Supraspinatus tendon rupture is not only a relatively common lesion but an extremely painful one. In spite of this, the diagnosis is seldom made and the condition suffers from general neglect. These records covered fifteen years, and in them were listed six hundred and fifty varied types of painful shoulders. The diagnosis of complete rupture of the supraspinatus tendon was not made in a single case. This finding aroused great curiosity, and as a result personal conversations were held with twenty leading orthopedic surgeons in the middle and far west in the eight months that followed. Without a single exception, they readily admitted never having made the diagnosis of a complete rupture, and consequently, they had never seen or repaired such a rupture.
Musculotendinous rupture of the supraspinatus is an unusual lesion of the rotator cuff. With incomplete injuries, recovery can be anticipated with nonsurgical management. However, in the case of a complete rupture with muscle retraction, nonoperative management leads to unsatisfactory outcomes.
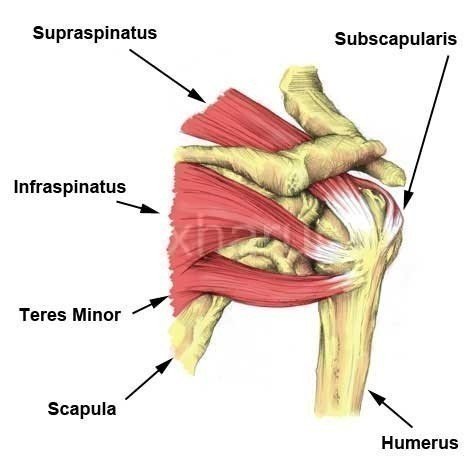
Anatomy
- Origin – medial 2/3 of supraspinatus fossa above the spine of scapula;
- Insertion – the superior surface of greater tuberosity of humerus and capsule of the shoulder joint;
- Dimensions – supraspinatus averages 25 mm wide and has a medial-to-lateral footprint (tendon attachment) of 12.1 mm at the mid-end
- Action – the abduction of the humerus at GHJ: stabilization of glenohumeral joint
- Nerve supply – suprascapular, C4, C5
- Synergist – deltoid;
- Injury – overuse of supraspinatus & resulting fatigue can subject amateur athlete to shoulder injuries.
- Exam – the supraspinatus muscle is tested with the shoulder abducted 90 degrees, flexed 30 deg and then maximally internally rotated; downward pressure is resisted primarily by the supraspinatus
- Function – The supraspinatus muscle performs abduction of the arm, and pulls the head of the humerus medially towards the glenoid cavity.[rx] It independently prevents the head of the humerus to slip inferiorly.[rx ] The supraspinatus works in cooperation with the deltoid muscle to perform abduction, including when the arm is in the adducted position.[rx] Beyond 15 degrees the deltoid muscle becomes increasingly more effective at abducting the arm and becomes the main propagator of this action.[rx]
Causes of Supraspinatus Tendon Rupture
- Sudden forceful fall down
- Road traffic accident
- Falls – Falling onto an outstretched hand is one of the most common causes of tendinitis.
- Sports injuries – Many Injury occurs during contact sports or sports in which you might fall onto an outstretched hand — such as in-line skating or snowboarding.
- Motor vehicle crashes – Motor vehicle crashes can cause necks of femur fracture to break, sometimes into many pieces, and often require surgical repair.
- Have osteoporosis – a disease that weakens your bones
- Eave low muscle mass or poor muscle strength – or lack agility and have poor balance (these conditions make you more likely to fall)
- Walk or do other activities in the snow or on the ice – or do activities that require a lot of forwarding momenta, such as in-line skating and skiing
- Wave an inadequate intake of calcium or vitamin D
- Football or soccer, especially on artificial turf
- Rugby
- Horseback riding
- Hockey
- Skiing
- Snowboarding
- In-line skating
- Jumping on a trampoline
Symptoms of Supraspinatus Tendon Rupture
In Acute Stage
- Many rotator cuff tears have no symptoms. Both partial and full-thickness tears have been found on post mortem and MRI studies in those without any history of shoulder pain or symptoms.
- However, the most common presentation is shoulder pain or discomfort. This may occur with activity, particularly shoulder activity above the horizontal position, but may also be present at rest in bed.
- Pain-restricted movement above the horizontal position may be present, as well as weakness with shoulder flexion and abduction.
- Severe pain that might worsen when gripping or squeezing or moving.
