P, Wright V, Reiner A et al. Dev Med Child Neurol 2002; 44:17-25.
- Blackmore AM, Boettcher-Hunt E, Jordan M, Chan MDY. Dev Med Child Neurol 2007; 49:781-790.
|
studies (patients studied) | randomized trials (patients randomized) | Conclusions |
|---|---|---|---|
|
11 (46) | 1 (20) | trend towards improved communication skills; evidence not sufficient to recommend change in practice (1) |
|
3 (94) | 2 (49) | a significant benefit in a single trial; positive trend favoring constraint-induced movement therapy (CIMT) and Forced Use; “given the limited evidence, the use of CIMT, modified CIMT and Forced Use should be considered experimental in children with hemiplegic cerebral palsy.” (2) |
|
6 (449) | 2 (137) | Hyperbaric oxygen therapy and pressurized room air improved function to a similar degree; a proportion of patients treated with these therapy experience seizures (3) |
- Pennington L, Goldbart J, Marshall J. Cochrane Collaboration. 2003.
- Hoare BJ, Wasiak J, Imms C, Carey L. Cochrane Collaboration. 2007.
- Ade-Hall RA, Moore AP. Cochrane Collaboration. 2000. McDonagh MS, Morgan D, Carson S, Russman BS. Dev Med Child Neurol 2007; 49:942-947.
Drug Treatments
Nonoperative modalities, such as medication, splinting and bracing, and physical therapy, are commonly used as primary treatment or in conjunction with other forms of treatment such as surgery.[rx]–[rx]
Oral medications such as
- Diazepam,
- Baclofen
- Tolperisone and Eperisone to relax muscle to increase muscle tone
- Phenobarbiton
- Gabapentin/pregabalin to inhabit the pain receptor in the brain.
- Mecobalamin /vitamin B12 to regenerate the myeline sheet in the nervous system.
- Steroid to suppressive the brain inflamation.
- Clonazipam drop to control over salivation & proper sleep.
- Dizanidine – are usually used as the first line of treatment to relax stiff, contracted, or overactive muscles. Some drugs have some risk side effects such as drowsiness, changes in blood pressure, and risk of liver damage that require continuous monitoring. Oral medications are most appropriate for children who need an only mild reduction in muscle tone or who have widespread spasticity.
- Botulinum toxin (BT-A) – injected locally, has become a standard treatment for overactive muscles in children with spastic movement disorders such as CP. BT-A relaxes contracted muscles by keeping nerve cells from over-activating muscle. The relaxing effect of a BT-A injection lasts approximately 3 months. Undesirable side effects are mild and short-lived, consisting of pain upon injection and occasionally mild flu-like symptoms. BT-A injections are most effective when followed by a stretching program including physical therapy and splinting. BT-A injections work best for children who have some control over their motor movements and have a limited number of muscles to treat, none of which is fixed or rigid.
- Intrathecal baclofen- therapy uses an implantable pump to deliver baclofen, a muscle relaxant, into the fluid surrounding the spinal cord. Baclofen decreases the excitability of nerve cells in the spinal cord, which then reduces muscle spasticity throughout the body. The pump can be adjusted if muscle tone is worse at certain times of the day or night. The baclofen pump is most appropriate for individuals with chronic, severe stiffness or uncontrolled muscle movement throughout the body
- Dantrolene – a peripheral acting drug, acts at the level of skeletal muscle and selectively decreases abnormal muscle stretch reflexes and tone. Dantrolene is used less frequently than other medications because some patients taking it to develop profound weakness, and there is a risk of hepatotoxicity with its long-term use.
Surgery
- Orthopedic surgery – is often recommended when spasticity and stiffness are severe enough to make walking and moving about difficult or painful. For many people with CP, improving the appearance of how they walk – their gait – is also important. Surgeons can lengthen muscles and tendons that are proportionately too short, which can improve mobility and lessen pain. Tendon surgery may help the symptoms for some children with CP but could also have negative long-term consequences. Orthopedic surgeries may be staggered at times appropriate to a child’s age and level of motor development. Surgery can also correct or greatly improve spinal deformities in people with CP. Surgery may not be indicated for all gait abnormalities and the surgeon may request a quantitative gait analysis before surgery.
- Surgery to cut nerves – Selective dorsal rhizotomy (SDR) is a surgical procedure recommended for cases of severe spasticity when all of the more conservative treatments – physical therapy, oral medications, and intrathecal baclofen — have failed to reduce spasticity or chronic pain. A surgeon locates and selectively severs overactivated nerves at the base of the spinal column. SDR is most commonly used to relax muscles and decrease chronic pain in one or both of the lower or upper limbs. It is also sometimes used to correct an overactive bladder. Potential side effects include sensory loss, numbness, or uncomfortable sensations in limb areas once supplied by the severed nerve.
