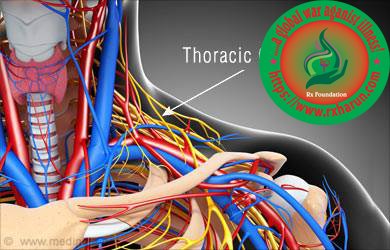
Thoracic outlet syndrome can be described compression of the neurovascular structures as they exit through the thoracic outlet (cervicothoracobrachial region). It is a condition in which there is compression of the nerves, arteries, or veins in the passageway from the lower neck to the armpit. The neurogenic type is the most common and presents with pain, weakness, and occasionally loss of muscle at the base of the thumb. The venous type results in swelling, pain, and possibly a bluish coloration of the arm.The arterial type results in pain, coldness, and paleness of the arm The thoracic outlet is marked by the anterior scalene muscle anteriorly, the middle scalene posteriorly, and the first rib inferiorly.
Thoracic outlet syndrome covers a wide range of manifestations due to compression of nerves and vessels during their passage through the cervicothoracobrachial region. Various forms of TOS are distinguished: vascular forms (arterial or venous) which raise few diagnostic problems [Rx], and “neurological” forms, which are by far the most frequent as they represent more than 95% of all cases of TOS [Rx, Rx]. The “neurological forms” are classified in the “true” neurological form associated with neurological deficits (mostly muscular atrophy), and painful neurological forms (with no objective neurological deficit). These painful forms are very frequent, especially when patients are systematically screened for these symptoms. The existence of these forms of TOS remains controversial in part because muscular and neurological manifestations are strongly interrelated. Clinical experience suggests that the main triggering mechanism is more often a muscular dysfunction in the cervicoscapular region than primitive nerve compression. It is directly responsible for cervicoscapular symptoms (pain and discomfort) and sometimes for referred scapulobrachial and facial pain. In parallel, shortened muscles (mainly scalene muscles) and cervicoscapular muscles imbalance may lead to intermittent nerve compression and/or tension on brachial plexus in the thoracic outlet resulting in proximal pain and producing pain and discomfort in the upper limb. The neurological involvement accounts for most of the distal symptoms, but the controversy concerning the reality of TOS is essentially due to the absence of objective criteria to confirm the diagnosis (no neurological weakness and normal neurophysiological examination). Despite considered as “debatable” for some authors, several arguments support the reality of this syndrome, such as the influence of TOS on the results of treatment of carpal tunnel and cubital tunnel syndromes [Rx,Rx]. This problem is further complicated by the frequent concomitant presence of other neuromuscular diseases of the upper limb, which can be secondary to TOS or, on the contrary, may precede and predispose to the development of TOS [Rx, Rx], in which case TOS is often masked by the concomitant disease. “Neurological” forms of TOS can be subdivided into primary forms in which features of TOS may remain isolated or may be complicated by underlying neuromuscular disorders, and forms secondary to a more distal disease (neuromuscular or joint disease), always responsible for complex clinical features.

Types of Thoracic Outlet Syndrome
- Vascular – This can be a compression of the artery and vein.
- Neurogenic – The nerves become compromised from an extra cervical rib, present at birth.
- Disputed or painful form –There is no neurological deficit but patients experience neurological symptoms and pain. Typically these patients’ electrodiagnostic studies (EMG / NCV) are normal, but they complain of pain.
The subtypes include
- Arterial TOS (A-TOS) – due to compression of the subclavian artery, most commonly caused by a cervical rib. Symptoms may include blood clots, arm pain with exertion, or acute arterial thrombosis (sudden blood flow obstruction in an artery).
- Venous TOS (V-TOS) – due to compression of the subclavian vein, often associated with repetitive arm activities. It may cause pain, swelling, and deep vein thrombosis.
- Traumatic neurovascular TOS – occurs after trauma to the collarbone and may affect both nerves and vessels. Symptoms may include pain, swelling, bruising, weakness, and loss of sensation in the arm and hand.
