Lumbago is a common disorder involving the muscles, nerves, and bones of the back. Pain can vary from a dull constant ache to a sudden sharp feeling. Low back pain may be classified by duration as acute (pain lasting less than 6 weeks), sub-chronic (6 to 12 weeks), or chronic (more than 12 weeks). The condition may be further classified by the underlying cause as either mechanical, non-mechanical, or referred pain. The symptoms of low back pain usually improve within a few weeks from the time they start, with 40-90% of people completely better by six weeks.
Acute low-back pain without sciatica, with some spread of discomfort to the region of the sacroiliac joint, to the outer part of the buttock as well as to the lateral and the back part of the thigh, is a unifying symptom of a very common clinical syndrome whose exact underlying cause remains often uncertain. Most patients fall then into the category of non-specific low-back pain. Probably the pathogenesis is not uniform, and the pain can arise from a variety of structures (muscles, ligament, spine). Pain which persists after 3 to 4 days should warn the clinician that a serious pathological condition may be present which requires a new approach to diagnosis and treatment.
Pain in the lower part of the back is commonly referred to as Lumbago. It can be defined as mild to severe pain or discomfort in the area of the lower back. The pain can be acute (sudden and severe) or chronic if it has lasted more than three months.
Most people will experience lumbago at some point in their life. It is one of the most common reasons people miss work and visit the doctor. It can occur at any age but is a particular problem in younger people whose work involves physical effort and much later in life, in the elderly.

www.rxharun.com
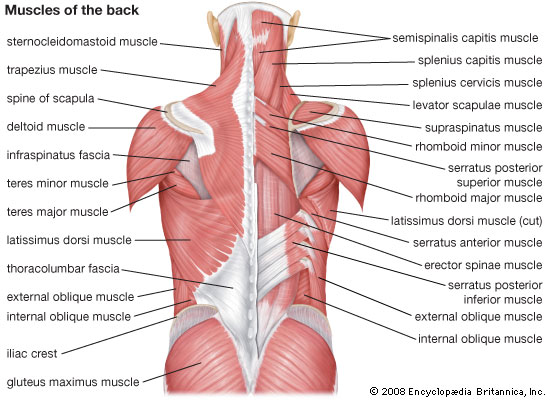
Anatomy of the Low Back
The lumbar spine consists of five vertebrae (L1–L5). The complex anatomy of the lumbar spine is a combination of these strong vertebrae, linked by joint capsules, ligaments, tendons, and muscles, with extensive innervation. The spine is designed to be strong since it has to protect the spinal cord and spinal nerve roots. At the same time, it is highly flexible, providing for mobility in many different planes.
The mobility of the vertebral column is provided by the symphyseal joints between the vertebral bodies, with an IVD in between. The facet joints are located between and behind adjacent vertebrae, contributing to spine stability. They are found at every spinal level and provide about 20% of the torsional (twisting) stability in the neck and low back segments [rx]. Ligaments aid in joint stability during rest and movement, preventing injury from hyperextension and hyperflexion. The three main ligaments are the anterior longitudinal ligament (ALL), posterior longitudinal ligament (PLL), and ligament flavum (LF). The canal is bordered by vertebral bodies and discs anteriorly and by laminae and LF posteriorly. Both the ALL and PLL run the entire length of the spine, anteriorly and posteriorly, respectively. Laterally, spinal nerves and vessels come out from the intervertebral foramen. Beneath each lumbar vertebra, there is the corresponding foramen, from which spinal nerve roots exit. For example, the L1 neural foramina are located just below the L1 vertebra, from where the L1 nerve root exits.
IVDs are located between vertebrae. They are compressible structures able to distribute compressive loads through osmotic pressurization. In the IVD, the annulus fibrosus (AF), a concentric ring structure of organized lamellar collagen, surrounds the proteoglycan-rich inner nucleus pulposus (NP). Discs are avascular in adulthood, except for the periphery. At birth, the human disc has some vascular supply but these vessels soon recede, leaving the disc with little direct blood supply in the healthy adult [rx]. Hence, metabolic support of much of the IVD is dependent on the cartilaginous endplates adjacent to the vertebral body. A meningeal branch of the spinal nerve, better known as the recurrent sinuvertebral nerve, innervates the area around the disc space [rx].
The lumbar spine is governed by four functional groups of muscles, split into extensors, flexors, lateral flexors, and rotators. The lumbar vertebrae are vascularized by lumbar arteries that originate in the aorta. Spinal branches of the lumbar arteries enter the intervertebral foramen at each level, dividing themselves into smaller anterior and posterior branches [rx]. The venous drainage parallels the arterial supply [rx].
Typically, the end of the spinal cord forms the conus medullaris within the lumbar spinal canal at the lower margin of the L2 vertebra [rx]. All lumbar spinal nerve roots stem from the connection between the dorsal or posterior (somatic sensory) root from the posterolateral aspect of the spinal cord and the ventral or anterior (somatic motor) root from the anterolateral aspect of the cord [rx]. The roots then flow down through the spinal canal, developing into the cauda equina, before exiting as a single pair of spinal nerves at their respective intervertebral foramina. Cell bodies of the motor nerve fibers can be found in the ventral or anterior horns of the spinal cord, whereas those of the sensory nerve fibers are in the dorsal root ganglion (DRG) at each level. One or more recurrent meningeal branches, known as the sinuvertebral nerves, run out from the lumbar spinal nerves. The sinuvertebral nerve, or Luschka’s nerve, is a recurrent branch created from the merging of the grey ramus communicans (GRC) with a small branch coming from the proximal end of the anterior primary ramus of the spinal nerve. This polisegmentary mixed nerve directly re-enters the spinal canal and gives off ascending and descending anastomosing branches comprising both somatic and autonomic fibers for the posterolateral annulus, the posterior vertebral body and the periosteum, and the ventral meninges [rx, rx]. The sinuvertebral nerves connect with branches from radicular levels both above and below the point of entry, in addition to the contralateral side, meaning that localizing pain from the involvement of these nerves is challenging [rx]. Also, the facet joints receive two-level innervation comprising somatic and autonomic components. The former convey a well-defined local pain, while the autonomic afferents transmit referred pain.
www.rxharun.com
Causes of Lumbago
The human back is composed of a complex structure of muscles, ligaments, tendons, disks and bones – the segments of our spine are cushioned with cartilage-like pads called disks. Problems with any of these components can lead to back pain. In some cases of back pain, its cause is never found.
Problems with the spine such as osteoporosis can lead to back pain.
Strain – the most common causes of back pain are
- Strained muscles
- Strained ligaments
- A muscle spasm
Things that can lead to strains or spasms include
- Lifting something improperly
- Lifting something that is too heavy
- The result of an abrupt and awkward movement
Structural problems –
- Sprains and strains – account for most acute back pain. Sprains are caused by overstretching or tearing ligaments, and strains are tears in tendon or muscle. Both can occur from twisting or lifting something improperly, lifting something too heavy, or overstretching. Such movements may also trigger spasms in back muscles, which can also be painful.
- Intervertebral disc degeneration – is one of the most common mechanical causes of low back pain, and it occurs when the usually rubbery discs lose integrity as a normal process of aging. In a healthy back, intervertebral discs provide height and allow bending, flexion, and torsion of the lower back. As the discs deteriorate, they lose their cushioning ability.
- Herniated or ruptured discs – can occur when the intervertebral discs become compressed and bulge outward (herniation) or rupture, causing low back pain.
- Radiculopathy – is a condition caused by compression, inflammation and/or injury to a spinal nerve root. Pressure on the nerve root results in pain, numbness, or a tingling sensation that travels or radiates to other areas of the body that are served by that nerve. Radiculopathy may occur when spinal stenosis or a herniated or ruptured disc compresses the nerve root.
- Sciatica – is a form of radiculopathy caused by compression of the sciatic nerve, the large nerve that travels through the buttocks and extends down the back of the leg. This compression causes shock-like or burning low back pain combined with pain through the buttocks and down one leg, occasionally reaching the foot. In the most extreme cases, when the nerve is pinched between the disc and the adjacent bone, the symptoms may involve not only pain, but numbness and muscle weakness in the leg because of interrupted nerve signaling. The condition may also be caused by a tumor or cyst that presses on the sciatic nerve or its roots.
