Vitamin D Food Source/Vitamin D is a group of fat-soluble secosteroids responsible for increasing intestinal absorption of calcium, magnesium, and phosphate, and multiple other biological effects. In humans, the most important compounds in this group are vitamin D3 (also known as cholecalciferol) and vitamin D2 (ergocalciferol). Cholecalciferol and ergocalciferol can be ingested from the diet and from supplements. Only a few foods contain vitamin D. The major natural source of the vitamin is a synthesis of cholecalciferol in the skin from cholesterol through a chemical reaction that is dependent on sun exposure (specifically UVB radiation).
Vitamin D promotes calcium absorption in the gut and maintains adequate serum calcium and phosphate concentrations to enable normal mineralization of bone and to prevent hypocalcemic tetany. It is also needed for bone growth and bone remodeling by osteoblasts and osteoclasts. Without sufficient vitamin D, bones can become thin, brittle, or misshapen. Vitamin D sufficiency prevents rickets in children and osteomalacia in adults. Together with calcium, vitamin D also helps protect older adults from osteoporosis.
Types of Vitamin D
| Name | Chemical composition | Structure |
|---|---|---|
| Vitamin D1 | Mixture of molecular compounds of ergocalciferol with lumisterol, | |
| Vitamin D2 | ergocalciferol (made from ergosterol) | |
| Vitamin D3 | cholecalciferol (made from 7-dehydrocholesterol in the skin). | |
| Vitamin D4 | 22-dihydroergocalciferol | |
| Vitamin D5 | sitocalciferol (made from 7-dehydrositosterol) |
Noncalcemic benefits of vitamin D
ESCP recommends prescribing vitamin D supplementation for fall prevention and do not recommend supplementation beyond recommended daily needs for the purpose of preventing cardiovascular disease or death or improving quality of life.[rx]
Vitamin D analogs
Vitamin D has five natural analogs, called vitamers, and four synthetic analogs which are made synthetically. Vitamin D analogs are chemically classified as secosteroids, which are steroids with one broken bond.
Natural analogs of vitamin D
- Vitamin D1 – is a molecular compound of ergocalciferol (D2) with lumisterol in a 1:1 ratio.
- Vitamin D2 (ergocalciferol) – is produced by invertebrates, some plants, and fungi. Biological production of D2 is stimulated by ultraviolet light.
- Vitamin D3 (cholecalciferol) – is synthesized in the skin by the reaction of 7-dehydrocholesterol with UVB radiation, present in sunlight with an UV index of three or more
- Vitamin D4 – is an analog scientifically known as 22-dihydroergocalciferol.
- Vitamin D5 (sitocalciferol) – is an analog created from 7-dehydrositosterol.
Synthetic analogs of vitamin D
- Maxacalcitol (22-oxacalcitriol or OCT)- is the first analog found to have a wider therapeutic window than 1,25(OH)2D3.[rx]
- Calcipotriol – is derived from calcitriol was first discovered during trials involving the use of vitamin D for treating osteoporosis.
- Dihydrotachysterol (DHT) – is a synthetic form of vitamin D that many consider superior to natural D2and D3. It becomes active by the liver without needing to go through hydroxylation in the kidneys.
- Paricalcitol (19-norD2) – is also derived from calcitriol. It is the first of the new vitamin D analogs to be approved for secondary hyperparathyroidism and differs from calcitriol in that it lacks the exocyclic carbon 19 and has a vitamin D2 side chain instead of a vitamin D3 side chain.[rx]
- Tacalcitol is a derivative of vitamin D3 – It is known to hinder keratinocytes in the skin.
- Doxercalciferol (1α(OH)D2) – is a prodrug and must be activated in vivo. It is less toxic than 1α (OH)D3[1rx] when administered chronically.
- Falecalcitriol (1,25(OH) 2-26, 27-F6-D3) – is approved for secondary hyperparathyroidism in Japan.[rx] It is more active than calcitriol because of its slower metabolism.[rx]
Vitamin D deficiency is typically diagnosed by measuring the concentration of the 25-hydroxyvitamin D in the blood, which is the most accurate measure of stores of vitamin D in the body.
- Deficiency: <20 ng/mL
- Insufficient: 20–29 ng/mL
- Normal: 30–100 ng/mL
Vitamin D levels falling within this normal range prevent clinical manifestations of vitamin D insufficiency as well as vitamin D toxicity from taking in too much vitamin D. Several forms (vitamers) of vitamin D exist. The two major forms are vitamin D2 or ergocalciferol, and vitamin D3 or cholecalciferol; vitamin D without a subscript refers to either D2 or D3 or both. These are known collectively as calciferol. Vitamin D2 was chemically characterized in 1931. In 1935, the chemical structure of vitamin D3 was established and proven to result from the ultraviolet irradiation of 7-dehydrocholesterol.