- True neurogenic TOS (TN-TOS) – caused by compression of the brachial plexus. Symptoms include numbness, abnormal sensations, and weakness of the arms and shoulders, as well as pain in the neck, shoulder or hand.
- Disputed TOS – the vast majority of neurogenic cases. It is controversial whether it is a true form of TOS because it lacks a consistent physical abnormality, a recognized cause, consistent symptoms, a reliable method of testing, and a standard treatment. Pain and tingling or numbness in the neck, arm and hand are common complaints..
Anatomy of Thoracic Outlet Syndrome
Thoracic outlet
Borders
- Anterior: anterior scalene muscle
- Posterior: middle scalene muscle
- Inferior: first rib
Contents
- Brachial plexus trunks
- Subclavian artery
- Subclavian vein does not pass through interscalene triangle
- runs beneath anterior scalene muscle prior to entering the costoclavicular space
Costoclavicular space
- Middle space
- Separated from the interscalene triangle by the first rib
Borders
- anterior: clavicle and subclavius muscle
- posterior: first rib and scalene muscles
- medial: costoclavicular ligament
- lateral: upper scapular border
Contents
- Brachial plexus divisions
- Subclavian artery and vein
Retropectoralis minor space
- Distal space
- Also known as the thoraco-coraco-pectoral space or subcoracoid space
- Borders
- superior: coracoid
- anterior: pectoralis minor muscle
- posterior: ribs 2-4
Thoracic Outlet Syndrome
- Brachial plexus cords
- Axillary artery and vein
Causes of Thoracic Outlet Syndrome
TOS can be attributed to one or more of the following factors
- Congenital abnormalities – are often reported and can be associated with traumatic or functional causes. Bone anomalies (cervical rib, prolonged transverse process), fibrous anomalies (transversocostal, costocostal, etc.), or muscular anomalies (scalenus anticus muscle, sickle-shaped scalenus medius, etc.) are more frequent in patients who develop TOS [Rx]. Bone anomalies are well known, but 2/3 of the abnormalities detected at operation are fibromuscular [Rx] and the majority of bone anomalies do not cause TOS [Rx, Rx]. These anomalies are part of a real local and regional “dysplasia” constituting only one of the numerous predisposing factors, associated with a morphotype composed of narrow, drooping shoulders.
Congenital factors
- Cervical rib
- Prolonged transverse process
- Anomalous muscles
- Fibrous anomalies (transverse costal, costocostal)
- Abnormalities of the insertion of the scalene muscles
- Fibrous muscular bands
- Exostosis of the first rib
- Cervicodorsal scoliosis
- Congenital uni- or bilateral elevated scapula
- Location of the A. or V. Subclavian in relation to the M. scalene anterior
Post-traumatic causes- either due to isolated trauma or repeated trauma, account for up to 2/3 of cases in some series [Rx, Rx]. Post-traumatic TOS due to soft tissue injury raises medicolegal and often management problems. These forms are related to neck and shoulder trauma, particularly “whiplash” injuries, or sometimes upper limb trauma. Injuries to scalene muscles and their subsequent fibrosis are implicated in this process [Rx, Rx]. Diagnostic criteria of post-traumatic TOS are the pathogenic mechanism and the onset of symptoms within the first two years.