- Spondylolisthesis – is a condition in which a vertebra of the lower spine slips out of place, pinching the nerves exiting the spinal column.
- A traumatic injury – such as from playing sports, car accidents, or a fall can injure tendons, ligaments or muscle resulting in low back pain. Traumatic injury may also cause the spine to become overly compressed, which in turn can cause an intervertebral disc to rupture or herniate, exerting pressure on any of the nerves rooted to the spinal cord. When spinal nerves become compressed and irritated, back pain and sciatica may result.
- Ruptured disks – each vertebra in our spine is cushioned by disks. If the disk ruptures there will be more pressure on a nerve, resulting in back pain.
- Bulging disks – in much the same way as ruptured disks, a bulging disk can result in more pressure on a nerve.
- Sciatica – a sharp and shooting pain that travels through the buttock and down the back of the leg, caused by a bulging or herniated disk pressing on a nerve.
- Arthritis – patients with osteoarthritis commonly experience problems with the joints in the hips, lower back, knees, and hands. In some cases, spinal stenosis can develop, which is the term used to describe when the space around the spinal cord narrows.
- Abnormal curvature of the spine – if the spine curves in an unusual way the patient is more likely to experience back pain. An example is scoliosis, a condition in which the spine curves to the side.
- Osteoporosis – bones, including the vertebrae of the spine, become brittle and porous, making compression fractures more likely.
- Spinal stenosis – is a narrowing of the spinal column that puts pressure on the spinal cord and nerves that can cause pain or numbness with walking and over time leads to leg weakness and sensory loss.
- Skeletal irregularities – include scoliosis, a curvature of the spine that does not usually cause pain until middle age; lordosis, an abnormally accentuated arch in the lower back; and other congenital anomalies of the spine.
- Abdominal aortic aneurysms – occur when the large blood vessel that supplies blood to the abdomen, pelvis, and legs becomes abnormally enlarged. Back pain can be a sign that an aneurysm is becoming larger and that the risk of rupture should be assessed.
- Kidney stones – can cause sharp pain in the lower back, usually on one side.
Below are some other causes of back pain
- Cauda equina syndrome – the cauda equine is a bundle of spinal nerve roots that arise from the lower end of the spinal cord. People with cauda equine syndrome feel a dull pain in the lower back and upper buttocks, as well as analgesia (lack of feeling) in the buttocks, genitalia, and thigh. There are sometimes bowel and bladder function disturbances.
- Cancer of the spine – a tumor located on the spine may press against a nerve, resulting in back pain.
- Infection of the spine – if the patient has an elevated body temperature (fever) as well as a tender warm area on the back, it could be caused by an infection of the spine.
- Other infections – pelvic inflammatory disease (females), bladder, or kidney infections may also lead to back pain.
- Endometriosis – is the buildup of uterine tissue in places outside the uterus.
- Fibromyalgia – a chronic pain syndrome involving widespread muscle pain and fatigue.
- Sleep disorders – individuals with sleep disorders are more likely to experience back pain, compared to others.
- Shingles – an infection that can affect the nerves may lead to back pain, depending on the nerves affected.
- Bad mattress – if a mattress does not support specific parts of the body and keep the spine straight, there is a greater risk of developing back pain.
Everyday activities or poor posture
Back pain can also be the result of some everyday activity or poor posture. Examples include: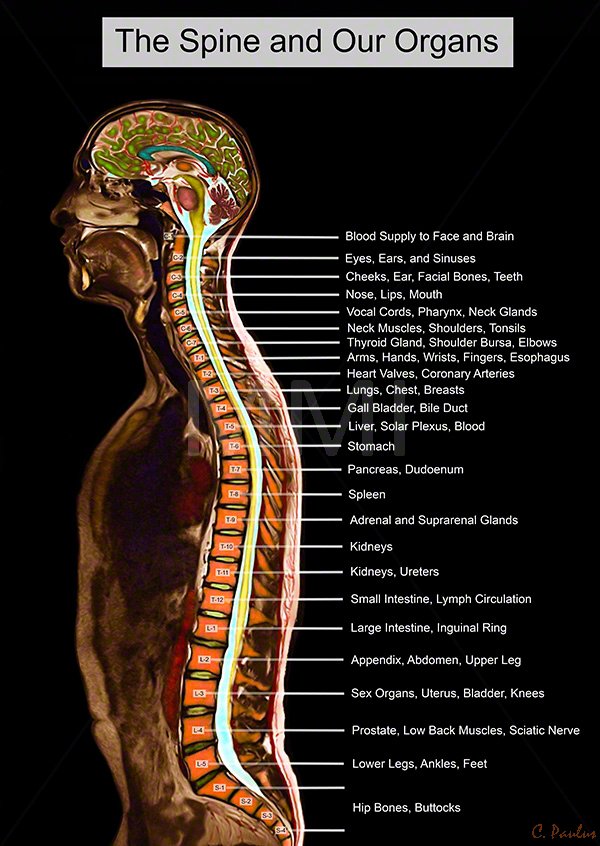
Adopting a very hunched sitting position when using computers can result in increased back and shoulder problems over time.
- Bending awkwardly
- Pushing something
- Pulling something
- Carrying something
- Lifting something
- Standing for long periods
- Bending down for long periods
- Twisting
- Coughing
- Sneezing
- Muscle tension
- Over-stretching
- Straining the neck forward, such as when driving or using a computer
- Long driving sessions without a break, even when not hunched
- Exertion or lifting.
- Severe blow or fall.
- Back disorders.
- Infections.
- Ruptured lumbar disk.
- Nerve dysfunction.
- Osteoporosis.
- Spondylosis (hardening and stiffening of the spinal column).
- Congenital problem.
- Childbirth.
- Often there is no obvious cause.
Jobs That Can Cause Lower Back Pain
- Airline crew (pilots, baggage handlers)
- Surgeons
- Nurses & healthcare workers
- Bus and cab drivers
- Warehouse workers
- Construction workers
- Carpet installers and cleaners
- Farmers (agricultural, dairy)
- Firefighters and police
- Janitors
- Mechanics
- Office personnel (eg, telemarketers, file clerks, computer operators)
The symptom of Lumbago /Backache
The main symptom of back pain is, as the name suggests, an ache or pain anywhere on
- Pain in the back, and sometimes all the way down to the buttocks and legs. Some back issuescan cause pain in other parts of the body, depending on the nerves affected.
- In most cases, signs, and symptoms clear up on their own within a short period. If any of the following signs or symptoms accompany back pain, people should see their doctor:
- Pain. It may be continuous, or only occur when you are in a certain position. The pain may be aggravated by coughing or sneezing, bending or twisting.
- Patients who have been taking steroids for a few months
- Drug abusers
- Patients with cancer
- Patients who have had cancer
- Patients with depressed immune systems
- Stiffness.
According to the British National Health Service (NHS), the following groups of people should seek medical advice if they experience back pain:
- Weight loss
- Elevated body temperature (fever)
- Inflammation (swelling) on the back
- Persistent back pain – lying down or resting does not help
- Pain down the legs
- Pain reaches below the knees
- A recent injury, blow or trauma to your back
- Urinary incontinence – you pee unintentionally (even small amounts)
- Difficulty urinating – passing urine is hard
- Fecal incontinence – you lose your bowel control (you poo unintentionally)
- Numbness around the genitals
- Numbness around the anus
- Numbness around the buttocks
- dull ache,
- numbness,
- tingling,
- sharp pain,
- pulsating pain,
- pain with movement of the spine,
- pins and needles sensation,
- muscle spasm,
- tenderness,
- sciatica with shooting pain down one or both lower extremities
- People aged less than 20 and more than 55 years
- Additionally, people who experience pain symptoms after a major trauma (such as a car accident) are advised to see a doctor. If low back pain interferes with daily activities, mobility, sleep, or if there are other troubling symptoms, medical attention should be sought.