- Inability to move immediately after a fall
- Inability to put weight on your hand on the side of your injured thighs.
- Stiffness, bruising and swelling in and around your hip area
- Shorter leg on the side of your injured thighs.
- Turning outward of your leg on the side of your injured
- Swelling
- Tenderness
- Bruising
Chronic Stage
- You have Pain in the shoulder when doing a repetitive shoulder activity that eventually becomes noticeable when the shoulder is at rest.
- You are experiencing Atrophy (loss of Range of Motion)or weakening of the tendons and muscles in the rotator cuff.
- You have pain that starts as a dull ache and progresses to radiating pain from the shoulder, especially when sleeping.
- You have Sudden pain when reaching above the head or bringing the arm out to the side.
- You are experiencing Muscle spasm and weakness in the arm and shoulder area with a limited range of motion.
- You are experiencing a crackling sensation that may be felt as the condition worsens.
Diagnosis of Supraspinatus Tendon Rupture
A modification of the original Codman classification system published in 1930:
- Full-thickness rotator cuff tear (FTRCT)
- Complete cuff tear: full-thickness as well as full-width tear
- Vertical with a connection from joint to the bursa, not involving the whole breadth of the tendon
- Partial-thickness rotator cuff tear (PTRCT) bursal surface tear and articular surface tear
- Critical zone tear partial or full-thickness
- Rim rent tear: articular surface tear of the footprint
- Intratendinous tear / central tears: not in communication with the joint surface or with the bursal surface of the tendon; also known as tendon delamination or interstitial tear; if the gap is filled with fluid then it is called cleavage tear of the rotator cuff tendon
Radiographic features
Exact features depend on the type of tear, general features include Typically these are normal in acute tears with chronic tears showing degenerative-type changes
- May show a decreased acromiohumeral interval
- < 7 mm on true AP shoulder radiograph in chronic tears
- < 2 mm on an ‘active abduction’ view in acute tears
- May show decreased supraspinatus opacity and decreased bulk due to fatty atrophy in chronic tears
- Humeral subluxation superiorly may be seen in chronic tears
- May show features of acromial impingement
- spur formation on the undersurface of acromioclavicular joint
- acromion with an inferolateral tilt seen on outlet view (i.e. modified ‘Y’ view)
- type III acromion
- Secondary degenerative changes: sclerosis, subchondral cysts, osteolysis, and notching/pitting of greater tuberosity
Ultrasound
- In the hands of a good radiologist, ultrasound may have up to 90% sensitivity and specificity. It can also reveal other mimics like tendinosis, calcific tendinitis, subacromial-subdeltoid bursitis, greater tuberosity fracture, and adhesive capsulitis.
- Full-thickness tears extend from bursal to the articular surface, while partial-thickness tears are focal defects in the tendon that involve either the bursal or articular surface. Full-thickness appear on ultrasound as hypoechoic/anechoic defects in the tendon. Due to the fluid replacing tendon, cartilage shadow gets accentuated giving a ‘double cortex’ or ‘cartilage interface sign.
Direct signs are:
- Non-visualization of the supraspinatus tendon
- Hypoechoic discontinuity in tendon
Indirect signs are:
- Double cortex sign
- Sagging peribursal fat sign
- Compressibility
- Muscle atrophy
Secondary associated signs are:
- Cortical irregularity of greater tuberosity
- Shoulder joint effusion
- Fluid along the biceps tendon
- Fluid in the axillary pouch and posterior recess
MRI
- Complete tears are easier to diagnose on MRI than a full-thickness tear. Hyperintense signal area within the tendon on T2W, fat-suppressed and GRE sequences, usually corresponding to fluid signal is seen.
- Clinical judgment, rather than over-reliance on MRI or any other modality, is strongly advised in determining the cause of shoulder pain, or planning its treatment since rotator cuff tears are also found in some without pain or symptoms.
- The role of X-ray, MRI, and ultrasound, is adjunctive to clinical assessment and serves to confirm a diagnosis provisionally made by a thorough history and physical examination. Over-reliance on imaging may lead to overtreatment or distract from the true dysfunction causing symptoms.[rx]
Treatment of a supraspinatus Tendon Rupture
What can the athlete do?
- Rest – Continuing to use your arm when it is painful prevents your supraspinatus tear from healing.
- For a partial rupture – complete rest is best. Your shoulder should be immobilized in a sling or similar. See a sports injury specialist or doctor who can advise on treatment and rehabilitation.