Assistive devices
- Assistive devices such devices as computers, computer software, voice synthesizers, and picture books can greatly help some individuals with CP improve communications skills. Other devices around the home or workplace make it easier for people with CP to adapt to activities of daily living.
- Orthotic devices help to compensate for muscle imbalance and increase independent mobility. Braces and splints use external force to correct muscle abnormalities and improve function such as sitting or walking. Other orthotics help stretch muscles or the positioning of a joint. Braces, wedges, special chairs, and other devices can help people sit more comfortably and make it easier to perform daily functions. Wheelchairs, rolling walkers, and powered scooters can help individuals who are not independently mobile. Vision aids include glasses, magnifiers, and large-print books and computer typeface. Some individuals with CP may need surgery to correct vision problems. Hearing aids and telephone amplifiers may help people hear more clearly.
Complementary and Alternative Therapies
- Many children and adolescents with CP use some form of complementary or alternative medicine. Controlled clinical trials involving some of the therapies have been inconclusive or showed no benefit and the therapies have not been accepted in mainstream clinical practice.
- Although there are anecdotal reports of some benefit in some children with CP, these therapies have not been approved by the U.S. Food and Drug Administration for the treatment of CP.
- Such therapies include hyperbaric oxygen therapy, special clothing worn during resistance exercise training, certain forms of electrical stimulation, assisting children in completing certain motions several times a day, and specialized learning strategies. Also, dietary supplements, including herbal products, may interact with other products or medications a child with CP may be taking or have unwanted side effects on their own. Families of children with CP should discuss all therapies with their doctor.
- Stem cell therapy – is being investigated as a treatment for cerebral palsy, but research is in early stages and large-scale clinical trials are needed to learn if stem cell therapy is safe and effective in humans. Stem cells are capable of becoming other cell types in the body. Scientists are hopeful that stem cells may be able to repair damaged nerves and brain tissues. Studies in the U.S. are examining the safety and tolerability of umbilical cord blood stem cell infusion in children with CP.
Risk factors
A number of factors are associated with an increased risk of cerebral palsy.
- Maternal health – Certain infections or health problems during pregnancy can significantly increase cerebral palsy risk to the baby. Infections of particular concern include:
- German measles (rubella) – Rubella is a viral infection that can cause serious birth defects. It can be prevented with a vaccine.
- Chickenpox (varicella) – Chickenpox is a contagious viral infection that causes itching and rashes, and it can cause pregnancy complications. It too can be prevented with a vaccine.
- Cytomegalovirus – Cytomegalovirus is a common virus that causes flu-like symptoms and may lead to birth defects if a mother experiences her first active infection during pregnancy.
- Herpes – Herpes infection can be passed from mother to child during pregnancy, affecting the womb and placenta. Inflammation triggered by infection may then damage the unborn baby’s developing nervous system.
- Toxoplasmosis – Toxoplasmosis is an infection caused by a parasite found in contaminated food, soil and the feces of infected cats.
- Syphilis – Syphilis is a sexually transmitted bacterial infection.
- Exposure to toxins – Exposure to toxins, such as methyl mercury, can increase the risk of birth defects.
- Zika virus infection – Infants for whom maternal Zika infection causes microcephaly can develop cerebral palsy.
- Other conditions. Other conditions may increase the risk of cerebral palsy, such as thyroid problems, intellectual disabilities or seizures.
Infant illness
Illnesses in a newborn baby that can greatly increase the risk of cerebral palsy include:
- Bacterial meningitis –This bacterial infection causes inflammation in the membranes surrounding the brain and spinal cord.
- Viral encephalitis – This viral infection similarly causes inflammation in the membranes surrounding the brain and spinal cord.
- Severe or untreated jaundice – Jaundice appears as a yellowing of the skin. The condition occurs when certain byproducts of “used” blood cells aren’t filtered from the bloodstream.
Other factors of pregnancy and birth
While the potential contribution from each is limited, additional pregnancy or birth factors associated with increased cerebral palsy risk include:
- Breech births – Babies with cerebral palsy are more likely to be in a feet-first position (breech presentation) at the beginning of labor rather than headfirst.
- Complicated labor and delivery – Babies who exhibit vascular or respiratory problems during labor and delivery may have existing brain damage or abnormalities.
- Low birth weight – Babies who weigh less than 5.5 pounds (2.5 kilograms) are at higher risk of developing cerebral palsy. This risk increases as birth weight drops.
- Multiple babies – Cerebral palsy risk increases with the number of babies sharing the uterus. If one or more of the babies die, the chance that the survivors may have cerebral palsy increases.