Risk increases with
- Biomechanical risk factors.
- Sedentary occupations.
- Gardening and other yard work.
- Sports and exercise participation, especially if infrequent.
- Obesity.
Preventive measures
- Exercises to strengthen lower back muscles.
- Learn how to lift heavy objects.
- Sit properly.
- Back support in bed.
- Lose weight, if obese.
- Choose proper footwear.
- Wear special back support devices.
Red flag conditions indicating possible underlying spinal pathology or nerve root problemsw9
Red flags
-
Onset age < 20 or > 55 years
-
Non-mechanical pain (unrelated to time or activity)
-
Thoracic pain
-
Previous history of carcinoma, steroids, HIV
-
Feeling unwell
-
Weight loss
-
Widespread neurological symptoms
-
Structural spinal deformity
Indicators for nerve root problems
-
Unilateral leg pain > low back pain
-
Radiates to foot or toes
-
Numbness and paraesthesia in same distribution
-
Straight leg raising test induces more leg pain
-
Localized neurology (limited to one nerve root)
Diagnosis of Lumbago /Backache
Suspected disk, nerve, tendon, and other problems – X-rays or some other imaging scan, such as a CT (computerized tomography) or MRI (magnetic resonance imaging) scan may be used to get a better view of the state of the soft tissues in the patient’s back.
- Blood tests – CBC ,ESR,Hb, RBS,CRP, Serum Creatinine,Serum Electrolyte,
- Myelograms
- Discography.
- Electrodiagnostics
- Bone scans
- Ultrasound imaging
- X-rays – can show the alignment of the bones and whether the patient has arthritis or broken bones. They are not ideal for detecting problems with muscles, the spinal cord, nerves or disks.
- MRI or CT scans – these are good for revealing herniated disks or problems with tissue, tendons, nerves, ligaments, blood vessels, muscles, and bones.
- Bone scan – a bone scan may be used for detecting bone tumors or compression fractures caused by brittle bones (osteoporosis). The patient receives an injection of a tracer (a radioactive substance) into a vein. The tracer collects in the bones and helps the doctor detect bone problems with the aid of a special camera.
- Electromyography or EMG – the electrical impulses produced by nerves in response to muscles is measured. This study can confirm nerve compression which may occur with a herniated disk or spinal stenosis (narrowing of the spinal canal).
| Syndrome | Findings | Assessment/Plan |
|---|---|---|
| Facet syndrome | History and physical examination:
Radiological findings (not indicated on initial evaluation):
|
Differential diagnosis:
Treatment: |
| Sacro-iliac joint syndrome | History and physical examination:
Radiological findings (not indicated on intial evaluation):
|
Functional disturbance: muscular imbalance Treatment: stabilizing exercises, analgesics (1–3 days) if needed, manual medicine, sacro-iliac joint injection if indicated |
| Myofascial pain syndrome | History and physical examination:
Radiological and histological findings:
|
Local treatment: |
| Functional instability | History and physical examination:
Radiological findings:
|
|
The differential diagnosis for back pain is very broad, especially when considering the pediatric population. Below is a review of the more common diagnoses along with history or physical exam features that may increase your index of suspicion. This list is not comprehensive but represents the more likely and more concerning conditions that make up the differential.
-
Lumbosacral muscle strains/sprains
-
Presentation: follows traumatic incident or repetitive overuse, pain worse with movement, better with rest, restricted range of motion, tenderness to palpation of muscles
-
-
Lumbar spondylosis
-
Presentation: patient typically is greater than 40years old, pain may be present or radiate from hips, pain with extension or rotation, neurologic exam is usually normal
-
-
Disk herniation
-
Presentation: usually involves the L4 to S1 segments, may include paresthesia, sensory change, loss of strength or reflexes depending on severity and nerve root involved
-
-
Spondylolysis, Spondylolisthesis
-
Presentation: similar to pediatrics, spondylolisthesis may present back pain with radiation to buttock and posterior thighs, neuro deficits are usually in the L5 distribution
-
-
Vertebral compression fracture
-
Presentation: localized back pain worse with flexion, point tenderness on palpation, may be acute or occur insidiously over time, age, chronic steroid use, and osteoporosis are risk factors
-
-
Spinal stenosis
-
Presentation: back pain which can be accompanied with sensory loss or weakness in legs relieved with rest (neurologic claudication), neuro exam normal.
-
-
Tumor
-
Presentation: a history of metastatic cancer, unexplained weight loss, focal tenderness to palpation in the setting of risk factors
-
Clinical note: 97% of spinal tumors are metastatic disease; however, the provider should keep multiple myeloma in the differential
-
-
Infection: vertebral osteomyelitis, discitis, septic sacroiliitis, epidural abscess, paraspinal muscle abscess
-
Presentation: Spinal procedure within the last 12 months, Intravenous drug use, Immunosuppression, prior lumbar spine surgery, fever, wound in spinal region, localized pain, and tenderness
-
Clinical note: Granulomatous disease may represent as high as one-third of cases in developing countries.
-
-
Fracture
-
Presentation: Significant trauma (relative to age), Prolonged corticosteroid use, osteoporosis, and age greater than 70 years, Contusions, abrasions, tenderness to palpation over spinous processes
-
Pediatrics[rx][rx][rx][rx][rx][rx][rx]:
-
Tumor
-
Presentation: fever, malaise, weight loss, nighttime pain, recent onset scoliosis
-
Clinical note: Osteoid osteoma is the most common tumor that presents with back pain – classically, the pain is promptly relieved with anti-inflammatory drugs such as NSAIDS
-
-
Infection: vertebral osteomyelitis, discitis, septic sacroiliitis, epidural abscess, paraspinal muscle abscess
-
Presentation: fever, malaise, weight loss, nighttime pain, recent onset scoliosis
-
Clinical notes: Epidural abscess should be a consideration with the presence of fever, spinal pain, and neurologic deficits or radicular pain; discitis may present with a patient refusing to walk or crawl
-
-
Herniated disk, slipped apophysis
-
Presentation: Acute pain, radicular pain, positive straight leg raise test, pain with spinal forward flexion, recent onset scoliosis
-
-
Spondylolysis, spondylolisthesis, lesion or injury to the posterior arch
-
Presentation: Acute pain, radicular pain, positive straight leg raise test, pain with spinal extension, tight hamstrings
-
-
Vertebral fracture
-
Presentation: acute pain, other injuries, traumatic mechanism of injury, neurologic loss
-
-
Muscle strain
-
Presentation: acute pain, muscle tenderness without radiation
-
-
Scheuermann’s kyphosis
-
Presentation: chronic pain, rigid kyphosis
-
-
Inflammatory spondyloarthropathies
-
Presentation: chronic pain, morning stiffness lasting greater than 30min, sacroiliac joint tenderness
-
-
Psychological Disorder (conversion, somatization disorder)
-
Presentation: normal evaluation but persistent subjective pain
-
-
Idiopathic Scoliosis:
-
Presentation: positive Adam’s test (for larger angle curvature), most commonly asymptomatic
-
Clinical note: Of note, no definitive evidence that scoliosis causes pain, but patients with scoliosis have more frequently reported pain; therefore provider should rule out other causes before attributing pain to scoliosis
-
Treatment of Lumbago /Backache
General measures
- Bed rest for the first 24 hours. Additional bed rest will be determined by the severity of the problem. Recent medical studies indicate that staying more active is better for back disorders than prolonged bed rest.
- Use a firm mattress (place a bed board under the mattress if needed).
- An ice pack or cold massage or heat applied to the affected area with a heating pad or hot water bottle.
- Physical therapy.
- Massage may help. Be sure the person is well-trained or massage could cause more harm than help.
- Wear a special back support device.
- Other options are available depending on the degree of injury, such as surgery (if disk damaged), electrical nerve stimulation, acupuncture, special shoes, etc.
- Stress reduction techniques, if needed.