Chemically, the various forms of vitamin D are secosteroids, i.e., steroids in which one of the bonds in the steroid rings is broken. The structural difference between vitamin D2 and vitamin D3 is the side chain of D2 contains a double bond between carbons 22 and 23, and a methyl group on carbon 24.
Biology of the Sunshine Vitamin
Vitamin D is unique because it can be made in the skin from exposure to sunlight.[rx,rx–rx] Vitamin D exists in two forms. Vitamin D2 is obtained from the UV irradiation of the yeast sterol ergosterol and is found naturally in sun-exposed mushrooms. UVB light from the sun strikes the skin, and humans synthesize vitamin D3, so it is the most “natural” form. Human beings do not make vitamin D2, and most oil-rich fish such as salmon, mackerel, and herring contain vitamin D3. Vitamin D (D represents D2, or D3, or both) that is ingested is incorporated into chylomicrons, which are absorbed into the lymphatic system and enter the venous blood. Vitamin D that comes from the skin or diet is biologically inert and requires its first hydroxylation in the liver by the vitamin D-25-hydroxylase (25-OHase) to 25(OH)D.[rx,rx] However, 25(OH)D requires a further hydroxylation in the kidneys by the 25(OH)D-1-OHase (CYP27B1) to form the biologically active form of vitamin D 1,25(OH)2D.[rx,rx] 1,25(OH)2D stimulates intestinal calcium absorption.[rx] Without vitamin D, only 10–15% of dietary calcium and about 60% of phosphorus are absorbed. Vitamin D sufficiency enhances calcium and phosphorus absorption by 30–40% and 80%, respectively.[rx,rx]
Vitamin D receptor (VDR) is present in most tissues and cells in the body.[rx,rx] 1,25(OH)2D has a wide range of biological actions, such as inhibition of cellular proliferation and inducing terminal differentiation, inhibiting angiogenesis, stimulating insulin production, inhibiting renin production, and stimulating macrophage cathelicidin production.[rx,rx–rx] The local production of 1,25(OH)2D may be responsible for regulating up to 200 genes[rx] that may facilitate many of the pleiotropic health benefits that have been reported for vitamin D.[rx,rx,rx,rx]
Deficiency Symptoms of Vitamin D
Vitamin D deficiency can be asymptomatic, but may also cause several problems including:
- Osteomalacia – a bone-thinning disorder that occurs exclusively in adults and is characterized by proximal muscle weakness and bone fragility.
- Osteoporosis – a condition characterized by reduced bone mineral density and increased bone fragility.
- Increased risk of fracture
- Rickets – a childhood disease characterized by impeded growth and deformity of the long bones. The earliest sign of subclinical vitamin D deficiency is craniotabes, abnormal softening or thinning of the skull.
- Muscle aches and weakness
- Muscle twitching – (fasciculations) is commonly seen due to reduced ionized calcium, arising from a low vitamin D.
- Light-headedness
- Periodontitis – a local inflammatory bone loss that can result in tooth loss.
- Pre-eclampsia – There has been an association of vitamin D deficiency and women who develop pre-eclampsia in pregnancy. The exact relationship of these conditions is not well understood. Maternal vitamin D deficiency may affect the baby, causing overt bone disease from before birth and impairment of bone quality after birth.
- Depression – Hypovitaminosis D is a risk factor for depression. Some studies have found that low levels of vitamin D are correlated with depressed feelings and are found in patients who have been diagnosed with depression.
Symptoms of vitamin D deficiency may include
- Getting sick or infected more often.
- Fatigue.
- Painful bones and back.
- Depressed mood.
- Impaired wound healing.
- Hair loss.
- Muscle pain.
- obesity
- diabetes
- hypertension
- depression
- fibromyalgia
- chronic fatigue syndrome
- osteoporosis
- neurodegenerative diseases, such as Alzheimer’s disease
Reference Intakes of Vitamin D
Intake reference values for vitamin D and other nutrients are provided in the Dietary Reference Intakes (DRIs) developed by the Food and Nutrition Board (FNB) at the Institute of Medicine of The National Academies (formerly National Academy of Sciences). DRI is the general term for a set of reference values used to plan and assess the nutrient intakes of healthy people. These values, which vary by age and gender, include:
- Recommended Dietary Allowance (RDA) – Average daily level of intake sufficient to meet the nutrient requirements of nearly all (97%–98%) healthy individuals; often used to plan nutritionally adequate diets for individuals.
- Adequate Intake (AI) – Intake at this level is assumed to ensure nutritional adequacy; established when evidence is insufficient to develop an RDA.
- Estimated Average Requirement (EAR) – Average daily level of intake estimated to meet the requirements of 50% of healthy individuals; usually used to assess the nutrient intakes of groups of people and to plan nutritionally adequate diets for them; can also be used to assess the nutrient intakes of individuals.
