Oogenesis is the maturation of the female gametes through meiotic division.
Key Points
- Oogenesis starts with the process of developing oogonia via the transformation of primordial follicles into primary oocytes, a process called oocytogenesis.
- Oocytogenesis is complete either before or shortly after birth in humans. During the menstrual cycle primary oocytes complete maturation through further meiotic divisions.
- The first meiotic division is coordinated by hormones: follicle-stimulating hormone (FSH), estrogen, luteinizing hormone (LH), and progesterone.
- The oocyte is arrested in cell division prior to the second meiotic division, which only occurs after fertilization.
Key Terms
- polar body: A small haploid cell formed concomitantly as an egg cell during oogenesis, but which does not have the ability to be fertilized.
- ootid: A nearly mature ovum that results from
meiotic division of a secondary oocyte. - luteinizing hormone: A hormone produced by the anterior pituitary gland. In females, an acute rise of LH triggers ovulation and development of the corpus luteum.
- follicle: A small cavity or sac that is the site of oocyte development in the ovary.
- follicle-stimulating hormone: A gonadotropic glycoprotein hormone, secreted in part of the pituitary gland that stimulates the growth of ovarian follicles in female mammals and induces spermatogenesis in male mammals.
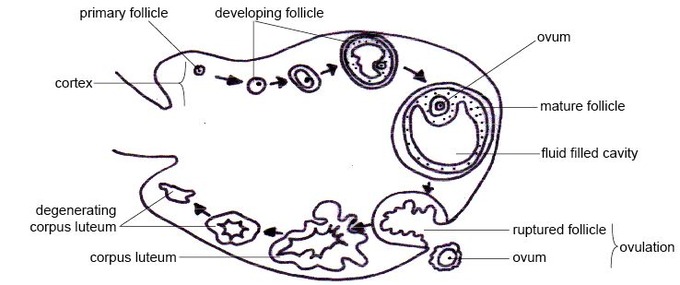
The menstrual cycle begins with the maturation of oocytes through the process of oogenesis, as well as concurrent follicle development that stimulates ovulation. Oogenesis starts with the process of developing oogonia via the transformation of primordial follicles into primary oocytes, a process called oocytogenesis. Oocytogenesis is complete either before or shortly after birth in humans. During the menstrual cycle primary oocytes complete maturation through further meiotic divisions.
Follicle development signals the beginning of the menstrual cycle. At the start of the menstrual cycle, some 12-20 primary follicles begin to develop under the influence of elevated levels of follicle-stimulating hormone (FSH) to form secondary follicles. The primary follicles form from primordial follicles, which develop in the ovary as a fetus during conception and are arrested in the prophase state of the cellular cycle.
By around day 9 of the menstrual cycle, only one healthy secondary follicle remain. The rest are reabsorbed into the ovary. The remaining follicle, called the dominant follicle, is responsible for producing large amounts of estrogen during the late follicular phase.
On day 14 of the cycle, a luteinizing hormone surge is triggered by the positive feedback of estrogen. This causes the secondary follicle to develop into a tertiary follicle, which then leaves the ovary 24–36 hours later. An important event in the development of the tertiary follicle occurs when the primary oocyte completes the first meiotic division, resulting in the formation of a polar body and a secondary oocyte. The empty follicle then forms a corpus luteum which later releases progesterone to maintain a potential pregnancy.
Immediately after meiosis I, the haploid secondary oocyte initiates meiosis II. However, this process is also halted at the metaphase II stage until fertilization occurs. When meiosis II has completed, an ootid and another polar body is created.
Both polar bodies disintegrate at the end of meiosis II, leaving only the ootid, which eventually develops into a mature ovum. The formation of polar bodies serves to discard the extra haploid sets of chromosomes that have resulted as a consequence of meiosis.
The Oogenesis Process: Diagram showing maturation of the ovum.
Ovarian Cycle
The menstrual cycle is the physiological process that fertile women undergo for the purposes of reproduction and fertilization.