- Non-Prescription Pain Relievers – Naproxen, acetaminophen, and ibuprofen each reduce inflammation and pain. Though these drugs are available over-the-counter, they are potent and taking more than the recommended dose can harm health. A doctor can help with advice about the right kind of non-prescription pain reliever to take.
- Cold and Heat – Applying a cold pack to the painful part of the back contracts inflamed muscle and relieves pain. This treatment helps a great deal when the disk has recently ruptured and swelling is at its greatest. A heating pad or warm pack helps with residual pain.
- Continued Physical Activity – Though pain or weakness seem like good reasons to rest the back, excessive bed-rest worsens the symptoms of a slipped disc. Moving around too little allows muscles to grow weaker and prevents the body from healing. Periods of rest interspersed with periods of normal activity throughout the day keep the back muscles in shape.
- Prescription Remedies – If over-the-counter drugs fail to ease slipped disc pain, the doctor will turn to prescription medications. These can include narcotics, such as hydrocodone or codeine. While they can do away with pain, narcotics are very addictive and induce a mental fogginess that can itself be dangerous. More narrowly-focused medicines designed to target damaged nerves that create chronic pain may be a better choice, as they have fewer undesirable side effects. Gabapentin and Cymbalta are two drugs that act in different ways to minimize nerve pain. These drugs are less addictive than narcotics.
- Physical Therapy – Physical therapists show slipped disc sufferers ways to move that do not cause pain. Occupational therapists teach skills that allow patients to return to a productive life.
- Nutrition – In order to restore the disc we also are going to need to include different substances in our diet. There are a lot of supplements on the market, of course. If you wish to try them, that’s fine. I personally don’t like them. I have tried one with glucosamine and chondroitin, but I didn’t feel any different. So, if you have the opportunity to take these with the food or from more natural sources, it will be great. You can find these substances in seafood and animal cartilages and by digesting them we ensure the building blocks for the connecting tissue for our joints and spine. Also, we will need more Omega 3 fatty acids, which can be supplied from cold-pressed oils, fatty fish, flax seeds, chia and many more. Vitamins from the B group are very beneficial for people with herniated discs and all kinds of issues with the peripheral nervous system. Vitamins B1, B6 and B12 nourish the nerves and help them recover from the disk accident. Usually, doctors prescribe them as a part of the treatment, but it is worth mentioning anyway.
- A good massage – A massage is one of the natural methods of relieving pain. Individuals who get a massage weekly for several months stand a better chance of alleviating back pain. A good massage provides a person with many health benefits that lessen back pain. A massage triggers the release of endorphins. Endorphins aid in decreasing anxiety and relieving pain. They offer a relaxation effect by softening muscles that are injured preventing cramping.
- Undertaking yoga – Yoga is an applicable strategy for keeping the level of back pain at minimal levels. Taking yoga sessions often is very effective method of dealing with back pain. With yoga, there is a high likelihood of proper body functions. The use of pain prescriptions is also diminished. Patients suffering from back pain related issues do not have to rely on these prescriptions to manage pain. Incorporating laughter in yoga is a good way of exercising. Yoga incorporates simple yet appropriate exercises that enhance the stretching of muscles. Laughter with yoga stimulates relieving of pain. It facilitates increased uptake of oxygen, little anxiety, and production of endorphins. All these variables play an essential role in diminishing back pain.
- Adjusting sleeping position – A simple sleeping mistake can immensely contribute to back pain. A poor sleeping position can cause stress and tension on the muscles contributing to back pain. Altering one’s sleeping position and adopting a style that does not exert a lot of stress on the back is a recommended tactic. Nurturing sleeping habits such as assuming a reclining position, using wedge-shaped cushions and getting adjustable beds from reputable medical institutions are easy techniques to endorse. If a reclining position does not suit an individual, the other two techniques can be embraced.
- Heat therapy – Several considerations should be observed when using heat therapy. The right temperature ought to be set so as to ensure a patient does not face risks associated with too much exposure to heat. The key objective should be to ensure enough access of heat to the muscles to yield benefits for the patient. The adoption of heat therapy for easing back pain is determined by the magnitude of pain a person is experiencing. In cases where relatively low back pain is encountered, short heat therapy sessions are recommended. On the other hand, if an individual is experiencing prolonged back pain, long heat therapy sessions are the most applicable.
- Taking hot baths – This is a form of heat therapy that aims at relieving back pain. It guarantees permeation of heat into the muscles leading to reduced pain. Many individuals opt for this method since they believe it achieves competent results. Hot baths initiate a fast process of blood supply to stiff neck and back muscles. When this happens, the muscles relax and stretch leading to decreased back pain. To avoid interference with one’s sleeping patterns, a hot bath should be taken several hours before retiring to bed.
- Aquatic therapy – This natural technique involves physical therapy in a pool. Individuals get the best out of this therapy by relying on the resistance of water. Consistency in undertaking this therapy is what ascertains getting back pain relief. Integrating aquatic therapy in an individual’s life for the better part of the week enhances the reduction of back pain quickly.
- Enlighten others – Individuals have the power to devise their own natural strategies that aid them in coping with back pain. The strategies can also be a good remedy for others going through similar circumstances. An individual can use social media platforms to equip others with important tips on how to keep back pain at bay. Further, becoming a member of associations that address back pain issues enables better communication of the knowledge gained from personal experience.
Treatments for acute and chronic low back pain Rx
| Effectiveness | Acute low back pain | Chronic low back pain |
|---|---|---|
| Beneficial | Advice to stay active, non-steroidal anti-inflammatory drugs (NSAIDs) | Exercise therapy, Intensive multidisciplinary treatment programs |
| Trade-off | Muscle relaxants | Muscle relaxants |
| Likely to be beneficial | Spinal manipulation, behavior therapy, multidisciplinary treatment programs (for subacute low back pain) | Analgesics, acupuncture, antidepressants, back schools, behavior therapy, NSAIDs, spinal manipulation |
| Unknown | Analgesics, acupuncture, back schools, epidural steroid injections, lumbar supports, massage, multidisciplinary treatment (for acute low back pain), transcutaneous electrical nerve stimulation, traction, temperature treatments, electromyographical biofeedback | Epidural steroid injections, EMG biofeedback, lumbar supports, massage, transcutaneous electrical nerve stimulation, traction, local injections |
| Unlikely to be beneficial | Specific back exercises | — |
| Ineffective or harmful | Bed rest | Facet joint injections |
Medications
A wide range of medications is used to treat acute and chronic low back pain. Some are available over the counter (OTC); others require a physician’s prescription. Certain drugs, even those available OTC, may be unsafe during pregnancy, may interact with other medications, cause side effects, or lead to serious adverse effects such as liver damage or gastrointestinal ulcers and bleeding. Consultation with a health care provider is advised before use. The following are the main types of medications used for low back pain:
- Analgesic medications – are specifically designed to relieve pain. They include OTC acetaminophen and aspirin, as well as prescription opioids such as codeine, oxycodone, hydrocodone, and morphine. Opioids should be used only for a short period of time and under a physician’s supervision. People can develop a tolerance to opioids and require increasingly higher dosages to achieve the same effect. Opioids can also be addictive. Their side effects can include drowsiness, constipation, decreased reaction time, and impaired judgment. Some specialists are concerned that chronic use of opioids is detrimental to people with back pain because they can aggravate depression, leading to a worsening of the pain.
- Nonsteroidal anti-inflammatory drugs (NSAIDS) – relieve pain and inflammation and include OTC formulations (ibuprofen, ketoprofen, and naproxen sodium). Several others, including a type of NSAID called COX-2 inhibitors, are available only by prescription. Long-term use of NSAIDs has been associated with stomach irritation, ulcers, heartburn, diarrhea, fluid retention, and in rare cases, kidney dysfunction and cardiovascular disease. The longer a person uses NSAIDs the more likely they are to develop side effects. Many other drugs cannot be taken at the same time a person is treated with NSAIDs because they alter the way the body processes or eliminates other medications.
- Anticonvulsants—drugs primarily used to treat seizures—may be useful in treating people with radiculopathy and radicular pain.