- Tolerable Upper Intake Level (UL) – Maximum daily intake unlikely to cause adverse health effects.
The FNB established an RDA for vitamin D representing a daily intake that is sufficient to maintain bone health and normal calcium metabolism in healthy people. RDAs for vitamin D are listed in both International Units (IUs) and micrograms (mcg); the biological activity of 40 IU is equal to 1 mcg. Even though sunlight may be a major source of vitamin D for some, the vitamin D RDAs are set on the basis of minimal sun exposure.
[dropshadowbox align=”none” effect=”lifted-both” width=”auto” height=”” background_color=”#ffffff” border_width=”3″ border_color=”#dddddd” ]
| Age | Male | Female | Pregnancy | Lactation |
|---|---|---|---|---|
| 0–12 months* | 400 IU (10 mcg) |
400 IU (10 mcg) |
||
| 1–13 years | 600 IU (15 mcg) |
600 IU (15 mcg) |
||
| 14–18 years | 600 IU (15 mcg) |
600 IU (15 mcg) |
600 IU (15 mcg) |
600 IU (15 mcg) |
| 19–50 years | 600 IU (15 mcg) |
600 IU (15 mcg) |
600 IU (15 mcg) |
600 IU (15 mcg) |
| 51–70 years | 600 IU (15 mcg) |
600 IU (15 mcg) |
||
| >70 years | 800 IU (20 mcg) |
800 IU (20 mcg) |
* Adequate Intake (AI)
Recommended levels
| United States | ||
| Age group | RDA (IU/day) | (μg/day) |
|---|---|---|
| Infants 0–6 months | 400* | 10 |
| Infants 6–12 months | 400* | 10 |
| 1–70 years | 600 | 15 |
| 71+ years | 800 | 20 |
| Pregnant/Lactating | 600 | 15 |
| Age group | Tolerable upper intake level (IU/day) | (µg/day) |
| Infants 0–6 months | 1,000 | 25 |
| Infants 6–12 months | 1,500 | 37.5 |
| 1–3 years | 2,500 | 62.5 |
| 4–8 years | 3,000 | 75 |
| 9+ years | 4,000 | 100 |
| Pregnant/lactating | 4,000 | 100 |
| Canada | ||
| Age group | RDA (IU) | Tolerable upper intake (IU) |
| Infants 0–6 months | 400* | 1,000 |
| Infants 7–12 months | 400* | 1,500 |
| Children 1–3 years | 600 | 2,500 |
| Children 4–8 years | 600 | 3,000 |
| Children and Adults 9–70 years | 600 | 4,000 |
| Adults > 70 years | 800 | 4,000 |
| Pregnancy & Lactation | 600 | 4,000 |
| Australia and New Zealand | ||
| Age group | Adequate Intake (μg) | Upper Level of Intake (μg) |
| Infants 0–12 months | 5* | 25 |
| Children 1–18 years | 5* | 80 |
| Adults 19–50 years | 5* | 80 |
| Adults 51–70 years | 10* | 80 |
| Adults > 70 years | 15* | 80 |
| European Food Safety Authority | ||
| Age group | Adequate Intake (μg) | Tolerable upper limit (μg) |
| Infants 0–12 months | 10 | 25 |
| Children 1–10 years | 15 | 50 |
| Children 11–17 years | 15 | 100 |
| Adults | 15 | 100 |
| Pregnancy & Lactation | 15 | 100 |
| * Adequate intake, no RDA/RDI yet established | ||
Several food sources of vitamin D are listed in Table 3.
| Food | IUs per serving* | Percent DV** |
|---|---|---|
| Cod liver oil, 1 tablespoon | 1,360 | 340 |
| Swordfish, cooked, 3 ounces | 566 | 142 |
| Salmon (sockeye), cooked, 3 ounces | 447 | 112 |
| Tuna fish, canned in water, drained, 3 ounces | 154 | 39 |
| Orange juice fortified with vitamin D, 1 cup (check product labels, as amount of added vitamin D varies) | 137 | 34 |
| Milk, nonfat, reduced fat, and whole, vitamin D-fortified, 1 cup | 115-124 | 29-31 |
| Yogurt, fortified with 20% of the DV for vitamin D, 6 ounces (more heavily fortified yogurts provide more of the DV) | 80 | 20 |
| Margarine, fortified, 1 tablespoon | 60 | 15 |
| Sardines, canned in oil, drained, 2 sardines | 46 | 12 |
| Liver, beef, cooked, 3 ounces | 42 | 11 |
| Egg, 1 large (vitamin D is found in yolk) | 41 | 10 |
| Ready-to-eat cereal, fortified with 10% of the DV for vitamin D, 0.75-1 cup (more heavily fortified cereals might provide more of the DV) | 40 | 10 |
| Cheese, Swiss, 1 ounce | 6 | 2 |
* IUs = International Units.