- Premature birth – A normal pregnancy lasts 40 weeks. Babies born fewer than 37 weeks into the pregnancy are at higher risk of cerebral palsy. The earlier a baby is born, the greater the cerebral palsy risk.
- Rh blood type incompatibility between mother and child – If a mother’s Rh blood type doesn’t match her baby’s, her immune system may not tolerate the developing baby’s blood type and her body may begin to produce antibodies to attack and kill her baby’s blood cells, which can cause brain damage.
Complications
Muscle weakness, muscle spasticity and coordination problems can contribute to a number of complications either during childhood or later during adulthood, including:
- Contracture – Contracture is muscle tissue shortening due to severe muscle tightening (spasticity). Contracture can inhibit bone growth, cause bones to bend, and result in joint deformities, dislocation or partial dislocation.
- Malnutrition – Swallowing or feeding problems can make it difficult for someone who has cerebral palsy, particularly an infant, to get enough nutrition. This may cause impaired growth and weaker bones. Some children may need a feeding tube for adequate nutrition.
- Mental health conditions – People with cerebral palsy may have mental health (psychiatric) conditions, such as depression. Social isolation and the challenges of coping with disabilities can contribute to depression.
- Lung disease – People with cerebral palsy may develop lung disease and breathing disorders.
- Neurological conditions – People with cerebral palsy may be more likely to develop movement disorders or worsened neurological symptoms over time.
- Osteoarthritis – Pressure on joints or abnormal alignment of joints from muscle spasticity may lead to the early onset of painful degenerative bone disease (osteoarthritis).
- Osteopenia – Fractures due to low bone density (osteopenia) can stem from several common factors such as lack of mobility, nutritional shortcomings and antiepileptic drug use.
- Eye muscle imbalance – This can affect visual fixation and tracking; an eye specialist should evaluate suspected imbalances.
- Low birthweight and premature birth – Premature babies (born less than 37 weeks into pregnancy) and babies weighing less than 5 ½ pounds at birth have a much higher risk of developing cerebral palsy than full-term, heavier weight babies. Tiny babies born at very early gestational ages are especially at risk.
- Multiple births – Twins, triplets, and other multiple births — even those born at term — are linked to an increased risk of cerebral palsy. The death of a baby’s twin or triplet further increases the risk.
- Infections during pregnancy – Infections such as toxoplasmosis, rubella (German measles), cytomegalovirus, and herpes, can infect the womb and placenta. Inflammation triggered by infection may then go on to damage the developing nervous system in an unborn baby. Maternal fever during pregnancy or delivery can also set off this kind of inflammatory response.
- Blood type incompatibility between mother and child – Rh incompatibility is a condition that develops when a mother’s Rh blood type (either positive or negative) is different from the blood type of her baby. The mother’s system doesn’t tolerate the baby’s different blood type and her body will begin to make antibodies that will attack and kill her baby’s blood cells, which can cause brain damage.
- Exposure to toxic substances – Mothers who have been exposed to toxic substances during pregnancy, such as methyl mercury, are at a heightened risk of having a baby with cerebral palsy.
- Mothers with thyroid abnormalities, intellectual disability, excess protein in the urine, or seizures – Mothers with any of these conditions are slightly more likely to have a child with CP. There are also medical conditions during labor and delivery, and immediately after delivery that act as warning signs for an increased risk of CP. However, most of these children will not develop CP. Warning signs include:
- Breech presentation – Babies with cerebral palsy are more likely to be in a breech position (feet first) instead of head first at the beginning of labor. Babies who are unusually floppy as fetuses are more likely to be born in the breech position.
- Complicated labor and delivery – A baby who has vascular or respiratory problems during labor and delivery may already have suffered brain damage or abnormalities.
- Small for gestational age – Babies born smaller than normal for their gestational age are at risk for cerebral palsy because of factors that kept them from growing naturally in the womb.
- Low Apgar score – The Apgar score is a numbered rating that reflects a newborn’s physical health. Doctors periodically score a baby’s heart rate, breathing, muscle tone, reflexes, and skin color during the first minutes after birth. A low score at 10-20 minutes after delivery is often considered an important sign of potential problems such as CP.
- Jaundice – More than 50 percent of newborns develop jaundice (a yellowing of the skin or whites of the eyes) after birth when bilirubin, a substance normally found in bile, builds up faster than their livers can break it down and pass it from the body. Severe, untreated jaundice can kill brain cells and can cause deafness and CP.
Are there treatments for other conditions associated with cerebral palsy?
Epilepsy
- Many children with intellectual disability and CP also have epilepsy. In general, drugs are prescribed based on the type of seizures an individual experiences, since no one drug controls all types. Some individuals may need a combination of two or more drugs to achieve good seizure control.