LEARNING OBJECTIVES
Differentiate among the phases of the menstrual cycle
KEY TAKEAWAYS
Key Points
- The ovarian cycle refers to the series of changes in the ovary during which the follicle matures, the ovum is shed, and the corpus luteum develops.
- The follicular phase describes the development of the follicle in response to follicle stimulation hormone ( FSH ). As luteinizing hormone ( LH ) and FSH levels increase they stimulate ovulation, or the release of a mature oocyte into the fallopian tubes.
- In the luteal phase, the corpus luteum forms on the ovary and secretes many hormones, most significantly progesterone, which makes the endometrium of the uterus ready for implantation of an embryo.
- If implantation does not occur, the corpus luteum will be degraded, resulting in menstruation.
- If implantation occurs the corpus luteum is maintained.
Key Terms
- ischemic phase: The final part of the secretory phase. The endometrium becomes
pale and arteries constrict due to lower hormone release by the disintegrating corpus
luteum. - granulosa cells: These cells produce
hormones and growth factors that interact with the oocyte during its
development. - menstrual cycle: The recurring cycle of physiological changes in the females of some animal species that is associated with reproductive fertility.
- luteal phase: The latter part of the menstrual cycle that occurs after ovulation, in which the corpus luteum secretes progesterone to prepare the endometrium for the implantation of an embryo.
- follicular phase: The phase of the estrous cycle that involves follicular maturation within the ovary and, controlled by the hormone estradiol.
The menstrual cycle is the scientific term for the physiological changes that occur in fertile women for the purpose of sexual reproduction.The menstrual cycle is controlled by the endocrine system and commonly divided into three phases: the follicular phase, ovulation, and the luteal phase. However, some sources define these phases as menstruation, proliferative phase, and secretory phase. Menstrual cycles are counted from the first day of menstrual bleeding.
The Follicular Phase
The follicular phase (or proliferative phase) is the phase of the menstrual cycle in humans and great apes during which follicles in the ovary mature, ending with ovulation. The main hormone controlling this stage is estradiol. During the follicular phase, follicle-stimulating hormone (FSH) is secreted by the anterior pituitary gland. FSH levels begin to rise in the last few days of the previous menstrual cycle and peak during the first week of the follicular phase. The rise in FSH levels recruits five to seven tertiary-stage ovarian follicles (also known as Graafian or antral follicles) for entry into the menstrual cycle. These follicles compete with each other for dominance.
FSH induces the proliferation of granulosa cells in the developing follicles and the expression of luteinizing hormone (LH) receptors on these granulosa cells. Two or three days before LH levels begin to increase, usually by day seven of the cycle, one or occasionally two of the recruited follicles emerges as dominant. Many endocrinologists believe that estrogen secretion of the dominant follicle increases to a level that indirectly lowers the levels of LH and FSH. This slowdown in LH and FSH production leads to the atresia (death) of most of the recruited follicles, though the dominant follicle continues to mature.
These high estrogen levels initiate the formation of a new layer of endometrium in the uterus. Crypts in the cervix are also stimulated to produce fertile cervical mucus that reduces the acidity of the vagina, creating a more hospitable environment for sperm. In addition, basal body temperature may lower slightly under the influence of high estrogen levels. Ovulation normally occurs 30 (± 2) hours after the beginning of the LH surge (when LH is first detectable in urine).
Ovulation
Ovulation is the phase in which a mature ovarian follicle ruptures and discharges an ovum (also known as an oocyte, female gamete, or egg). Ovulation also occurs in the estrous cycle of other female mammals, which differs in many fundamental ways from the menstrual cycle. The time immediately surrounding ovulation is referred to as the ovulatory phase or the periovulatory period.
The Luteal Phase
The luteal phase (or secretory phase) is the latter part of the menstrual or estrous cycle. It begins with the formation of the corpus luteum and ends in either pregnancy or luteolysis. The main hormone associated with this stage is progesterone, which is significantly higher during the luteal phase than in other phases of the cycle. Some sources define the end of the luteal phase as a distinct ischemic phase.