- Functional acquired – causes are the most controversial, although probably the most frequent. In this group, upper limb dysfunction or a muscle imbalance of the neck and shoulder region is considered to be responsible [Rx, Rx]. Two main features are mainly associated with “functional” acquired causes: “hypertrophic” muscle morphotype of the cervicoscapular region and “dropped” scapular morphotype (leading in some patients to a dysfunction of the normal scalenus anterior muscle). Muscles of the thoracic outlet are also accessory respiratory muscles capable of prolonged tonic contractions due to their high percentage of type I muscle fibres [Rx]. Chronic stimulation of these muscles has also been shown to increase the percentage of type I fibres. Machleder showed that a normal scalenus anterior muscle contains 70% of type I fibres versus 85% in the case of TOS [Rx]. The factors involved in the pathogenesis of these disorders include overuse and physical and mental stress phenomena, frequently associated with unfavourable psychosocial factors [Rx
- Postural factors
- Dropped shoulder condition
- Wrong work posture (standing or sitting without paying attention to the physiological curvature of the spine
- Heavy mammaries
- Trauma
- Clavicle fracture
- Rib fracture
- Hyperextension neck injury, whiplash
- Repetitive stress injuries (repetitive injury most often form sitting at a keyboard for long hours)
- Muscular causes – Hypertrophy of the scalene muscles Decrease of the tonus of the M. trapezius, M. levator scapulae, M.rhomboids
Shortening of the scalene muscles, M. trapezius, M. levator scapulae, pectoral muscles - Post-traumatic causes – either due to isolated trauma or repeated trauma, account for up to 2/3 of cases in some series [Rx, Rx]. Post-traumatic TOS due to soft tissue injury raises medicolegal and often management problems. These forms are related to neck and shoulder trauma, particularly “whiplash” injuries, or sometimes upper limb trauma. Injuries to scalene muscles and their subsequent fibrosis are implicated in this process [Rx, Rx]. Diagnostic criteria of post-traumatic TOS are the pathogenic mechanism and the onset of symptoms within the first two years.
Others Causes of Thoracic Outlet Syndrome
- Trauma – (e.g., whiplash injuries) or repetitive strain is frequently implicated.Rarer acquired causes include tumors, hyperostosis, and osteomyelitis
- Anatomical defects – Inherited defects that are present at birth (congenital) may include an extra rib located above the first rib (cervical rib) or an abnormally tight fibrous band connecting your spine to your rib.
- Poor posture – Drooping your shoulders or holding your head in a forward position can cause compression in the thoracic outlet area.
- Trauma – A traumatic event, such as a car accident, can cause internal changes that then compress the nerves in the thoracic outlet. The onset of symptoms related to a traumatic accident often is delayed.
- Repetitive activity – Doing the same thing repeatedly can, over time, wear on your body’s tissue. You may notice symptoms of thoracic outlet syndrome if your job requires you to repeat a movement continuously, such as typing on a computer, working on an assembly line or lifting things above your head, as you would if you were stocking shelves.
- Pressure on your joints – Obesity can put an undue amount of stress on your joints, as can carrying around an oversized bag or backpack.
Symptoms of Thoracic Outlet Syndrome
There are a number of types of thoracic outlet syndrome, including
- Neurogenic (neurological) thoracic outlet syndrome – This form of thoracic outlet syndrome is characterized by compression of the brachial plexus. The brachial plexus is a network of nerves that come from your spinal cord and control muscle movements and sensation in your shoulder, arm and hand. In the majority of thoracic outlet syndrome cases, the symptoms are neurogenic.
- Vascular thoracic outlet syndrome – This type of thoracic outlet syndrome occurs when one or more of the veins (venous thoracic outlet syndrome) or arteries (arterial thoracic outlet syndrome) under the collarbone (clavicle) are compressed.
- Nonspecific-type thoracic outlet syndrome – This type is also called disputed thoracic outlet syndrome. Some doctors don’t believe it exists, while others say it’s a common disorder. People with nonspecific-type thoracic outlet syndrome have chronic pain in the area of the thoracic outlet that worsens with activity, but a specific cause of the pain can’t be determined.
- Muscle wasting in the fleshy base of your thumb (Gilliatt-Sumner hand)
- Numbness or tingling in your arm or fingers
- Pain or aches in your neck, shoulder or hand
- Weakening grip
- Discoloration of your hand (bluish color)
- Arm pain and swelling, possibly due to blood clots
- Blood clot in veins or arteries in the upper area of your body
- Lack of color (pallor) in one or more of your fingers or your entire hand
- Weak or no pulse in the affected arm
- Cold fingers, hands or arms
- Arm fatigue with activity
- Numbness or tingling in your fingers
- Weakness of arm or neck
- Throbbing lump near your collarbone
Diagnosis of Thoracic Outlet Syndrome
- The following pathologies are common differential diagnosis for TOS
- Carpal tunnel syndrome
- De Quervain’s tenosynovitis
- Lateral epicondylitis
- Medial epicondylitis
- Complex regional pain syndrome (CRPS I or II).