Incontinence
- Medical treatments for incontinence include special exercises, biofeedback, prescription drugs, surgery, or surgically implanted devices to replace or aid muscles.
Osteopenia
- Children with CP who are unable to walk risk developing poor bone density (osteopenia), which makes them more likely to break bones. In a study of older Americans funded by the National Institutes of Health (NIH), a family of drugs called bisphosphonates, which has been approved by the FDA to treat mineral loss in elderly patients, also appeared to increase bone mineral density Doctors may choose to selectively prescribe the drug off-label to children to prevent osteopenia.
Pain
- Pain can be a problem for people with CP due to spastic muscles and the stress and strain on parts of the body that are compensating for muscle abnormalities. Some individuals may also have frequent and irregular muscle spasms that can’t be predicted or medicated in advance.
- Diazepam can reduce the pain associated with muscle spasms and gabapentin has been used successfully to decrease the severity and frequency of painful spasms. Botulinum toxin injections have also been shown to decrease spasticity and pain.
- Intrathecal baclofen has shown good results in reducing pain. Some children and adults have been able to decrease pain by using noninvasive and drug-free interventions such as distraction, relaxation training, biofeedback, and therapeutic massage.
Premature aging
- The majority of individuals with CP will experience some form of premature aging by the time they reach their 40s because of the extra stress and strain the disease puts upon their bodies.
- The developmental delays that often accompany CP keep some organ systems from developing to their full capacity and level of performance. As a consequence, organ systems such as the cardiovascular system (the heart, veins, and arteries) and pulmonary system (lungs) have to work harder and they age prematurely.
Functional issues at work
- The day-to-day challenges of the workplace are likely to increase as an employed individual with CP reaches middle age. Some individuals will be able to continue working with accommodations such as an adjusted work schedule, assistive equipment, or frequent rest periods.
Depression
- Mental health issues can also be of concern as someone with cerebral palsy grows older. The rate of depression is three to four times higher in people with disabilities such as cerebral palsy.
- It appears to be related not so much to the severity of their disabilities, but to how well they cope with them. The amount of emotional support someone has, how successful they are at coping with disappointment and stress, and whether or not they have an optimistic outlook about the future all have a significant impact on mental health.
Post-impairment syndrome
- This syndrome is marked by a combination of pain, fatigue, and weakness due to muscle abnormalities, bone deformities, overuse syndromes (sometimes also called repetitive motion injuries), and arthritis. Fatigue is often a challenge, since individuals with CP may use up to three to five times the amount of energy that able-bodied people use when they walk and move about.
Osteoarthritis and degenerative arthritis
- Musculoskeletal abnormalities that may not produce discomfort during childhood can cause pain in adulthood. For example, the abnormal relationships between joint surfaces and excessive joint compression can lead to the early development of painful osteoarthritis and degenerative arthritis.
- Individuals with CP also may have limited strength and restricted patterns of movement, which puts them at risk for overuse syndromes and nerve entrapments.
Other medical conditions
- Adults have higher than normal rates of other medical conditions secondary to their cerebral palsy, such as hypertension, incontinence, bladder dysfunction, and swallowing difficulties.
- Scoliosis is likely to progress after puberty, when bones have matured into their final shape and size. People with CP also have a higher incidence of bone fractures, occurring most frequently during physical therapy sessions.
- Genetic defects are sometimes responsible for the brain malformations and abnormalities that cause cerebral palsy. Scientists are searching for the genes responsible for these abnormalities by collecting DNA samples from people with cerebral palsy and their families and using genetic screening techniques to discover linkages between individual genes and specific types of abnormality – primarily those associated with the process in the developing brain in which neurons migrate from where they are born to where they settle into neural circuits (called neural migration).
- Scientists are scrutinizing events in newborn babies’ brains, such as bleeding, epileptic seizures, and breathing and circulation problems, which can cause the abnormal release of chemicals that triggers the kind of damage that causes cerebral palsy. For example, research has shown that bleeding in the brain unleashes dangerously high amounts of glutamate, a chemical that helps neurons communicate. However, too much glutamate overexcites and kills neurons. By learning how brain chemicals that are normally helpful become dangerously toxic, scientists will have opportunities to develop new drugs to block their harmful effects.
- Researchers are using imaging techniques and neurobehavioral tests to predict those preterm infants who will develop cerebral palsy. If these screening techniques are successful, doctors will be able to identify infants at risk for cerebral palsy before they are born.
- Periventricular white matter damage—the most common cause of CP—is characterized by death of the white matter around the fluid-filled ventricles in the brain. The periventricular area contains nerve fibers that carry messages from the brain to the body’s muscles. NINDS-sponsored researchers are hoping to develop preventative strategies for white matter damage. For example, researchers are examining the role the brain chemicals play on white matter development in the brain.