After ovulation, the pituitary hormones FSH and LH cause the remaining parts of the dominant follicle to transform into the corpus luteum. It continues to grow for some time after ovulation and produces significant amounts of hormones, particularly progesterone, and to a lesser extent, estrogen. Progesterone plays a vital role in making the endometrium receptive to implantation of the blastocyst and supportive of the early pregnancy. It also raises the woman’s basal body temperature. The hormones produced by the corpus luteum suppress production of the FSH and LH, causing the corpus luteum will atrophy. The death of the corpus luteum results in falling levels of progesterone and estrogen. This in turn causes increased levels of FSH, leading to recruitment of follicles for the next cycle. Continued drops in estrogen and progesterone levels trigger the end of the luteal phase, menstruation, and the beginning of the next cycle.
The loss of the corpus luteum can be prevented by implantation of an embryo. After implantation, human embryos produce human chorionic gonadotropin (hCG), which is structurally similar to LH and can preserve the corpus luteum. Because the hormone is unique to the embryo, most pregnancy tests look for the presence of hCG. If implantation occurs, the corpus luteum will continue to produce progesterone (and maintain high basal body temperatures) for eight to twelve weeks, after which the placenta takes over this function.
The ovarian cycle: The ovarian cycle is the series of changes that occur in the ovary during the menstrual cycle that cause maturation of a follicle, ovulation, and development of the corpus luteum.
Uterine (Menstrual) Cycle
The uterine cycle describes a series of changes that occur to the lining of the uterus, or endometrium, during a typical menstrual cycle.
LEARNING OBJECTIVES
Outline the process of the uterine cycle
KEY TAKEAWAYS
Key Points
- The uterine cycle includes the increase in the endometrium in preparation for implantation and the shedding of the lining following lack of implantation, termed menstruation.
- Menstrual cycles are counted from the first day of menstrual bleeding.
- Endometrial thickening is stimulated by the increasing amount of estrogen in the follicular phase.
- If implantation does not occur, progesterone and estrogen levels drop, which stimulates menstruation.
Key Terms
- endometrium: The mucous membrane that lines the uterus in mammals, in which fertilized eggs are implanted.
- menstrual cycle: In the females of some animal species, the recurring cycle of physiological changes associated with reproductive fertility.
- decidua: A mucous membrane that lines the uterus: it is shed during menstruation and modified during pregnancy.
Several changes to the uterine lining (endometrium) occur during the menstrual cycle, also called the uterine cycle. The endometrium is the innermost glandular layer of the uterus. During the menstrual cycle, the endometrium grows to a thick, blood vessel-rich tissue lining, representing an optimal environment for the implantation of a blastocyst upon its arrival in the uterus. Menstrual cycles are counted from the first day of menstrual bleeding and are typically 28 days long.
During menstruation, the body begins to prepare for ovulation again. The levels of estrogen gradually rise, signalling the start of the follicular, or proliferation, phase of the menstrual cycle. The discharge of blood slows and then stops in response to rising hormone levels and the lining of the uterus thickens, or proliferates. Ovulation is triggered by a surge in luteinizing hormone. The sudden change in hormones at the time of ovulation sometimes causes minor changes in the endometrium and light midcycle blood flow.
After ovulation, under the influence of progesterone, the endometrium changes to a secretory lining in preparation for the potential implantation of an embryo to establish a pregnancy. If a blastocyst implants, then the lining remains as the decidua. This becomes part of the placenta and provides support and protection for the embryo during gestation.
If implantation does not occur within approximately two weeks, the progesterone-producing corpus luteum in the ovary will recede, causing sharp drops in levels of both progesterone and estrogen. This hormone decrease causes the uterus to shed its lining and the egg in menstruation. The cessation of menstrual cycles at the end of a woman’s reproductive period is termed menopause. The average age of menopause in women is 52 years, but it can occur anytime between 45 and 55.