- Horner’s Syndrome
- Raynaud’s disease
- disease (especially discogenic)
- Brachial plexus trauma
- Systemic disorders: inflammatory disease, esophageal or cardiac disease
- Upper extremity deep venous thrombosis , Paget-Schroetter syndrome
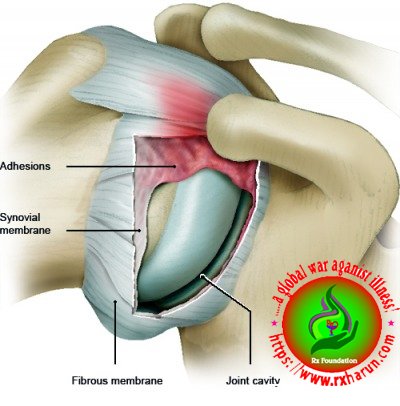
- Rotator cuff pathology
- Glenohumeral joint instability
- Nerve root involvement
- Malignancies (local tumours)
- Chest pain, angina
- Vasculitis
- Thoracic 4 syndrome
- Sympathetic-mediated pain
Systematic causes of brachial plexus pain include
- Pancoast’s Syndrome
- Radiation induced brachial plexopathy
- Parsonage Turner Syndrome
- carpal tunnel syndrome
- peripheral neuropathies (like ulnar nerve entrapment at the elbow, shoulder tendinitis and impingement syndrome)
- fibromyalgia of the shoulder and neck muscles
- cervical disc disease (like cervical spondylosis and herniated cervical disk)
History and examination features in ATOS, VTOS, and NTOS.
| TOS Subtype | History | Examination |
|---|---|---|
| ATOS | Claudication/rest pain of upper limb, excluding shoulder/neck Numbness, coolness, pallor |
Raynaud’s phenomenon Upper limb ischaemia, digital ulceration, peripheral embolisation Pulsatile mass ± bruit on auscultation Blood pressure differential >20 mmHg Positive EAST, ULTT, Adson’s test |
| VTOS | Deep pain on movement or rest pain in upper limb, chest, shoulder Swelling and cyanotic discoloration |
Upper limb swelling Cyanosis Positive EAST, ULTT, Adson’s test |
| NTOS | Pain in neck, trapezius, shoulder, arm, chest, occipital headache Variable pattern upper limb weakness, numbness, paraesthesias |
Tenderness on palpation: scalene triangle, subcoracoid space Upper plexus (C5-C7): sensory disturbance of arm. Weakness/atrophy of deltoid, biceps, brachialis Lower plexus (C8-T1): sensory disturbance ulnar forearm & hand. Weakness/atrophy of small muscles of the hand, weak wrist & finger flexion Positive EAST, ULTT, Adson’s test |
Special Tests
- Elevated Arm Stress/ Roos test – The patient has arms at 90° abduction and the therapist puts downwards pressure on the scapula as the patient opens and closes the fingers. If the TOS symptoms are reproduced within 90 seconds, the test is positive.
- Adson’s – The patient is asked to rotate the head and elevate the chin toward the affected side. If the radial pulse on the side is absent or decreased then the test is positive, showing the vascular component of the neurovascular bundle is compressed by the scalene muscle or cervical rib.
- Wright’s – The patient’s arm is hyper abducted. If there is a decrease or absence of a pulse on one side then the test is positive, showing the axillary artery is compressed by the pectoralis minor muscle or coracoid process due to stretching of the neurovascular bundle.
- Cyriax Release – The patient is seated or standing. The examiner stands behind the patient and grasps under the forearms, holding the elbows at 80 degrees of flexion with the forearms and wrists in neutral. The examiner leans the patient’s trunk posteriorly and passively elevated the shoulder girdle. This position is held for up to 3 minutes. The test is positive when paresthesia and/or numbness (release phenomenon) occurs, including a reproduction of symptoms.