** DV = Daily Value. DVs were developed by the U.S. Food and Drug Administration to help consumers compare the nutrient contents among products within the context of a total daily diet. The DV for vitamin D is currently set at 400 IU for adults and children age 4 and older. Food labels, however, are not required to list vitamin D content unless a food has been fortified with this nutrient. Foods providing 20% or more of the DV are considered to be high sources of a nutrient, but foods providing lower percentages of the DV also contribute to a healthful diet.
Natural Sources of Vitamin D
Sources of vitamin D
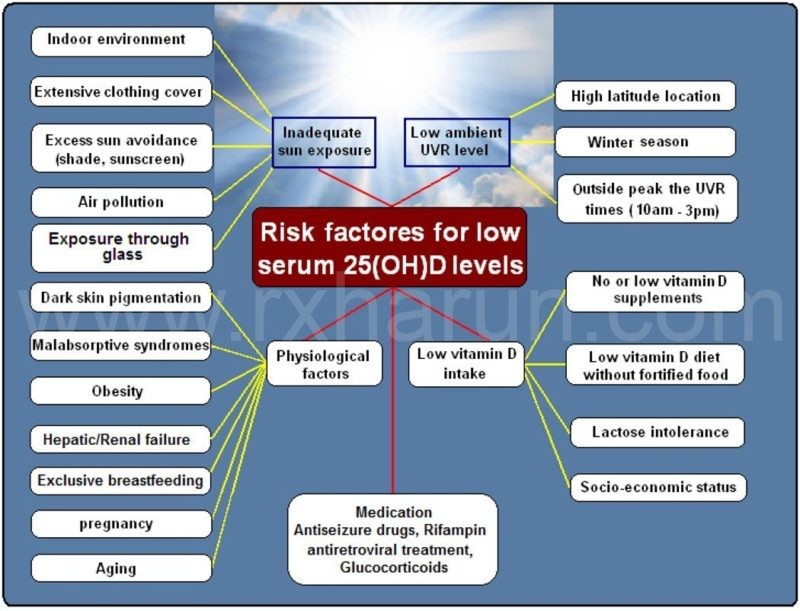
A major source of vitamin D for most humans is synthesized from the exposure of the skin to sunlight typically between 1000 h and 1500 h in the spring, summer, and fall.[rx,rx,rx,rx] Vitamin D produced in the skin may last at least twice as long in the blood compared with ingested vitamin D.[rx] When an adult wearing a bathing suit is exposed to one minimal erythemal dose of UV radiation (a slight pinkness to the skin 24 h after exposure), the amount of vitamin D produced is equivalent to ingesting between 10,000 and 25,000 IU.[rx] A variety of factors reduce the skin’s production of vitamin D3, including increased skin pigmentation, aging, and the topical application of sunscreen.[rx,rx,rx] An alteration in the zenith angle of the sun caused by a change in latitude, the season of the year, or time of day dramatically influences the skin’s production of vitamin D3.[rx,rx]
Physiological Actions of Vitamin D
Vitamin D is a fat-soluble vitamin that acts as a steroid hormone. In humans, the primary source of vitamin D is UVB-induced conversion of 7-dehydrocholesterol to vitamin D in the skin [.[rx,rx] Vitamin D influences the bones, intestines, immune and cardiovascular systems, pancreas, muscles, brain, and the control of cell cycles.[rx]
In general, vitamin D2 is found in fungi and vitamin D3 is found in animals. Vitamin D2 is produced by ultraviolet irradiation of ergosterol found in many fungi. The vitamin D2content in mushrooms and Cladina arbuscula, a lichen, increase with exposure to ultraviolet light. This process is emulated by industrial ultraviolet lamps, concentrating vitamin D2levels to higher levels.
The United States Department of Agriculture reports D2 and D3 content combined in one value
Fungal sources
- C. arbuscula (lichen), thalli, dry: vitamin D3 0.67 to 2.04 μg/g (27 to 82 IU/g); vitamin D2 0.22-0.55 μg/g (8.8 to 22 IU/g).