The Uterine Cycle: High estrogen and progesterone levels stimulate increased endometrial thickness, but following their decline from a lack of implantation, the endometrium is shed and menstruation occurs.
Normal menstrual flow can occur although ovulation does not occur. This is referred to as an anovulatory cycle. Follicular development may start but not be completed although estrogen will still stimulate the uterine lining. Anovulatory flow that results from a very thick endometrium caused by prolonged, continued high estrogen levels is called estrogen breakthrough bleeding. However, if it is triggered by a sudden drop in estrogen levels, it is called withdrawal bleeding. Anovulatory cycles commonly occur before menopause and in women with polycystic ovary syndrome.
Hormonal Regulation of the Female Reproductive Cycle
The menstrual cycle is controlled by a series of changes in hormone levels, primarily estrogen and progesterone.
LEARNING OBJECTIVES
Differentiate among the phases of the menstrual cycle
KEY TAKEAWAYS
Key Points
- The follicular phase begins with an increase in follicle -stimulation hormone ( FSH ), which causes increases in luteinizing hormone ( LH ) and gonadotropin-releasing hormone ( GnRH ). Concurrent increases in estrogen levels cause increases in progesterone, stimulating proliferation of the endometrium.
- A spike in LH and FSH (“LH surge”) causes ovulation, following a suppression of GnRH.
- Estrogen levels continue to rise following ovulation and the corpus luteum forms, which secretes progesterone in significant levels and causes decreases in LH and FSH levels.
- Without implantation, estrogen and progesterone levels will fall and the corpus luteum will degrade.
Key Terms
- estrogen: A hormone responsible for the appearance of secondary sex characteristics of human females at puberty and the maturation and maintenance of the reproductive organs in their functional state.
- cumulus: A cluster of cells that surround the oocyte both in the ovarian follicle and after ovulation. These cells
coordinate follicular development and oocyte maturation. - progesterone: A steroid hormone secreted by the ovaries that prepares the uterus for the implantation of a fertilized ovum and subsequent pregnancy.
- theca cells: A group of endocrine cells in the ovary made
up of connective tissue surrounding the follicle. They provide
androgen synthesis and signal transduction between granulosa cells
and oocytes during development. - luteinizing hormone surge: Acute rise of LH levels that triggers ovulation and development of the corpus luteum.
The menstrual cycle is the physiological change that occurs under the control of the endocrine system in fertile women for the purposes of sexual reproduction and fertilization.
The Menstrual Cycle: The menstrual cycle is controlled by the endocrine system, with distinct phases correlated to changes in hormone concentrations.
Phases of the Menstrual Cycle
The menstrual cycle is divided into three stages: follicular phase, ovulation, and the luteal phase.
Follicular Phase
During the follicular phase (or proliferative phase), follicles in the ovary mature under the control of estradiol. Follicle-stimulating hormone (FSH) is secreted by the anterior pituitary gland beginning in the last few days of the previous menstrual cycle. Levels of FSH peak during the first week of the follicular phase. The rise in FSH recruits tertiary-stage ovarian follicles (antral follicles) for entry into the menstrual cycle.
Follicle-stimulating hormone induces the proliferation of granulosa cells in the developing follicles and the expression of luteinizing hormone (LH) receptors on these cells. Under the influence of FSH, granulosa cells begin estrogen secretion. This increased level of estrogen stimulates production of gonadotropin-releasing hormone (GnRH), which increases production of LH. LH induces androgen synthesis by theca cells, stimulates proliferation and differentiation, and increases LH receptor expression on granulosa cells.
Throughout the entire follicular phase, rising estrogen levels in the blood stimulate growth of the endometrium and myometrium of the uterus. This also causes endometrial cells to produce receptors for progesterone, which helps prime the endometrium to the late proliferative phase and the luteal phase. Two or three days before LH levels begin to increase, one or occasionally two of the recruited follicles emerge as dominant. Many endocrinologists believe that the estrogen secretion of the dominant follicle lowers the levels of LH and FSH, leading to the atresia (death) of most of the other recruited follicles. Estrogen levels will continue to increase for several days.