- Antidepressants – such as tricyclics and serotonin and norepinephrine reuptake inhibitors have been commonly prescribed for chronic low back pain, but their benefit for nonspecific low back pain is unproven, according to a review of studies assessing their benefit.
- Muscle Relaxants – If the muscles around the slipped disc experience painful spasms, a muscle relaxant such as Valium may be useful. The drawback to drugs like these is that they do not limit their power to the affected nerve. Instead, they have a generally relaxing effect and will interfere with daily activities. Such as cyclobenzaprine (Flexeril), might be prescribed to relieve the discomfort associated with muscle spasms. However, these medicines might cause confusion in older people. Depending on the level of pain, prescription pain medicines might be used in the initial period of treatment.
- Steroids – If inflammation is severe, a doctor may also prescribe a steroid. Steroids, such as cortisone, reduce swelling quickly. A cortisone shot directly in the affected area will have an immediate effect on the displaced disc.
- Counter-irritants – such as creams or sprays applied topically stimulate the nerves in the skin to provide feelings of warmth or cold in order to dull the sensation of pain. Topical analgesics reduce inflammation and stimulate blood flow.
- Nerve Relaxant — Pregabalin or gabapentin and anti-inflammatory drugs help to relieve pain and stiffness, allowing for increased mobility and exercise. There are many common over-the-counter medicines called non-steroidal anti-inflammatory drugs (NSAIDs). They include aspirin, ibuprofen (Motrin, Advil), and naproxen (Naprosyn, Aleve).
- Carisoprodol – This muscle relaxant was investigated in two high-quality studies on acute low back pain. The first study compared carisoprodol with diazepam [rx]. Carisoprodol was superior in performance on all the outcome parameters measured. A comparison of carisoprodol with cyclobenzaprine‐hydrochloride in the second study revealed no statistically significant differences between the two treatments [rx].
- Chlorzoxazone – This muscle relaxant was compared with tizanidine in one high-quality study in a very small sample of patients with degenerative lumbar disc disease [rx]. No differences were found between the treatments.
- Cyclobenzaprine‐hydrochloride – Cyclobenzaprine was compared with diazepam in a low-quality trial on chronic low back pain, but no significant differences between the treatments were identified [rx]. There was also no significant difference between cyclobenzaprine and carisoprodol in one high-quality study on acute low back pain [rx].
- Diazepam – In comparison with carisoprodol, diazepam was found to be inferior in performance on muscle spasm, global efficacy and functional status in a high-quality trial on acute low back pain [rx]. In a very small high-quality trial (30 people) comparing diazepam with tizanidine, there were no differences in pain, functional status and muscle spasm after seven days [rx].
- Tizanidine – This muscle relaxant was compared with chlorzoxazone and diazepam in two very small high quality [rx]. Both trials did not find any differences in pain, functional status and muscle spasm after 7 days.
- Pridinol mesylate – One low-quality trial showed no differences between this muscle relaxant and thiocolchicoside on pain relief and global efficacy.
Advanced Treatment of
- Spinal manipulation and spinal mobilization – Are approaches in which professionally licensed specialists (doctors of chiropractic care) use their hands to mobilize, adjust, massage, or stimulate the spine and the surrounding tissues. Manipulation involves a rapid movement over which the individual has no control; mobilization involves slower adjustment movements. The techniques have been shown to provide small to moderate short-term benefits in people with chronic low back pain. Evidence supporting their use for acute or subacute low back pain is generally of low quality. Neither technique is appropriate when a person has an underlying medical cause for back pain such as osteoporosis, spinal cord compression, or arthritis.
- Traction – involves the use of weights and pulleys to apply constant or intermittent force to gradually “pull” the skeletal structure into better alignment. Some people experience pain relief while in traction, but that relief is usually temporary. Once traction is released the back pain tends to return. There is no evidence that traction provides any longterm benefits for people with low back pain.
- Spinal injections — An injection of a cortisone-like anti-inflammatory medicine into the lower back might help reduce swelling and inflammation of the nerve roots, allowing for increased mobility.
- Biofeedback – It is used to treat many acute pain problems, most notably back pain and headache. The therapy involves the attachment of electrodes to the skin and the use of an electromyography machine that allows people to become aware of and self-regulate their breathing, muscle tension, heart rate, and skin temperature. People regulate their response to pain by using relaxation techniques. Biofeedback is often used in combination with other treatment methods, generally without side effects. The evidence is lacking that biofeedback provides a clear benefit for low back pain.
- Nerve block therapies – aim to relieve chronic pain by blocking nerve conduction from specific areas of the body. Nerve block approaches range from injections of local anesthetics, botulinum toxin, or steroids into affected soft tissues or joints to more complex nerve root blocks and spinal cord stimulation. When extreme pain is involved, low doses of drugs may be administered by catheter directly into the spinal cord. The success of a nerve block approach depends on the ability of a practitioner to locate and inject precisely the correct nerve. Chronic use of steroid injections may lead to increased functional impairment.
Surgery Lumbago
When other therapies fail, surgery may be considered an option to relieve pain caused by serious musculoskeletal injuries or nerve compression. It may be months following surgery before the patient is fully healed, and he or she may suffer permanent loss of flexibility.
- Vertebroplasty and kyphoplasty – are minimally invasive treatments to repair compression fractures of the vertebrae caused by osteoporosis. Vertebroplasty uses three-dimensional imaging to assist in guiding a fine needle through the skin into the vertebral body, the largest part of the vertebrae. Glue-like bone cement is then injected into the vertebral body space, which quickly hardens to stabilize and strengthen the bone and provide pain relief. In kyphoplasty, prior to injecting the bone cement, a special balloon is inserted and gently inflated to restore height to the vertebral structure and reduce spinal deformity.
- Spinal laminectomy – (also known as spinal decompression) is performed when spinal stenosis causes a narrowing of the spinal canal that causes pain, numbness, or weakness. During the procedure, the lamina or bony walls of the vertebrae, along with any bone spurs, are removed. The aim of the procedure is to open up the spinal column to remove pressure on the nerves.
- Discectomy or microdiscectomy – may be recommended to remove a disc, in cases where it has herniated and presses on a nerve root or the spinal cord, which may cause intense and enduring pain. Microdiscectomy is similar to a conventional discectomy; however, this procedure involves removing the herniated disc through a much smaller incision in the back and a more rapid recovery. Laminectomy and discectomy are frequently performed together and the combination is one of the more common ways to remove pressure on a nerve root from a herniated disc or bone spur.
- Foraminotomy – is an operation that “cleans out” or enlarges the bony hole (foramen) where a nerve root exits the spinal canal. Bulging discs or joints thickened with age can cause narrowing of the space through which the spinal nerve exits and can press on the nerve, resulting in pain, numbness, and weakness in an arm or leg. Small pieces of bone over the nerve are removed through a small slit, allowing the surgeon to cut away the blockage and relieve pressure on the nerve.
- Intradiscal electrothermal therapy (IDET) – is a treatment for discs that are cracked or bulging as a result of degenerative disc disease. The procedure involves inserting a catheter through a small incision at the site of the disc in the back. A special wire is passed through the catheter and an electrical current is applied to heat the disc, which helps strengthen the collagen fibers of the disc wall, reducing the bulging and the related irritation of the spinal nerve. IDET is of questionable benefit.
- Nucleoplasty also called plasma disc decompression (PDD) – is a type of laser surgery that uses radiofrequency energy to treat people with low back pain associated with mildly herniated discs. Under x-ray guidance, a needle is inserted into the disc. A plasma laser device is then inserted into the needle and the tip is heated to 40-70 degrees Celsius, creating a field that vaporizes the tissue in the disc, reducing its size and relieving pressure on the nerves. Several channels may be made depending on how tissue needs to be removed to decompress the disc and nerve root.
- Radiofrequency denervation – is a procedure using electrical impulses to interrupt nerve conduction (including the conduction of pain signals). Using x-ray guidance, a needle is inserted into a target area of nerves and a local anesthetic is introduced as a way of confirming the involvement of the nerves in the person’s back pain. Next, the region is heated, resulting in localized destruction of the target nerves. Pain relief associated with the technique is temporary and the evidence supporting this technique is limited.