- Supraclavicular Pressure – The patient is seated with the arms at the side. The examiner places his fingers on the upper trapezius and thumb on the anterior scalene muscle near the first rib. Then the examiner squeezes the fingers and thumb together for 30 seconds. If there is a reproduction of pain or paresthesia the test is positive, this addresses compromise to brachial plexus through scalene triangles.
- Costoclavicular Maneuver – This test may be used for both neurological and vascular compromise. The patient brings his shoulders posteriorly and hyperflexes his chin. A decrease in symptoms means that the test is positive and that the neurogenic component of the neurovascular bundle is compressed.
- Upper Limb Tension – These tests are designed to put stress on neurological structures of the upper limb. The shoulder, elbow, forearm, wrist, and fingers are kept in specific position to put stress on the particular nerve (nerve bias) and further modification in the position of each joint is done as “sensitizer”.
- Cervical Rotation Lateral Flexion – The test is performed with the patient in sitting. The cervical spine is passively and maximally rotated away from the side being tested. While maintaining this position, the spine is gently flexed as far as possible moving the ear toward the chest. A test is considered positive when the lateral flexion movement is blocked.
Others Test
- An X-ray of the thoracic outlet can reveal whether you have an extra rib. It may also rule out other conditions that could be causing your symptoms.
- An MRI uses powerful magnets and radio waves to create clear, detailed images of the thoracic outlet. The pictures can help determine the location and cause of the compression. They may also show certain structural abnormalities that could be causing your symptoms.
- Electromyography allows your doctor to see how well the muscles and nerves in the thoracic outlet are working. During this test, an electrode is inserted through your skin into various muscles. It evaluates the electrical activity of your muscles when at rest and when contracted.
- A nerve conduction study uses a low amount of electrical current to measure how quickly your nerves send impulses to various muscles throughout the body. It can determine whether you have nerve damage.
Treatment of Thoracic Outlet Syndrome
- Analgesics: Prescription-strength drugs that relieve pain but not inflammation.
- Antidepressants: A Drugs that block pain messages from your brain and boost the effects of eorphins .
- Medication – Common pain remedies such as aspirin, acetaminophen, ibuprofen and naproxen can offer short-term relief. All are available in low doses without a prescription. Other medications, including muscle relaxants and anti-seizure medications, treat aspects of spinal stenosis, such as muscle spasms and damaged nerves.
- Corticosteroid injections – Your doctor will inject a steroid such as prednisone into your back or neck. Steroids make inflammation go down. However, because of side effects, they are used sparingly.
- Anesthetics – Used with precision, an injection of a “nerve block” can stop pain for a time.
- Muscle Relaxants – These medications provide relief from spinal muscle spasms.
- Neuropathic Agents – Drugs(pregabalin & gabapentine) that address neuropathic—or nerve-related—pain. This includes burning, numbness, and tingling.
- Opioids – Also known as narcotics, these medications are intense pain relievers that should only be used under a doctor’s careful supervision.
- Topical Medications – These prescription-strength creams, gels, ointments, patches, and sprays help relieve pain and inflammation through the skin.
- Calcium & vitamin D3 – to improve bones health and healing fracture.
Others Treatment Approach
- Transaxillary approach – The first rib forms the common denominator for all causes of nerve and artery compression in this region, so that its removal generally improves symptoms. Surgeon makes an incision in the chest to access the first rib, divide the muscles in front of the rib and remove a portion of the first rib to relieve compression, without disturbing the nerves or blood vessels.
- Supraclavicular approach – Has been advocated to perform first rib resection and scalenectomy, a safe and effective procedure, characterized by a shorter operative time and having a complication rate lower or comparable to that of transaxillary first rib resection.
This approach repairs compressed blood vessels. The surgeon makes an incision just under the neck to expose the brachial plexus region. Then he looks for signs of trauma or muscles contributing to compression near the first rib. The first rib may be removed if necessary to relieve compression. - Arterial TOS – Decompression can include cervical and/or first rib removal and scalene muscle revision. The subclavian can then be inspected for degeneration, dilation, or an aneurysm. Saphenous vein graft or synthetic prosthesis can then be used if necessary Level of evidence 2B.