NIH-funded scientists continue to look at new therapies and novel ways to use existing options to treat individuals with CP, including:
- Constraint-induced therapy (CIT) – is a promising therapy for CP. CIT typically involves restraining the stronger limb (such as the “good” arm in a person who has been affected by a stroke on one side of the body) in a cast and forcing the weaker arm to perform intensive activities every day over a period of weeks. A clinical study sponsored by the NICHD is examining the use of different dosage levels of daily training using either full-time cast immobilization vs. part-time splint restraint in improving upper body extremity skills in children with weakness on both sides of their body. Study findings will establish evidence-based practice standards to improve lifelong neuromotor capacity in individuals with CP.
- Functional electrical stimulation (FES)—the therapeutic use of low-level electrical current to stimulate muscle movement and restore useful movements such as standing or stepping—is an effective way to target and strengthen spastic muscles. Researchers are evaluating how FES-assisted stationary cycling can improve physical conditioning and general lower extremity muscle strength in adolescents.
- Robotic therapy – that applies controlled force to the leg during the swing phase of gait is may improve the efficacy of body weight supported treadmill training in children with CP. The results from this NICHD study will lead to an innovative clinical therapy aimed at improving locomotor function in children with CP.
- Botulinum toxin (Botox) – injected locally, has become a standard treatment in children with spastic movement disorders such as CP. Recent animal studies suggest Botox degrades bone but there are no studies of its skeletal consequences in humans. Other research shows a low intensity vibration treatment can improve bone structure in the lower extremity leg bones of children with CP. In a novel clinical study being conducted by NICHD, researchers are determining the effect of Botox treatment in conjunction with a daily vibration treatment on bone mass and bone structure in children with spastic CP.
Systemic hypothermia—the controlled medical cooling of the body’s core temperature—appears to protect the brain and decrease the rate of death and disability from certain disorders and brain injuries. Previous studies have shown that hypothermia is effective in treating neurologic symptoms in term or late preterm babies less than one month old that are attributed to hypoxic-ischemia (HIE, brain injury due to a severe decrease in the oxygen supply to the body), which can cause quadriplegic CP, with or without movement disorder. In an effort to determine the most effective cooling strategies, NICHD-funded researchers are studying different cooling treatments to improve the chance of survival and neurodevelopment outcomes 18-22 months post-treatment in infants with neurologic symptoms attributed to HIE. Other researchers are examining if combined therapy using hypothermia and recombinant erythropoietin (a hormone that promotes the growth of new red blood cells and increases oxygen levels in the blood) is more effective than either therapy alone in treating neurodevelopmental handicaps in an animal model involving lack of oxygen before, during, or just after birth.
Physical Therapy
What is physical therapy?
Physical therapy (PT) is a branch of rehabilitative health that is considered one of the most important aspects of treating children with Cerebral Palsy. Those with Cerebral Palsy experience mobility, function, posture and balance challenges of varying degrees, and physical therapy – which focuses on basic mobility such as standing, walking, climbing stairs, reaching or operating a wheelchair – is a key element in the multidisciplinary approach to increasing a child’s mobility.
Physical therapy is the rehabilitation of physical impairments by training and strengthening a patient’s large muscles – those in the arms, legs, and abdomen. The goal of physical therapy is to maximize functional control of the body, or increase gross motor function.
The goal of physical therapy is to help individuals:
- develop coordination
- build strength
- improve balance
- maintain flexibility
- optimize physical functioning levels
- maximize independence
Trained and licensed physical therapists identify mobility issues and determine the unique physical abilities and limitations of children, taking into account their age and cognitive functioning, after a diagnosis of Cerebral Palsy is made by a physician.
The therapist will then develop a course of treatment that will include exercises, stretches, and possibly assistive and adaptive equipment designed to achieve mobility. The treatment may also employ the use of passive modalities involving hot and cold packs, ultrasound technology or other means in which the child does not take an active role.
All treatment is designed to meet a child’s individual needs in a way that emphasizes physical fitness, and minimizes injuries and pain
Therapy aids overall treatment goals such as:
- Overcoming physical limitations
- Expanding range of joint motion
- Building and maintaining muscle tone
- Increasing recreational capabilities
- Identifying alternate ways to perform everyday tasks
- Fostering independence
- Decreasing the likelihood of contractures, bone deformity
- Educating children and parents about adaptive equipment
- Providing sensory stimulation
- Increasing fitness
- Increasing flexibility
- Improving posture
- Improving gait
- Minimizing pain and discomfort
Who benefits from physical therapy?
- A child, and his or her parents or caregivers, benefit tremendously from physical therapy because it helps the child overcome physical limitations by increasing mobility, and identifies alternate methods of completing tasks.