High estrogen levels initiate the formation of a new layer of endometrium in the uterus, the proliferative endometrium. Crypts in the cervix are stimulated to produce fertile cervical mucus that reduces the acidity of the vagina, creating a more hospitable environment for sperm. In addition, basal body temperature may lower slightly under the influence of high estrogen levels.
Ovulation
Estrogen levels are highest right before the LH surge begins. The short-term drop in steroid hormones between the beginning of the LH surge and ovulation may cause mid-cycle spotting or bleeding. Under the influence of the preovulatory LH surge, the first meiotic division of the oocytes is completed. The surge also initiates luteinization of theca and granulosa cells. Ovulation normally occurs 30 (± 2) hours after the beginning of the LH surge.
Ovulation is the process in a female’s menstrual cycle by which a mature ovarian follicle ruptures and discharges an ovum (oocyte). The time immediately surrounding ovulation is referred to as the ovulatory phase or the periovulatory period. In the preovulatory phase of the menstrual cycle, the ovarian follicle undergoes cumulus expansion stimulated by FSH. The ovum then leaves the follicle through the formed stigma. Ovulation is triggered by a spike in the amount of FSH and LH released from the pituitary gland.
Luteal Phase
The luteal phase begins with the formation of the corpus luteum stimulated by FSH and LH and ends in either pregnancy or luteolysis. The main hormone associated with this stage is progesterone, which is produced by the growing corpus luteum and is significantly higher during the luteal phase than other phases of the cycle. Progesterone plays a vital role in making the endometrium receptive to implantation of the blastocyst and supportive of the early pregnancy. It also raises the woman’s basal body temperature.
Several days after ovulation, the increasing amount of estrogen produced by the corpus luteum may cause one or two days of fertile cervical mucus, lower basal body temperatures, or both. This is known as a secondary estrogen surge. The hormones produced by the corpus luteum suppress production of the FSH and LH, which leads to its atrophy. The death of the corpus luteum results in falling levels of progesterone and estrogen, which triggers the end of the luteal phase. Increased levels of FSH start recruiting follicles for the next cycle.
Alternatively, the loss of the corpus luteum can be prevented by implantation of an embryo: after implantation, human embryos produce human chorionic gonadotropin (hCG). Human chorionic gonadotropin is structurally similar to LH and can preserve the corpus luteum. Because the hormone is unique to the embryo, most pregnancy tests look for the presence of hCG. If implantation occurs, the corpus luteum will continue to produce progesterone (and maintain high basal body temperatures) for eight to 12 weeks, after which the placenta takes over this function.
Extrauterine Effects of Estrogens and Progesterone
Estrogen and progesterone have several effects beyond their immediate roles in the menstrual cycle, pregnancy, and labor.
LEARNING OBJECTIVES
Describe the functions of progesterone and estrogen
KEY TAKEAWAYS
Key Points
- Estrogen promotes female secondary sex characteristics and has structural and metabolic functions, including bone formation, salt and water retention, and increased cortisol levels.
- The effects of progesterone are largely amplified by estrogen and include increases in core temperature, anti-inflammatory effects, increased use of fat for energy, and regulation of insulin release.
- Progesterone is sometimes called the ” hormone of pregnancy” as it has many roles relating to the fetal development, including preparing the uterus for implantation, increasing the amount of cervical mucus, and decreasing the maternal immune response.
Key Terms
- estrogen: A hormone responsible for the appearance of secondary sex characteristics of human females at puberty and for the maturation and maintenance of the reproductive organs in their mature functional state.
- aldosterone: A mineralocorticoid hormone secreted by the adrenal cortex that regulates the balance of sodium and potassium in the body.