Agaricus bisporus – (common mushroom), D2 + D3, per 100 grams (3.5 oz):
- raw portobello: 0.3 μg (10 IU); exposed to ultraviolet light: 11.2 µg (446 IU)
- raw crimini: 0.1 μg (3 IU); exposed to ultraviolet light: 31.9 µg (1276 IU)
Animal sources
- Fish liver oils, such as cod liver oil, 450 IU per teaspoon (4.5 g); (100 IU/g)
Fatty fish species, such as
- Salmon, pink, cooked, dry heat, 100 grams (3.5 oz): 522 IU (5.2 IU/g)
- Mackerel, Pacific and jack, mixed species, cooked, dry heat, 100 grams (3.5 oz): 457 IU (4.6 IU/g)
- Tuna, canned in oil, 100 grams (3.5 oz): 269 IU (2.7 IU/g)
- Sardines, canned in oil, drained, 100 grams (3.5 oz): 193 IU (1.9 IU/g)
- Cooked egg yolk: 44 IU for a 61 g egg (0.7 IU/g)
- Beef liver, cooked, braised, 100 grams (3.5 oz): 49 IU (0.5 IU/g)
| Age | Male | Female | Pregnancy | Lactation |
|---|---|---|---|---|
| 0–6 months | 1,000 IU (25 mcg) |
1,000 IU (25 mcg) |
||
| 7–12 months | 1,500 IU (38 mcg) |
1,500 IU (38 mcg) |
||
| 1–3 years | 2,500 IU (63 mcg) |
2,500 IU (63 mcg) |
||
| 4–8 years | 3,000 IU (75 mcg) |
3,000 IU (75 mcg) |
||
| 9–18 years | 4,000 IU (100 mcg) |
4,000 IU (100 mcg) |
4,000 IU (100 mcg) |
4,000 IU (100 mcg) |
| 19+ years | 4,000 IU (100 mcg) |
4,000 IU (100 mcg) |
4,000 IU (100 mcg) |
4,000 IU (100 mcg) |
[/dropshadowbox]
Interactions with Medications of Vitamin D
Vitamin D supplements have the potential to interact with several types of medications. A few examples are provided below. Individuals taking these medications on a regular basis should discuss vitamin D intakes with their healthcare providers.
Steroids
Corticosteroid medications such as prednisone, often prescribed to reduce inflammation, can reduce calcium absorption and impair vitamin D metabolism. These effects can further contribute to the loss of bone and the development of osteoporosis associated with their long-term use.
Other medications
Both the weight-loss drug orlistat and the cholesterol-lowering drug cholestyramine can reduce the absorption of vitamin D and other fat-soluble vitamins. Both phenobarbital and phenytoin used to prevent and control epileptic seizures, increase the hepatic metabolism of vitamin D to inactive compounds and reduce calcium absorption.
Vitamin D and Healthful Diets
The federal government’s 2015-2020 Dietary Guidelines for Americans notes that “Nutritional needs should be met primarily from foods. … Foods in nutrient-dense forms contain essential vitamins and minerals and also dietary fiber and other naturally occurring substances that may have positive health effects. In some cases, fortified foods and dietary supplements may be useful in providing one or more nutrients that otherwise may be consumed in less-than-recommended amounts.”
For more information about building a healthy diet, refer to the Dietary Guidelines for Americans and the U.S. Department of Agriculture’s MyPlate.
The Dietary Guidelines for Americans describes a healthy eating pattern as one that
- Includes a variety of vegetables, fruits, whole grains, fat-free or low-fat milk and milk products, and oils.
- Milk is fortified with vitamin D, as are many ready-to-eat cereals and some brands of yogurt and orange juice. Cheese naturally contains small amounts of vitamin D.
- Includes a variety of protein foods, including seafood, lean meats and poultry, eggs, legumes (beans and peas), nuts, seeds, and soy products.
- Fatty fish such as salmon, tuna, and mackerel are very good sources of vitamin D. Small amounts of vitamin D are also found in beef liver and egg yolks.
- Limits saturated and trans fats, added sugars, and sodium.
- Vitamin D is added to some margarines.
- Stays within your daily calorie needs.
Dosing
- Only a few foods are a good source of vitamin D. The best way to get additional vitamin D is through supplementation. Traditional multivitamins contain about 400 IU of vitamin D, but many multivitamins now contain 800 to 1000 IU. A variety of options are available for individual vitamin D supplements, including capsules, chewable tablets, liquids, and drops. Cod liver oil is a good source of vitamin D, but in large doses there is a risk of vitamin A toxicity.[rx]
Indications / Uses of Vitamin D
Effective for
- Low levels of phosphate in the blood due to an inherited disorder called familial hypophosphatemia – Taking vitamin D (calcitriol or dihydrotachysterol) by mouth along with phosphate supplements is effective for treating bone disorders in people with low levels of phosphate in the blood.
- Low levels of phosphate in the blood due to a disease called Fanconi syndrome – Taking vitamin D (ergocalciferol) by mouth is effective for treating low levels of phosphate in the blood due to a disease called Fanconi syndrome.
- Low blood calcium levels due to low parathyroid hormone levels – Low levels of parathyroid hormone can cause calcium levels to become too low. Taking vitamin D (dihydrotachysterol, calcitriol, or ergocalciferol) by mouth is effective for increasing calcium blood levels in people with low parathyroid hormone levels.