- Spinal fusion – is used to strengthen the spine and prevent painful movements in people with degenerative disc disease or spondylolisthesis (following laminectomy). The spinal disc between two or more vertebrae is removed and the adjacent vertebrae are “fused” by bone grafts and/or metal devices secured by screws. The fusion can be performed through the abdomen, a procedure known as an anterior lumbar interbody fusion, or through the back, called posterior fusion. Spinal fusion may result in some loss of flexibility in the spine and requires a long recovery period to allow the bone grafts to grow and fuse the vertebrae together. Spinal fusion has been associated with an acceleration of disc degeneration at adjacent levels of the spine.
- Artificial disc replacement – is considered an alternative to spinal fusion for the treatment of people with severely damaged discs. The procedure involves removal of the disc and its replacement by a synthetic disc that helps restore height and movement between the vertebrae.
Other Rx of Lumbago /Backache
Chiropractic Care
Sixty percent of people with sciatica who didn’t get relief from other therapies and then tried spinal manipulation experienced the same degree of pain relief as patients who eventually had surgery, found a 2010 study in the Journal of Manipulative and Physiological Therapeutics. The 120 people in the study saw a chiropractor about 3 times a week for 4 weeks and then continued weekly visits, tapering off treatment as they felt better. In people who responded to chiropractic care, benefits lasted up to a year. “Spinal manipulation may create a response in the nervous system that relieves pain and restores normal mobility to the injured area,” says study researcher Gordon McMorland, DC, of National Spine Care in Calgary, Alberta. “It also reduces inflammation, creating an environment that promotes the body’s natural healing mechanisms.”
Acupuncture
You can get relief as soon as the first session, though it takes about 12 sessions to see improvement,” says Jingduan Yang, MD, assistant professor at the Jefferson Myrna Brind Center of Integrative Medicine at Thomas Jefferson University. A small study in the Journal of Traditional Chinese Medicine found that of 30 people with sciatica, 17 got complete relief and 10 saw symptoms improve with warming acupuncture, in which the needles are heated.
Yoga
A study in the journal Pain reported that people with chronic back pain who practiced Iyengar yoga for 16 weeks saw pain reduced by 64% and disability by 77%. Although yoga’s effects on sciatica are less clear, gentle forms may be beneficial. By strengthening muscles and improving flexibility, a yoga practice can help sciatica sufferers “move and function better so they don’t fall into a posture that aggravates sciatica,” says James W. Carson, Ph.D., a psychologist at the Comprehensive Pain Center at Oregon Health & Science University. For extra grip and stability, try these grip socks from Natural Fitness.
Massage
Don’t expect a chilled-out spa massage if you have sciatica. In this instance, trigger-point therapy is best, says Jeff Smoot, vice president of the American Massage Therapy Association. The sciatic nerve sits underneath a muscle called the piriformis, which is located beneath the glutes. “When the piriformis muscle gets tight, it pinches the sciatic nerve, causing tingling and numbness down into the leg,” says Smoot. He applies pressure to irritated and inflamed areas, or trigger points, in the piriformis muscle, as well as in muscles in the lower back and glutes. Typically, Smoot schedules treatments 7 to 10 days apart. If patients don’t see progress by the fourth visit, “they need to try another form of therapy,” he says.
Shiatsu,
Also known as finger pressure therapy, is a type of massage where pressure is applied along energy lines in the body. The shiatsu therapist applies pressure with his/her fingers, thumbs and elbows.
Topical Preparations
St. John’s wort oil, a liniment, is “one of my favorites for nerve pain,” says Tieraona Low Dog, MD, director of the fellowship at the Arizona Center for Integrative Medicine. Apply the anti-inflammatory oil two or three times a day where there’s a pain. Another option: an OTC cayenne pepper plaster or cream; capsaicin, found in chiles, hinders the release of pain-causing compounds from nerves. For severe cases, Low Dog uses the prescription chile patch Qutenza, designed for shingles pain. “One application is effective for weeks,” says Low Dog.
Ice or Heat
Because the sciatic nerve is buried deep within the buttock and leg, ice or heat on the surface of the body won’t ease that inner inflammation. But the time-honored treatments can act as counterirritants—that is, “they give your body other input in the painful area, and that brings the pain down a notch,” says Ruppert. Apply an ice pack or a heating pad as needed for 15 minutes.
Devil’s Claw
The herbal medication devil’s claw is “quite a potent anti-inflammatory, working like ibuprofen and similar drugs to inhibit substances that drive inflammation,” says Low Dog. She generally starts patients on 1,500 to 2,000 mg twice a day. Look for a brand that has a standardized extract of roughly 50 mg of harpagoside, the active compound. Safety reviews show that the supplement is well tolerated by most people but should be avoided by patients with peptic ulcers or on blood-thinning medications.
CBT (cognitive behavioral therapy)
- CBT can help patients manage chronic back pain. The therapy is based on the principle that the way a person feels is, in part, dependent on the way they think about things. People who can be taught to train themselves to react in a different way to pain may experience less perceived pain. CBT may use relaxation techniques as well as strategies to maintain a positive attitude. Studies have found that patients with CBT tend to become more active and do exercise, resulting in a lower risk of back pain recurrence.
Exercise and Physical Therapy
- Moving is usually the last thing people dogged by sciatica want to do, but it’s important to be physically active. Lying in bed makes it more likely that the pain will last longer, says Ruppert. Exercise increases blood flow to the disk and the nerve, helping to get rid of the chemicals causing the inflammation. Take 15- to 20-minute walks. If that hurts too much, give swimming or water aerobics a try; there’s not as much pressure on the back when you’re in the water, says Ruppert. It may also be worth seeing a physical therapist, who can prescribe stretching exercises to restore flexibility to the back or moves that strengthen core muscles, helping to stabilize the spine and reduce the likelihood of a similar injury.
Here are six exercises for Lumbago /Backache
Pigeon pose
- Pigeon Pose is a common yoga pose. It works to broadly open the hips. There are multiple versions of this stretch. The first is a starting version of the pigeon pose, known as the reclining pigeon pose. If you are just starting your treatment, you should try the reclining pose first. Once you can do the reclining version without pain, work with your physical therapist on the sitting and forward versions.
Reclining pose
- While on the back, bring your right leg up to a right angle and grasp it with both hands behind the thigh, locking your fingers.
- Take your left leg and place your ankle against the knee. Hold the position for a moment before changing legs. This helps stretch the tiny piriformis muscle, which sometimes becomes inflamed and presses against the sciatic nerve causing pain.
- Repeat by switching sides and doing the same exercise with the other leg.
Sitting pose
- Sit on the floor with your legs stretched out straight in front of you. Then bend your right leg, putting your right ankle on top of the left knee.
- Lean forward and allow your upper body to lean toward your thigh. Hold for 15 to 30 seconds and then switch sides. This stretches the glutes and lowers back.
Forward pose
- Kneel on the floor on all fours.
- Pick up your right leg and move it forward so that your lower leg is on the ground, horizontal to the body. Your right foot should be in front of your right knee while your right knee stays to the right.
- Stretch the left leg out all the way behind you on the floor, with the top of the foot on the ground and toes pointing back.
- Shift your body weight gradually from your arms to your legs so that your legs are supporting your weight. Sit up straight with your hands on either side of your legs.
- Take a deep breath. While exhaling, lean your upper body forward over your lower leg. Support your weight with your arms as much as possible.
Knee to the opposite shoulder
This simple stretch helps relieve sciatica pain by loosening your gluteal and piriformis muscles, which can become inflamed and press against the sciatic nerve.
- Lie on your back with your legs extended outward and your feet flexed upward.
- Clasp your hands around your knee and gently pull your right leg across your body toward your left shoulder. Hold it there for 30 seconds and then push your knee so your leg returns to its starting position.
- Repeat for a total of 3 reps, and then switch legs. Remember to only pull your knee as far as it will comfortably go. You should feel a relieving stretch in your muscles, not pain.