- Venous TOS – Thrombolytic therapy is the first line of treatment for these patients. Because of the risk of recurrence, many recommend removal of the first rib is necessary even when thrombolytic therapy completely opened the vein. The results of a study show that the infraclavicular approach is a safe and effective treatment for acute VTOS. They had no brachial plexus or phrenic nerve injuries.
Physical Therapy in Thoracic Outlet Syndrome
Conservative management should be the first strategy to treat TOS since this seems to be effective at decreasing symptoms, facilitating return to work and improving function, but yet a few studies have evaluated the optimal exercise program as well as the difference between a conservative management and no treatment.
Stage 1 – The aim of the initial stage is to decrease the patient’s symptoms. This may be achieved by patient education, in which TOS, bad postures, the prognosis and the importance of therapy compliance are explained. Furthermore some patients who sleep with the arms in an overhead, abducted position should get some information about their sleeping posture to avoid waking up at night.
- Cyriax release maneuver
- Elbows flexed to 90°
- Towels create a passive shoulder girdle elevation
- Supported spine and the head in neutral
- The position is held until peripheral symptoms are produced. The patient is encouraged to allow symptoms to occur as long as can be tolerated up to 30 minutes, observing for a symptom decrescendo as time passes.
- The patient’s breathing techniques need to be evaluated as the scalenes and other accessory muscles often compensate to elevate the rib cage during inspiration.
- Encouraging diaphragmatic breathing will lessen the workload on already overused or tight scalenes and can possibly reduce symptoms.
Stage 2 – Once the patient has control over his/her symptoms, the patient can move to this stage of treatment. The goal of this stage is to directly address the tissues that create structural limitations of motion and compression. How this should be done is one of the most discussed topics of this pathology. Some examples of methods that are used in the literature are.
- Massage
- Strengthening of the levator scapulae, sternocleidomastoid, and upper trapezius. This group of muscles open the thoracic outlet by raising the shoulder girdle and opening the costoclavicular space
- Stretching of the pectoralis, lower trapezius and scalene muscles
These muscles close the thoracic outlet
- Postural correction exercises
- Relaxation of shortened muscles Level of evidence 1A
- exercises in a daily home exercise program
- Shoulder exercises to restore the range of motion and so provide more space for the neurovascular structures.
Exercise
- Lift your shoulders backwards and up, flex your upper thoracic spine and move the shoulders forward and down. Then straightened the back and repeat 5 to 10 times.ROM of the upper cervical spine
Exercise
- Lower your chin 5 to 10 times against your chest, while you are standing with the back of your head against a wall. The effectiveness of this exercise can be enlarged by pressing the head down by hands.
- Activation of the scalene muscles are the most important exercises. These exercises help to normalize the function of the thoracic aperture as well as all the malfunctions of the first rib.
Exercises
Anterior scalene
- Press your forehead 5 times against the palm of your hand for a duration of 5 seconds, without creating any movement.
Middle scalene - Press your head sidewards against your palm.
Posterior scalene - Press your head backwards against your palm.
Stretching exercises
- Taping – some patients with severe symptoms respond to additional taping, adhesive bandages or braces that elevate or retract the shoulder girdle.
- Manipulative treatment to mobilize the first rib
- Repositioning/mobilization of the shoulder girdle and pelvis joints cervicothoracic, sternoclavicular, acromioclavicular, and costotransverse joints
- Glenohumeral mobilizations in end-range elevation with the elbow supported in extension
Posterior Glenohumeral Glide with Arm Flexion
- The patient is supine. The mobilization hand contacts the proximal humerus avoiding coracoid process. The force is directed posterolaterally (direction of thumb).
Anterior Glenohumeral Glide with Arm Scaption
- The patient is prone. The mobilization hand contacts the proximal humerus avoiding the acromion process. The force is directed anteromedially.
Inferior Glenohumeral Glide
- The patient is prone. The stabilizing hand holds the proximal humerus the humerus distal to the lateral acromion process. The mobilization hand contacts the axillary border of the scapula. Mobilize the scapula in a craniomedial direction along the ribcage.
References