- Softening of the bones (osteomalacia) – Taking vitamin D (cholecalciferol) is effective for treating softening of the bones. Also, taking vitamin D (calcifediol) is effective for treating softening of the bones due to liver disease. In addition, taking vitamin D (ergocalciferol) is effective for treating softening of the bones caused by medications or poor absorption syndromes.
- Psoriasis – Applying vitamin D or calcipotriene (a synthetic form of vitamin D) to the skin treats psoriasis in some people. Applying vitamin D to the skin together with cream containing drugs called corticosteroids seems to be more effective for treating psoriasis than using just vitamin D or the corticosteroid creams alone.
- A bone disorder called renal osteodystrophy, which occurs in people with kidney failure – Taking vitamin D (calcifediol) by mouth manages low calcium levels and prevents bone loss in people with kidney failure. However, vitamin D does not appear to reduce the risk of death or bone pain in people with kidney failure.
- Rickets – Vitamin D is effective for preventing and treating rickets. A specific form of vitamin D, calcitriol, should be used in people with kidney failure.
- Vitamin D deficiency – Vitamin D is effective for preventing and treating vitamin D deficiency.
Likely Effective for
- Bone loss in people taking drugs called corticosteroids – Taking vitamin D (calcifediol, cholecalciferol, calcitriol, or alfacalcidol) by mouth prevents bone loss in people taking drugs called corticosteroids. Taking vitamin D alone or with calcium seems to improve bone density in people with existing bone loss caused by using corticosteroids.
- Preventing falls in older people – Researchers have observed that people who do not have enough vitamin D tend to fall more often than people who do. Taking a vitamin D supplement seems to reduce the risk of falling by up to 22%. Higher doses of vitamin D are more effective than lower doses. One study found that taking 800 IU of vitamin D reduced the risk of falling, but lower doses did not.
- Also, vitamin D, in combination with calcium, but not calcium alone, may prevent falls by decreasing body sway and blood pressure – Taking vitamin D plus calcium seems to prevent falls more significantly in women than men and in older people living in hospitals or residential care facilities than those living in community dwellings.
- Osteoporosis (weak bones) – Taking a specific form of vitamin D called cholecalciferol (vitamin D3) along with calcium seems to help prevent bone loss and bone breaks.
Possibly Effective for
- Cavities – Analysis of clinical research suggests that taking vitamin D in forms known as cholecalciferol or ergocalciferol reduces the risk of cavities by 36% to 49% in infants, children and adolescents.
- Heart failure – Some early research suggests that people with low vitamin D levels have an increased risk of developing heart failure compared to those with higher vitamin D levels. Also, most research suggests that taking vitamin D supplements, including vitamin D in a form known as cholecalciferol, may decrease the risk of death in people with heart failure.
- Bone loss caused by having too much parathyroid hormone (hyperparathyroidism) – Taking vitamin D in a form known as cholecalciferol by mouth seems to reduce parathyroid hormone levels and bone loss in women with a condition called hyperparathyroidism.
- Multiple sclerosis (MS) – Early research shows that taking vitamin D long-term can reduce the risk of developing MS in women by up to 40%. Taking at least 400 IU daily, the amount typically found in a multivitamin supplement, seems to work the best.
- Respiratory infections – Most research shows that taking vitamin D helps prevent respiratory infections in children and adults. A respiratory infection can be the flu, a cold, or an asthma attack triggered by a cold or other infection. Some research shows that taking vitamin D during pregnancy reduces the risk of these infections in the child after birth. But conflicting results exist.
- Tooth loss – Taking calcium and vitamin D in a form known as cholecalciferol by mouth appears to prevent tooth loss in elderly people.
Possibly Ineffective for
- Breast cancer – Evidence on the effects of vitamin D on breast cancer risk is not clear. The best evidence comes from a large study called the Women’s Health Initiative, which found that taking 400 IU of vitamin D and 1000 mg of calcium per day does not lower the chance of getting breast cancer when taken by postmenopausal women. However, the possibility remains that high doses of vitamin D might lower breast cancer risk in younger women.
- Cancer – Although some research shows that people who take a high-dose of vitamin D have a lower risk of developing cancer, most research does not support this.
- Heart disease – Early research suggests that people with low levels of vitamin D in their blood are more likely to develop heart disease, including heart failure, than people with higher vitamin D levels. However, taking vitamin D does not seem to extend the life of people with heart disease.
- Fractures Vitamin D doesn’t seem to prevent fractures in older people when used alone or in low doses with calcium. Vitamin D also doesn’t seem to prevent fractures in older people who still live in the community when used in higher doses with calcium. But it might help prevent fractures in older people living in a nursing home.