The individual with Cerebral Palsy benefits
- This is of benefit to the child because it makes possible something unaffected individuals take for granted: the ability to move from place to place and interact with other children or adults by playing or performing tasks. Therapy also increases overall health by strengthening the body in a way that makes functioning not only possible, but pain and stress-free.
- This is achieved not only by developing strength and flexibility in the body, but also using adaptive techniques – or equipment that can be operated by the child – that will allow the patient an alternate path to perform tasks able-bodied children their age perform.
- Depending on the nature of a child’s Cerebral Palsy, a child can live a near-normal life; persons with the condition have attended college, participated in sports and activities, excelled in their careers and have married.
- Physical therapy empowers the child physically and emotionally, and sets the stage for entering adulthood as an independent individual.
Parents and caregivers benefit
- Parents and caregivers benefit because as a patient progresses, raising a child with Cerebral Palsy becomes less labor intensive. Parents and caregivers are often overwhelmed and under an extreme level of stress.
- They have several responsibilities, including assisting their child with many physical tasks, providing love and emotional support, making sure the child is receiving adequate care in a medical setting and an education at school. The more physical challenges a child can overcome or adapt to, the less hands-on assistance is required of the parents.
- Additionally, a successful physical therapy program allows a parent to see their child interacting with others in a healthy way, building relationships, using their body to the best of his or her ability, and potentially, living independently.
What are the benefits of physical therapy?
- The benefit of physical therapy, for any patient that is experiencing physical limitations, is regaining – or developing – physical mobility.
- By developing a comprehensive plan of treatment, a physical therapist can address limitations in a child’s mobility – and specifically address them. This is achieved through employing exercises that increase physical function, and using adaptive equipment such as wheelchairs, walkers, canes and orthotics to improve performance.
- As a child’s physical abilities improve, the therapist can modify the equipment, or the overall course of therapy, to further advance a child’s treatment.
The largest benefit of therapy to the child with Cerebral Palsy is in treatment of problematic conditions when they occur, including:
- Muscle atrophy or tightening
- Loss in joint range of motion
- Muscle spasticity
- Pain in muscles and joints
- Joint inflammation
- Contractures (muscle rigidity)
The therapists focus on achieving optimal results and minimizing unforeseen complications.
How is physical therapy performed?
Physical therapy is carried out by licensed physical therapists and physical therapy assistants, often by using means such as:
- soft tissue mobilization (kneading of the muscles)
- joint mobilization
- specialized exercises
- stretching
- endurance exercises designed to meet therapeutic goals
Physical therapy is hands-on: a therapist, or an assistant, will guide the child through exercises.
Exercises often include the use of equipment, such as:
- Weights
- Exercise machines
- Bands
- Rollers
- Balance balls
- Heat and cold packs
- Ultrasound technology
At some centers, sports or recreation like swimming, dancing and playing games such as throwing and catching a ball, may be used to help children develop muscles, balance, coordination and range of motion.
- Swimming, because the child is almost entirely submerged in the water, will give children an opportunity to do exercises they cannot do otherwise; moving against the water, kicking and other beneficial exercises can be accomplished in a pool, sometimes in braces. These methods can provide children with an opportunity to play and have fun.
- Adaptive equipment including braces, splints, walkers, orthotics, wheelchairs and even computers will be used in therapy; therapists will modify the equipment as needed. The therapist will also play an instructive role in this regard for children and parents, teaching them how to use the equipment.
Where does physical therapy occur?
- Physical therapy takes place in several settings, including outpatient medical offices or clinics, inpatient rehabilitation centers, specialized physical therapy centers, skilled nursing centers, hospitals, special education classrooms, and in the home.
- The number of physical therapy settings are dependent on several factors; the most important of these is prescribed treatment of the child. Additional considerations include what adaptive equipment is used in treatment, as well as the abilities of a caregiver to provide additional therapy at home. Insurance coverage can also dictate how often a child attends therapy in a clinical setting.
In many cases, a physical therapist will prescribe exercises to be completed at home. The physical therapist or an assistant will train the individual with Cerebral Palsy, the parent or caregiver and the primary caregivers on how to properly perform exercises at home.
What happens during physical therapy?
There is no therapeutic template for Cerebral Palsy since there are many forms of Cerebral Palsy which affect each individual differently.
All physical therapy begins with a diagnosis – the child’s primary doctor will then refer the child to a physical therapist while providing specific treatment goals to accomplish.
At the start of physical therapy, a comprehensive medical history for the child will be obtained. Additionally, the therapist will conduct a series of tests, observations and measurements to assess the child’s body mechanics and function.
The examination may assess:
- Gait
- Range of joint motion
- Physical strength
- Flexibility
- Balance
- Endurance
- Joint integrity
- Posture
- Neuromoter development
- Sensory integration
- Cognitive functioning
- Reflexes
- Breathing, respiration
The therapist then prepares a patient-centered plan of care that takes into account the child’s condition, and the child’s overall environment.