Sitting spinal stretch
Sciatica pain is triggered when vertebrae in the spine compress. This stretch helps create space in the spine to relieve pressure from the sciatic nerve.
- Sit on the ground with your legs extended straight out with your feet flexed upward.
- Bend your right knee and place your foot flat on the floor on the outside of your opposite knee.
- Place your left elbow on the outside of your right knee to help you gently turn your body toward the right. Hold for 30 seconds and repeat three times, then perform this stretch with your left leg bent and body turned to the left side.
Standing hamstring stretch
This stretch can help ease pain and tightness in the hamstring caused by sciatica.
- Place your right foot on an elevated surface at or below your hip level. This could be a chair, ottoman, or step on a staircase. Flex your foot so your toes and leg are straight. If your knee tends to hyperextend, keep a slight bend in it.
- Bend your body forward slightly toward your foot. The further you go, the deeper the stretch. Do not push so far that you feel pain.
- Release the hip of your raised leg downward as opposed to it lifting up. If you need help easing your hip down, loop a yoga strap or long exercise band over your right thigh and under your left foot. Hold for at least 30 seconds, and then repeat on the other side.
Exercise with care
Kovacs emphasizes that you should not assume that you will be able to be as flexible as the exercises ideally call for. Don’t think that because of what you see on YouTube or TV that you can get into these positions, he said. Most people who demonstrate the exercises have great flexibility and have been doing it for years. If you have any kind of pain, you should stop.”
- Corina Martinez – a physical therapist at Duke Sports Medicine Center and a member of the American Medical Society for Sports Medicine, says that there is no one-size-fits-all exercise for people suffering from sciatic nerve pain. “Do you feel better when you bring your knees to the chest, or when they extend back a little more? If one feels better, that is the treatment you want to pursue.”
- Martinez – says that anyone experiencing even mild sciatic nerve pain symptoms for more than a month should see a doctor or physical therapist. They may find relief with an in-home exercise program tailored specifically to how their pain presents itself.
- What complications are associated with – Chronic (ongoing and lasting) pain is a complication of untreated sciatica. If the “pinched nerve” is seriously injured, chronic muscle weakness, such as a “drop foot,” might occur.
- What is the outlook for people with – Sciatic pain usually goes away with time and rest. Most people with sciatica (80 percent to 90 percent) will get better without surgery. About half of affected individuals recover from an episode within six weeks.
Can sciatica be prevented?
Some sources of sciatica are not preventable, such as degenerative disc disease, back strain due to pregnancy, and accidental falls.
- Although it might not be possible to prevent all cases of sciatica, you can take steps to protect your back and reduce your risk.
- Practice proper lifting techniques. Lift with your back straight, bringing yourself up with your hips and legs, and holding the object close to your chest. Use this technique for lifting everything, no matter how light.
Avoid/ stop cigarette smoking, which promotes disc degeneration.
Exercise regularly to strengthen the muscles of your back and abdomen, which work to
support your spine
- Use good posture when sitting, standing, and sleeping. Good posture helps to relieve the pressure on your lower back.
Avoid sitting for long periods.
Preventing Lumbago /Backache
Steps to lower the risk of developing back pain consist mainly of addressing some of the risk factors.
- Exercise – Regular exercise helps build strength as well as keeping your body weight down. Experts say that low-impact aerobic activities are best; activities that do not strain or jerk the back. Before starting any exercise program, talk to a health care professional. There are two main types of exercise that people can do to reduce the risk of back pain
- Core-strengthening exercises– exercises that work the abdominal and back muscles, helping to strengthen muscles that protect the back.
- Flexibility – exercises aimed at improving flexibility in your core, including your spine, hips, and upper legs, may help too.
- Smoking – a significantly higher percentage of smokers have back pain incidences compared to non-smokers of the same age, height, and weight.
- Bodyweight – the number of weight people carry, as well as where they carry it, affects the risk of developing back pain. The difference in back pain risk between obese and normal-weight individuals is considerable. People who carry their weight in the abdominal area versus the buttocks and hip area are also at greater risk.
- Posture when standing – make sure you have a neutral pelvic position. Stand upright, head facing forward, back straight, and balance your weight evenly on both feet – keep your legs straight and your head in line with your spine.

If you regularly use a computer, it is important to ensure that you have a chair with good back support and adopt a good posture and head position.
- Posture when sitting – a good seat should have good back support, armrests and a swivel base (for working). When sitting try to keep your knees and hips level and keep your feet flat on the floor – if you can’t, use a footstool. You should ideally be able to sit upright with support in the small of your back. If you are using a keyboard, make sure your elbows are at right-angles and that your forearms are horizontal.
- Lifting things – the secret for protecting your back when lifting things is to think “legs not back”. In other words, use your legs to do the lifting, more than your back. Keep your back as straight as you can, keeping your feet apart with one leg slightly forward so you can maintain balance. Bend only at the knees, hold the weight close to your body, and straighten the legs while changing the position of your back as little as possible. Bending your back initially is unavoidable, but when you bend your back try not to stoop or squat, and be sure to tighten your stomach muscles so that your pelvis is pulled in. Most importantly, do not straighten your legs before lifting; otherwise, you will be using your back for most of the work.
- Do not lift and twist at the same time. If something is particularly heavy, see if you can lift it with someone else. While you are lifting keep looking straight ahead, not up nor down, so that the back of your neck is like a continuous straight line from your spine.
- Moving things – remember that it is better for your back to push things across the floor, using your leg strength, rather than pulling them.
- Shoes – flat shoes place less of a strain on the back.
- Driving – it is important to have proper support for your back. Make sure the wing mirrors are properly positioned so you do not need to twist. The pedals should be squarely in front of your feet. If you are on a long journey, have plenty of breaks – get out of the car and walk around.
- Your bed – you should have a mattress that keeps your spine straight, while at the same time supporting the weight of your shoulders and buttocks. Use a pillow, but not one that forces your neck into a steep angle.
Home Remedies for Lumbago /Backache
Ice and Heat
Ice works wonders on lower back pain. Wrap some ice cubes in a plastic bag to prepare an ice pack. Then cover it with a towel and apply it to the painful area for 20 minutes. Repeat the same process several times a day. Then after 48 hours, you can switch to heat method. Dip a towel in warm water. Flatten and fold it on to the affected area. Place a heating pad on it with a plastic cover between towel and heating pad. Leave it for 20 minutes. Do it several times a day. It reduces swelling and relaxes the nerves that are responsible for sending pain signals to the brain.
Rest
Get sufficient rest. Don’t exhaust yourself physically and mentally. When sleeping, keep changing your positions. When you lie on back, put a pillow under your knees. Similarly, if you lie on your side, draw your knees near your chest and keep a pillow between your knees.
Right Posture
Your sitting and standing posture is very important to keep back pain at bay. One should not be in a bending position for a long time whether sitting or standing. Sitting on the edge of the chair and slouching should be avoided. The angle of the chair in office should be 110 degrees.
Lemon Juice
Lemon juice is an effective home remedy for back pain. Drink lemon juice twice a day for better results.
Poppy Seeds
Prepare a mixture of poppy seeds and rock candy by grinding together 100 gm of each. Take this mixture twice a day with a glass of milk. You will get relief from back pain.
Massage with Olive Oil
Massage with olive oil to reduce stress by relaxing tensed muscles. It also helps release stiffness in joints and relieves upper back pain.
Stretching
Stretching is the easiest back pain treatment. If your job demands sitting or standing for long hours, just take a break of 5 minutes every hour and walk or simply stretch your body to avoid back pain.
Wheat
Wheat has pain minimizing component in it. Mix cuscus grass and coriander with overnight soaked wheat. Add 1 cup of milk and bring it to boil. Consume this mixture twice a day
Garlic
Eat 2-3 garlic cloves on an empty stomach every morning to get relief from back pain. You can also use garlic oil. Massage your back with this oil, cover it with a warm blanket and lie on your back. Bathe using warm water after 20 minutes. This is a wonderful home remedy to treat back pain.