- progesterone: A steroid hormone secreted by the ovaries that prepares the uterus for the implantation of a fertilized ovum and subsequent pregnancy.
Both estrogens and progesterone serve functions in the body beyond their roles in menstruation, pregnancy, and childbirth.
Estrogens Overview

Estradiol: One of the estrogens produced in the human body, predominant during a woman’s reproductive years.
Estrogens are a group of compounds named for their importance in the estrous cycle of humans and other animals. They are the primary female sex hormones, although they are found in males as well. The three major naturally occurring forms of estrogen in women are estrone (E1), estradiol (E2), and estriol (E3). Estetrol (E4) is produced only during pregnancy.
Natural estrogens are steroid hormones, while some synthetic versions are non-steroidal. Estrogens are synthesized in all vertebrates as well as some insects, and their presence in both suggests that they have an ancient evolutionary history. Like all steroid hormones, estrogen readily diffuses across the cell membrane. Once inside the cell, it binds to and activates estrogen receptors which in turn modulate the expression of many genes.
Functions of Estrogens

Estriol: Another one of the three main estrogens produced in humans.
While estrogens are present in both men and women, they are usually at significantly higher levels in women of reproductive age. They promote the development of female secondary sexual characteristics, such as breasts, pubic hair, and female fat distribution. They are also involved in the thickening of the endometrium and other aspects of menstrual cycle regulation.
Other functions of and structural changes induced by estrogen include:
- Formation of female secondary sex characteristics
- Accelerating metabolism
- Increasing fat stores
- Stimulating endometrial growth
- Increasing uterine growth
- Increasing vaginal lubrication
- Thickening the vaginal wall
- Maintaining blood vessels and skin
- Reducing bone resorption, increasing bone formation
- Reducing muscle mass
Effect on Libido
Sex drive is dependent on androgen levels only in the presence of estrogen. Without estrogen, free testosterone levels actually decrease sexual desire, as demonstrated in women who have hypoactive sexual desire disorder. The sexual desire in these women can be restored by administration of estrogen through oral contraceptives.
Mental Health
Estrogen plays a significant role in women’s mental health. Sudden estrogen withdrawal, fluctuating estrogen, and periods of sustained low levels of estrogen correlate with significant mood changes. Restoration or stabilization of estrogen levels is clinically effective for recovery from postpartum, perimenopause, and postmenopause depression.
Progesterone Overview

Progesterone: Belongs to the progestogen class of hormones and is the predominant example in the human body.
Progesterone is a steroid hormone involved in the female menstrual cycle, pregnancy (supports gestation ), and embryogenesis of humans and other species.
Progesterone belongs to a class of hormones called progestogens and is the major naturally-occurring human form in this category. Progesterone exerts its primary action through the intracellular progesterone receptor, although a distinct, membrane-bound progesterone receptor has also been postulated.
Functions of Progesterone
Progesterone has a number of physiological effects that are amplified in the presence of estrogen. Estrogen, through estrogen receptors, upregulates the expression of progesterone receptors. Also, elevated levels of progesterone potently reduce the sodium-retaining activity of aldosterone, resulting in natriuresis and a reduction in extracellular fluid volume. Progesterone withdrawal, on the other hand, is associated with a temporary increase in sodium retention (reduced natriuresis, with an increase in extracellular fluid volume) due to the compensatory increase in aldosterone production. This combats the blockade of the mineralocorticoid receptor by the previously-elevated level of progesterone.
Progesterone has key effects via non-genomic signalling on human sperm as they migrate through the female tract before fertilization occurs, though the receptor(s) as yet remain unidentified. Detailed characterization of the events occurring in sperm in response to progesterone has shed light on intracellular calcium transients, maintained changes, and slow calcium oscillations, now thought to possibly regulate motility.
Progesterone is sometimes called the “hormone of pregnancy” and has many roles relating to fetal development. It converts the endometrium to its secretory stage to prepare the uterus for implantation. At the same time, it affects the vaginal epithelium and cervical mucus, making them thick and impenetrable to sperm.