- High blood pressure – Early research suggests that people with low blood levels of vitamin D have a higher risk of developing high blood pressure than people with normal blood levels of vitamin D. However, most research suggests that taking vitamin D does not reduce blood pressure in people with high blood pressure.
- Bone loss in people with kidney transplants – Taking vitamin D in a form known as calcitriol by mouth along with calcium does not decrease bone loss in people with kidney transplants.
- Tuberculosis. Taking vitamin D by mouth does not appear to help cure tuberculosis infections.
Insufficient Evidence for
- Alzheimer’s disease – Early research suggests that people with Alzheimer’s disease have lower blood levels of vitamin D than patients without Alzheimer’s disease. It’s not clear if taking vitamin D benefits people with Alzheimer’s disease.
- Asthma – People with asthma and low blood levels of vitamin D seem to need to use an inhaler more often and have a higher risk of asthma complications. However, the role of vitamin D supplements in treating asthma is unclear. Best evidence to date shows that taking vitamin D by mouth for up to one year can reduce the rate of severe asthma attacks by about 31% to 36% in adults and children with asthma. But it’s still too soon to know which, if any, people with asthma are most likely to respond to treatment with vitamin D.
- Overgrowth of bacteria in the vagina (bacterial vaginosis) – Early research suggests that taking vitamin D does not prevent bacterial vaginosis in women at high risk for sexually transmitted disease when taken along with standard therapy.
- Kidney disease – Research suggests that vitamin D decreases parathyroid hormone levels in people with chronic kidney disease. However, taking vitamin D does not appear to lower the risk of death in people with kidney disease. Also taking vitamin D might increase calcium and phosphate levels in people with kidney disease.
- Chronic obstructive pulmonary disease (COPD) – People with COPD seem to have lower vitamin D levels that people without COPD. But there is not enough information to know if taking a vitamin D supplement can decrease symptoms of COPD.
- Mental function – Early research shows low vitamin D levels are linked to worse mental performance compared to high vitamin D levels. However, it’s not clear if taking vitamin D can improve mental function.
- Colorectal cancer – It is not clear if vitamin D might benefit colorectal cancer. Some research shows that vitamin D might be an important factor in developing colorectal cancer. But other research shows that taking vitamin D with calcium doesn’t lower the risk of colorectal cancer.
- Critical illness requiring intensive care in the hospital – Early research shows that giving vitamin D to people who are hospitalized in an intensive care unit with a critical illness might improve survival. The benefit of vitamin D might be limited to those people with very low vitamin D levels. More research is needed.
- Dementia – Early research suggests that people with dementia have lower blood levels of vitamin D than people without dementia. However, it’s not known if taking vitamin D benefits people with dementia.
- Diabetes – Early research shows that people with lower vitamin D levels may be more likely to develop type 2 diabetes compared to people with higher vitamin D levels. However, evidence is unclear if taking vitamin D supplements can treat or prevent type 2 diabetes. Early research suggests that giving vitamin D supplements to infants daily during the first year of life is linked to a lower risk of developing type 1 diabetes later in life.
- Preventing falls in older people – The role of vitamin D for fall prevention is confusing and controversial. Clinical practice guidelines published in 2010 recommend that elderly people who have low levels of vitamin D or who are at an increased risk of falling take 800 IU of vitamin D per day to reduce the risk of falling.
- A condition of chronic pain called fibromyalgia – Early research suggests that taking vitamin D might decrease pain in people with fibromyalgia and low vitamin D levels in the blood. However, taking vitamin D does not seem to help mood or quality of life.
- High cholesterol – People with lower vitamin D levels seem to be more likely to have high cholesterol than people with higher vitamin D levels. Limited research shows that taking calcium plus vitamin D daily, in combination with a low-calorie diet, significantly raises “good”(HDL) cholesterol and lowers “bad”(LDL) cholesterol in overweight women. However, taking calcium plus vitamin D without dietary restrictions does not reduce LDL cholesterol levels. Other research suggests that vitamin D might actually increase LDL and have no beneficial effect on HDL, triglycerides, or total cholesterol.
- Low birth weight – The effect of taking vitamin D during pregnancy on the risk of low birth weight or small gestational age birth is inconsistent. Additional studies are needed to determine who might benefit, if any, and what dose or formulation of vitamin D is optimal to prevent low weight at birth.
- Metabolic syndrome – There is conflicting evidence about the link between vitamin D and metabolic syndrome. Some research suggests that women aged at least 45 years who consume high amounts of vitamin D or take vitamin D supplements do not have a lower risk of developing metabolic syndrome. However, other research suggests that higher vitamin D levels are linked to a lower risk of metabolic syndrome.
- Muscle strength – Taking vitamin D by mouth does not appear to improve muscle strength in people with sufficient blood levels of vitamin D. However, taking vitamin D by mouth, alone or in combination with calcium, may improve hip and leg muscle strength in people who have low levels of vitamin D, especially the elderly. Single injections of vitamin D do not seem to have beneficial effects.