The physical therapist will also determine what orthotic equipment, adaptive equipment, or assistive technologies may be needed to help a child.
Orthotic equipment can include braces that stabilize the ankles, knees, legs, torso, upper arms, lower arms, elbows or hands. Adaptive equipment includes strollers, nets, walkers and wheelchairs. The therapist will teach the child – and his or her caregivers – how to operate the equipment, and will make modifications to accommodate a child’s condition.
Once the child’s plan of treatment is determined, therapists will set goals for a child’s progress, and work with the child to meet those benchmarks. This typically means the therapist and his or her assistants manipulate a child’s body while completing stretches, strength exercises or games with specific movements or purpose.
Often therapy includes instructions for exercises, stretches, posturing and balance to be performed while outside the therapy sessions; at home, school or work.
Who provides physical therapy?
Physical therapy is performed by licensed, accredited physical therapists, or physiotherapists. These professionals are often assisted by physical therapy assistants.
Practicing physical therapists may be doctors, some having earned a master’s degree in physical therapy or kineosiology.
The coursework a budding physical therapist must complete is extensive, and includes:
- biology
- physics
- chemistry
- anatomy
- physiology
- kinesiology
- human growth and development
- examination
- therapeutic practices
Physical therapy assistants – who worked under the supervision of a physical therapist –typically complete bachelor’s or associate degree programs focusing on the same topics as the physical therapist.
All states require licensure via state board examination to practice, though the requirements to take the exam vary from state to state. Most states require the therapist to successfully complete the National Physical Therapy Examination; however, others administer their own examination..
What is the difference between physical therapy and physiotherapy?
- The job of the physical therapist and the physiotherapist is the same – to help a child develop muscular coordination, strength, flexibility and balance to support their mobility.
- Even though the two terms have been used interchangeably, here are some differences between the two professions. A physical therapist is trained to work in private physician practices, specialized centers or clinics. Physiotherapists are found more often in hospitals.
- There is also a slight difference in the approach to therapy; a physical therapist may concentrate solely on physical activities, while a physiotherapist may use ultrasounds or other electronic means to achieve goals.
- Though there used to be several differences in training, most experts agree that requirements to work as a physical therapist or a physiotherapist are very similar.
Is there any risk or special consideration for physical therapy?
- Although physical therapists and their assistants are trained to minimize unforeseen circumstances while carrying out treatment plans with patients, there is some risk associated with therapy. Physical therapy is meant to be restorative in nature – a therapist more often than not will not over-work a patient. However, this can occur.
- If physical therapy is taken too far in a given session, this can cause injury or unnecessary pain, which is not the goal of therapy.
- The key to minimizing risks and maximizing results is open communication between the child, his or her caregivers and physical therapists. Identify where your child’s physical and psychological limits are. Talk to your child regularly to discover difficult areas of therapy. Don’t be afraid to mention your concerns with the therapist.
Adduction deformities
- Adduction is the most common deformity of the hip in children with cerebral palsy. Adduction contractures can cause various difficulties, including scissoring of the legs, hip subluxation, and in severely affected children, difficulty with perineal hygiene.
- For mild contractures, an adductor tenotomy usually is sufficient; more severe contractures often require additional release of the gracilis and the anterior half of the adductor brevis. Neurectomy of the anterior branch of the obturator nerve should be avoided to prevent iatrogenic hip abduction contracture.9–12
Flexion deformities
- Excessive hip flexion brings the center of gravity anteriorly and is compensated for by increased lumbar lordosis, knee flexion, and ankle dorsiflexion. It is important to determine whether the increased hip flexion is the primary deformity or is compensatory to other deformities around the lower extremities, such as knee or ankle contractures. If an unrecognized knee flexion contracture is present, hip flexor release can weaken the hip further and increase hip flexion.
- Hip flexion contractures of 15–30° are usually treated with psoas lengthening through an intramuscular recession over the pelvic brim. Contractures of more than 30° may require more extensive releases of the rectus femoris, sartorius, and tensor fasciae latae and the anterior fibers of the gluteus minimus and medius, in addition to the iliopsoas.
Subluxation and dislocation
- Hip subluxation and dislocation occurs in 7% of ambulators and 60% of dependent sitters. The cause of this progressive deformity of hip is multifactorial and includes muscle imbalance, retained primitive reflexes, abnormal positioning, pelvic obliquity, acetabular dysplasia, excessive femoral anteversion, increased neck-shaft angle, and osteopenia.