Ginger
The anti-inflammatory properties of ginger make it an ideal home remedy to get rid of back pain. Add ½ teaspoon of black peppercorns, ½ teaspoon of cloves and 1 teaspoon of ginger powder in a cup of boiling water to prepare herbal tea. Drink it 2-3 times a day.
- Alternatively, grate some ginger to prepare a paste. Apply it on the affected area. Then massage with eucalyptus oil.
- Put thin ginger slices in a pan of boiling water. Simmer it for 10-15 minutes. Strain and allow it to cool down at room temperature. Add honey to sweeten it. Drink it twice or thrice a day.
Milk
Since milk is a great source of calcium, it is extremely beneficial for strong bones and preventing back pain. People of every age group should consume milk. For quick relief, add a few drops of honey and a pinch of turmeric in the milk.
Epsom Salt
A natural healer, Epsom salt reduces swelling in the back. It contains magnesium and sulfate which help muscles function properly, thus, provide relief from pain. Add 2 cups of Epsom salt to a tub of warm water. Let it soak for 30 minutes. Take bath with this water.
Rice
Rice is easily available in every household. It’s an effective home remedy for back pain. Put 1 cup uncooked rice in a thick sock and place it in the microwave for ½ – 1 minute. Now apply it onto the back.
Oats
Mash cooked whole oats with vinegar. Apply it on the back when hot. It soothes the aching back.
Potatoes
Mash the peeled and boiled potatoes. Let them cool and then apply on back. You will experience relief from back pain.
Coconut Oil
Take some coconut oil. Mix camphor in it and boil for 5-7 minutes. Allow it to cool. Store it in a bottle. Massage with this oil two times a day to cure back pain.
Capsaicin Cream
Capsaicin is an important ingredient of chilies. Apply capsaicin cream on the back. It will reduce the production of chemicals that transmit signals of pain to your brain.
Herbal Remedies for Lumbago /Backache
Willow Bark
White willow tree’s bark is considered an excellent herbal remedy for treating back pain. It has pain-relieving properties the same as aspirin. So it will help reduce your back pain.
Basil Leaves
Basil leaves are very famous for their medicinal benefits. They aid in curing lower back pain. Boil 10-12 fresh basil leaves in a cup of water until it becomes half. Add a pinch of salt to it. Drink it once or twice a day depending on the severity of your pain.
Herbal Oils
Herbal oils like almond oil, eucalyptus oil, coconut oil or olive oil are very effective in alleviating back pain. Massage with warm oils on the painful area to relax the nerves causing pain.
Chamomile
Take some chamomile flowers. Steep them in a cup of boiling water for 15-20 minutes. Drink it 2-3 times a day. It will relax the tense muscles, thereby cure a backache.
Note: – Pregnant ladies and those allergic to chamomile flowers should first consult doctor before taking this.
Ginger
Though more studies are needed, says Dr. Kiefer, ginger extract may help with joint and muscle pain because it contains phytochemicals, which help stop inflammation. Few side effects have been linked to ginger when taken in small doses.
Feverfew
Feverfew has been used for centuries to treat headaches, stomachaches, and toothaches. Nowadays it’s also used for migraines and rheumatoid arthritis. More studies are required to confirm whether feverfew is actually effective, but the herb may be worth trying since it hasn’t been associated with serious side effects. Mild side effects include canker sores and irritation of the tongue and lips. Pregnant women should avoid this remedy.
Turmeric
This spice has been used to relieve arthritis pain and heartburn, and to reduce inflammation. It’s unclear how turmeric works against pain or inflammation, but its activity may be due to a chemical called curcumin, which has anti-inflammatory properties. Turmeric is usually safe to use, but high doses or long-term use may cause indigestion. Also, people with gallbladder disease should avoid using turmeric.
Homeopathic Medicines for Lumbago /Backache
Rhus Tox
Rhus Tox tops the list of Homeopathic medicines for back pain. I have seen magnificent results in back pain from the use of Rhus Tox. Rhus Tox is indicated for both upper and lower back pain, especially where the back pain is accompanied by intense stiffness. The back pain that arises from muscle strain also recovers wonderfully well with Rhus Tox. Persons suffering from back pain as a result of exertion or lifting heavy weights have found complete relief when prescribed Rhus Tox, making it one of the most reliable Homeopathic medicines for back pain. A prominent symptom to look out for while prescribing Rhus Tox is that the back pain gets worse with rest while walking or hard pressure brings relief from pain.
Bryonia
In my clinical practice, Bryonia has shown marvelous results in lower back pain that worsens with the slightest of movements. Apart from motion, this pain also gets worse with standing or from turning in the bed, a key sign that Bryonia will work best. The pain may be accompanied by marked stiffness in such cases, for which Bryonia would rate among the best Homeopathic medicines for back pain. Lying down and taking rest brings relief from pain.
Aesculus
Aesculus is one of the most effective Homeopathic medicines for lower back pain that gets worse from stooping. In this case, the pain is most marked in the sacrum and hip region. The lower back feels as if it would break. Stiffness in the lower back is also intense. Aesculus is also one of the best Homeopathic medicines for back pain which gets worse when rising from a sitting position. Here it takes the person repeated efforts to rise from a chair or another sitting position.
Kali Carb
I would rank Kali Carb as one of the top grade Homeopathic medicines for back pain that arises after childbirth. The most prominent symptoms indicative of Kali Carb as the best suited Homeopathic medicines for back pain in such instances are stiffness and weakness in the lower back. The pain is very severe, with a feeling that the back might break. The back pain makes it difficult to walk. Women feel the need to lie down to get relief from the pain which may radiate to the upper back or down to the thigh and hips. Where these symptoms exist, Kali Carb comes highly recommended as one of the best Homeopathic medicines for back pain. Apart from a post-partum backache, Kali Carb is also useful for backache in women before or during menses and after a miscarriage.
Cobalt
Cobalt ranks on top of the list of Homeopathic medicines for back pain that worsens from sitting. In such cases, the person feels better while walking or lying down. The back pain may radiate down the legs and feet in some cases, but the person will surely feel a weakness in the legs, a sure sign that Cobaltum will provide sustained relief.
Colocynth & Magnesium Phos
I have successfully treated several cases of back pain radiating down the legs and/or feet with two main Homeopathic medicines. These top-rated Homeopathic medicines for back pain are Colocynth and Magnesium Phos. Among these, Colocynth is most effective Homeopathic medicine for back pain when the lower back pain radiates to the left leg and foot. Magnesium Phos brings relief when the lower back pain radiates down the right leg. The pain, in both cases, can be of a shooting, cramping or tearing nature. However, both the medicines have proven their ability to bring lasting relief from pain and established themselves as the best Homeopathic medicines for back pain.
Cimicifuga & Kalmia
Two highly recommended Homeopathic medicines for back pain in the cervical region are Cimicifuga and Kalmia. I have seen remarkable results with the use of Cimicifuga in cervical back pain accompanied by stiffness, contraction, and sensitiveness in the neck. If pressure worsens the neck pain, Cimicifuga will offer effective treatment. However, in cases where the cervical pain radiates down the arm or hands, Kalmia has proved to be one of the most helpful Homeopathic medicines for back pain treatment. Persons feeling a weakness, numbness or tingling sensation in the arms and hands along with neck pain also recover fully well with the use of Homeopathic medicine Kalmia.
Ruta & Hypericum
Ruta and Hypericum are highly suitable Homeopathic medicines for back pain resulting from the injury. Ruta is prescribed for a back that is sore and bruised from injury. The pain is most marked over the sacrum and coccyx region. The injured person may feel a weakness in the lower back. Where such symptoms are noted, Ruta is the most prominent among Homeopathic medicines for back pain and has shown effective results. Homeopathic medicine Hypericum is recommended when the pain from the tailbone radiates up the spine and down the limbs after injury. The pain is very sharp and intense. Motion, walking and stooping all make the pain worse. The spine is very tender and sensitive to touch in such cases where Hypericum has shown the best results.
References



Visitor Rating: 5 Stars
Visitor Rating: 5 Stars