- A blood cell disease called myelodysplastic syndrome – Taking vitamin D in forms known as calcitriol or calcifediol by mouth seems to help people with myelodysplastic syndrome.
- Overall death risk – Early research suggests that having low vitamin D levels is linked with an increased risk of death from any cause. Some research suggests that people who take vitamin D supplements daily have a lower risk of dying. However, other research suggests that vitamin D reduces the risk of death only when taking together with calcium.
- Gum disease – Early research suggests that higher blood levels of vitamin D are linked with a reduced risk of gum disease in people 50 years of age or older. However, this does not seem to be true for adults younger than 50 years. It is not known if taking vitamin D supplements reduces the risk of gum disease.
- Pain – Early research shows that taking vitamin D might reduce pain in people with long-term pain. More research is needed to confirm these results.
- Parkinson’s disease – Higher levels of vitamin D have been linked to milder symptoms of Parkinson’s disease. But taking vitamin D supplements doesn’t seem to improve Parkinson’s disease symptoms, although it might help prevent the disease from worsening. More studies are needed.
- Pregnancy-associated complications Some research shows that taking vitamin D during pregnancy might lower the chance of preterm birth. But these studies were low quality. Taking vitamin D during pregnancy might reduce the risk of developing diabetes during pregnancy. Taking vitamin D doesn’t seem to prevent pre-eclampsia or pregnancy-related high blood pressure.
- Cysts on ovaries or polycystic ovary syndrome (PCOS) – Early research shows that taking vitamin D might improve ovulation in women with PCOS. Vitamin D taken together with metformin might improve menstrual cycle regularity but not when vitamin D is taken by itself.
- Premenstrual syndrome (PMS) – Some early research suggests that consuming more vitamin D from the diet might help to prevent PMS or reduce symptoms. Taking vitamin D supplements does not seem to prevent PMS. However taking vitamin D plus calcium might reduce PMS symptoms.
- A muscle disease called proximal myopathy – Taking vitamin D in a form known as ergocalciferol by mouth or administering it as a shot into the muscle seems to help treat a muscle disease associated with vitamin D deficiency.
- Rheumatoid arthritis (RA) – Early research suggests that older women who consume more vitamin D from foods or supplements have a lower risk of developing rheumatoid arthritis.
- Seasonal depression (seasonal affective disorder) – Early research suggests that taking a large dose of vitamin D in a form known as ergocalciferol improves symptoms of seasonal depression.
- Non-cancerous wart-like growths on the skin (seborrheic keratosis) – Early research suggests that applying vitamin D in a form known as cholecalciferol to the skin might reduce tumor size in some people with seborrheic keratosis.
- Muscle pain caused by medications called statins – Some reports suggest that taking vitamin D supplements can decrease symptoms of muscle pain in people taking statin drugs. But higher quality research is needed to confirm these results.
- Thinning of the walls of the vagina (vaginal atrophy) – Early research shows that taking vitamin D supplements for a least one year improves the surface of the vaginal wall. However, it does not seem to improve symptoms of vaginal atrophy.
- Warts – Reports suggest that applying maxacalcitol, which comes from vitamin D3, to the skin, can reduce viral warts in people with weakened immune systems.
- Weight loss – Early research shows that people with lower vitamin D levels are more likely to be obese than those with higher levels. Women taking calcium plus vitamin D are more likely to lose weight and maintain their weight. However, this benefit is mainly in women who did not consume enough calcium before they started taking supplements. Also, other research shows that taking vitamin D only helps with weight loss when blood levels are increased in post-menopausal overweight or obese women. When vitamin D is taken by people who are overweight and normal weight, it does not seem to help with weight loss or fat loss.
- Breathing disorders
- Bronchitis
Side Effects of Taking Vitamin D
- Although vitamin D deficiency is commonly seen in practice, vitamin D toxicity is very rare [rx]. Vitamin D toxicity is defined by most experts as having a serum 25-hydroxyvitamin D [25(OH)D] concentration of more than 150 ng/mL [rx]. Vitamin D toxicity is caused by excessive ingestion of vitamin D supplements over an extended period of time and is not attributed to prolonged sunlight exposure [rx].
- Clinical signs and symptoms of vitamin D toxicity are often vague, such as poor appetite, weight loss, increased urination, and arrhythmias [rx]. Additionally, high levels of vitamin D for long periods have been attributed to hypercalcemia and hyperphosphatemia and, subsequently, cardiovascular and kidney damage [rx].
- Therefore, patients who are being treated for vitamin D deficiency with high doses of vitamin D supplementation for a long period of time should have their lab values monitored closely [rx]
References