If pregnancy does not occur, progesterone levels will decrease, leading to menstruation. Normal menstrual bleeding is progesterone-withdrawal bleeding. If ovulation does not occur and the corpus luteum does not develop, its levels may be low, leading to anovulatory dysfunctional uterine bleeding. During implantation and gestation, progesterone appears to decrease the maternal immune response to allow for the acceptance of the pregnancy and decrease contractility of the uterine smooth muscle.
In addition, progesterone inhibits lactation during pregnancy. A drop in its levels is facilitates the onset of labor. Another drop following delivery is one of the triggers for milk production. The fetus metabolizes placental progesterone in the production of adrenal steroids.
Female Sexual Response
Female sexual arousal causes physiological changes including increased blood flow to the genitals and enlargement and lubrication of the vagina.
LEARNING OBJECTIVES
Explain the process of female sexual response
KEY TAKEAWAYS
Key Points
- Responses specific to females include engorgement of several tissues including the nipples, vulva, clitoris, and vaginal walls.
- Further changes include changes to the shape of the vagina and the positioning of the uterus in the pelvis, as well as increases in blood pressure and heart rate.
- Experienced by males and females, orgasms are controlled by the involuntary or autonomic nervous system.
- Age-related changes in sexual responsiveness may be associated with changes in estrogen.
Key Terms
- vulva: The vaginal opening to the uterus.
- estrogen: A hormone responsible for the appearance of secondary sex characteristics of females at puberty and for the maturation and maintenance of the reproductive organs in their mature functional state.
- clitoris: A small, sensitive, and elongated erectile organ at the anterior part of the vulva in females and homologous with the penis.
Sexual arousal is caused by sexual desire during or in anticipation of sexual activity. A number of physiological changes occur in the body and mind in preparation for sex and continue during the act. For women, these changes include increased blood flow to the nipples, vulva, clitoris, and vaginal walls, and increased vaginal lubrication.
Physiological Response

Features of the vulva: The clitoris and labial folds are labelled.
The beginnings of sexual arousal in a woman’s body is usually marked by vaginal lubrication, engorgement of the external genitals, and internal enlargement of the vagina. Further stimulation can lead to more vaginal wetness and further engorgement and swelling of the clitoris and the labia, along with increased redness or darkening of the skin in these areas. Changes also occur to the internal shape of the vagina and to the position of the uterus within the pelvis.
Other bodily changes include an increase in heart rate and blood pressure, as well as flushing across the chest and upper body. If sexual stimulation continues, then sexual arousal may peak into orgasm, resulting in rhythmic muscular contractions in the pelvic region characterized by an intense sensation of pleasure. Experienced by males and females, orgasms are controlled by the involuntary or autonomic nervous system.
As women age, estrogen levels decrease. Reduced estrogen levels may be associated with increased vaginal dryness and less clitoral erection when aroused, but are not directly related to other aspects of sexual interest or arousal. In older women, decreased pelvic muscle tone may prolong the time to reach orgasm, diminish the intensity of orgasms, and cause more rapid resolution. In some women, the uterine contracts that occur during orgasm may cause pain or discomfort.
Psychological Response
Mental and physical stimuli such as touch and the internal fluctuation of hormones influence sexual arousal. Cognitive factors like sexual motivation, perceived gender role expectations, and sexual attitudes play important roles in women’s self-reported levels of sexual arousal. Basson suggests that women’s need for intimacy prompts them to engage with sexual stimuli, leading to an experience of sexual desire and psychological sexual arousal.
Research by Goldey and van Anders showed that sexual cognition impacts hormone levels in women. For instance, sexual thoughts result in a rapid increase in testosterone in women who were not using hormonal contraception. Inconsistent study results indicate that, although testosterone is involved in libido and sexuality of some women, its effects can be obscured by the coexistence of psychological factors in others.