- Hip subluxation in patients with cerebral palsy can be difficult to detect clinically because of the presence of abnormal muscle forces and contractures, and because early hip subluxation typically is painless. Routine clinical and radiographic examinations should be done every 6 months, especially in rapidly growing children and patients with spastic quadriplegia.
- Clinically, hips with flexion contractures of more than 20° and abduction of less than 30° are at increased risk of progressive subluxation. Radiographically, a hip at risk has an increased neck-shaft angle and increased femoral anteversion. When a hip at risk is identified, a program of aggressive physical therapy and abduction splinting is started. If further progression continues, operative treatment consisting of soft-tissue release of contracted tendons is indicated.
- Operative correction of femoral valgus and anteversion and acetabular dysplasia is sometimes necessary at this stage. The treatment of an established dislocation is more controversial. A patient with a long-standing dislocation is not a good candidate for a relocation procedure because of the deformities of the proximal femur and acetabulum.
Resection arthroplasty, redirectional osteotomy, arthrodesis have been proposed for the treatment of a painful dislocated hip when a relocation procedure is impossible.
Knee
- Deformities of the knee in patients with cerebral palsy are difficult to evaluate and rarely occur in isolation. Pelvic, hip, knee, ankle, and foot deformities are interrelated. Thus, a careful physical examination of the entire lower extremity is essential when evaluating the knee in patients with cerebral palsy. Important knee deformities are discussed below.
Flexion deformity
- Flexion is the most common knee deformity in patients with cerebral palsy and frequently occurs in ambulatory children. Spastic hamstrings, weak quadriceps, or a combination of both can cause isolated knee flexion. Patients with spastic hip flexors or weak hip extensors or both develop compensatory knee flexion that results in a “jump gait,” in which the hips, knees, and ankles are flexed.
- Patients with weakened gastrocnemius–soleus muscles from cerebral palsy or from Achilles tendon lengthenings, ambulate with knee flexion to accommodate for the relative overpull of the ankle dorsiflexors. The indications for hamstring lengthening are a straight leg raise of less than 70° or a popliteal angle of less than 135° in the absence of significant bony deformity. Care must be taken not to overlengthen the hamstrings because it can lead to excessive weakness and knee hyperextension gait.
Stiff knee gait
- Stiff knee gait is common in patients with cerebral palsy. Cospasticity of the hamstrings and quadriceps causes a loss of knee flexion that leads to decreased power and difficulties with foot clearance during the swing phase of gait. Gait analysis can highlight the spastic muscle. A transfer of the distal rectus femoral tendon to the semitendinosus medially or iliotibial band laterally is recommended, depending on the presence of malrotation.
Recurvatum of the knee
- Recurvatum of the knee is caused by a relative imbalance between the quadriceps and the hamstrings owing to several factors, including
- (1) cospasticity of the quadriceps and hamstrings in which the quadriceps is stronger;
- (2) weakened hamstrings secondary to previous surgery, overlengthening, or transfer;
- (3) gastrocnemius-soleus weakness; and
- (4) ankle equinus. A significant isolated recurvatum should be treated with bilateral long leg braces with a pelvic band with the knees locked in 20° of flexion and ankle stops at 5° of dorsiflexion. When hip control is achieved, the pelvic band can be removed, but long leg braces often are used for years until a stable knee is obtained. Flexion osteotomy for this condition is not recommended.
Foot
- Foot deformities are common in patients with cerebral palsy, with approximately 70%–90% of children affected. The most common deformity is ankle equinus, with equinovarus and equinovalgus deformities being equally common. A foot deformity can have significant effects on the patient’s overall ambulatory level. Common foot deformities are described below.
Equinus deformity
- Conservative treatment of eqiunus consists of stretching, bracing, and occasionally casting. Soleus stretching for 6 h a day can prevent equinus onset. Bracing, especially at night, to prevent the foot from going into the equinus position is essential. Surgery typically is indicated when the ankle cannot be brought into the neutral position in an ambulatory child and when it leads to difficulties with hygiene, shoe wear, and standing rehabilitation in a nonambulatory child.
Varus or valgus deformity
- Varus and valgus deformities can occur in association with an equinus deformity. Valgus is more frequent than varus. It also is important to determine whether the deformity is flexible or rigid because flexible deformities are more likely to be successfully treated nonoperatively with orthotics, shoe modifications and operatively with soft-tissue procedures such as tendon lengthenings, releases, or transfers (usually of the abnormally active muscle). Patients with rigid varus and valgus deformities generally require bone procedures, such as calcaneal osteotomy, subtalar or triple fusions.
- Sometimes, the biomechanics of the hip, knee and tibia also influence the onset and outcome of a foot varus or valgus deformity and should be carefully evaluated. Other common foot deformities in children seen in cerebral palsy are forefoot adduction, hallux valgus and claw toes.
References