- When your injury – has healed and you are pain-free, begin rotator cuff rehabilitation exercises. These should include mobility, strengthening and functional or sports specific exercises that should be done.
- Apply ice – after you get home from the hospital (regardless if you had surgery or not), you should apply a bag of crushed ice (or something cold) to your injured in order to reduce the swelling and numb the pain. Ice therapy is effective for acute (recent) injuries that involve swelling because it reduces blood flow by constricting local blood vessels. Apply the crushed ice to your injured area for 15 minutes three to five times daily until the soreness and inflammation eventually fade away or Ice can be applied for 15 minutes every 2 hours for the first day or two. From then on the frequency can be gradually reduced over a period of days.
-
Lightly exercise after the pain fades – after a couple of weeks when the swelling has subsided and the pain has faded away, remove your arm sling for short periods and carefully move in all different directions. Don’t aggravate the necks but gently reintroduce movements to the involved joints and muscles. Start cautiously, maybe starting with light and then progress to holding light weights (five-pound weights to start).
- Practice stretching and strengthening exercises – of the fingers, leg if your doctor recommends them.
- A splint – which you might use for a few days to a week while the swelling goes down; if a splint is used initially, a cast is usually put on about a week later.
- A cast – which you might need for six to eight weeks or longer, depending on how bad the break is (you might need a second cast if the first one gets too loose after the swelling goes away.)
- Get a referral to physical therapy – Once you’ve recovered and able to remove your arm sling splint for good, you’ll likely notice that the muscles surrounding your shoulder joint look smaller and feel weaker. That’s because muscle tissue atrophies without movement. If this occurs, then you’ll need to get a referral for some physical rehabilitation. Rehab can start once you are cleared by your orthopedist, are pain-free, and can perform all the basic arm and necks of femur fracture movements. A physiotherapist or athletic trainer can show you specific rehabilitation exercises and stretches to restore your muscle strength, joint movements, and flexibility
Medication
- Antibiotic – Cefuroxime or Azithromycin, or Flucloxacillin or any other cephalosporin/quinolone antibiotic must be used to prevent infection or clotted blood remove to prevent furthers swelling and edema. Antibiotics and tetanus vaccination may be used if the bone breaks through the skin creating immunization.
- NSAIDs – Prescription-strength drugs that reduce both pain and inflammation. Pain medicines and anti-inflammatory drugs help to relieve pain and stiffness, allowing for increased mobility and exercise. There are many common over-the-counter medicines called non-steroidal anti-inflammatory drugs (NSAIDs). They include and Ketorolac, Aceclofenac, Naproxen, Etoricoxib.
- Corticosteroids – Also known as oral steroids, these medications reduce inflammation.
- Muscle Relaxants – These medications provide relief from associated muscle spasms or injury
- Neuropathic Agents – Drugs(pregabalin & gabapentin) that address neuropathic—or nerve-related—pain. This includes burning, numbness, and tingling.
- Opioids – Also known as narcotics, these medications are intense pain relievers that should only be used under a doctor’s careful supervision.
- Topical Medications – These prescription-strength creams, gels, ointments, patches, and sprays help relieve pain and inflammation through the skin.
- Calcium & vitamin D3 – To improve bone health and healing fracture. As a general rule, men and women age 50 and older should consume 1,200 milligrams of calcium a day, and 600 international units of vitamin D a day.
- Glucosamine & Diacerein, Chondroitin sulfate – can be used to tightening the loose tendon, cartilage, ligament, and cartilage, ligament regenerates cartilage or inhabits the further degeneration of cartilage, ligament.
- Dietary supplement -to remove general weakness & healing and improved health.
- Antidepressants – A drug that blocks pain messages from your brain and boosts the effects of endorphins (your body’s natural painkillers).
- Menthol – provides deep penetrating pain relief with a nice cooling sensation
- Vitamin B1, B6, B12– promotes normal nerve function
- Vitamin E – anti-inflammatory, enhances circulation, hydrates the skin
- Aloe vera – anti-inflammatory properties, soothes the skin
- Tea Tree – enhances the penetration of ingredients
- MSM – supports healthy connective tissues, anti-inflammatory
- Ilex Leaf Extract – increases circulation, skin conditioner
Rehabilitation And Physiotherapy
Benefits attributed to Electromagnetic Energy (the energy used in TShellz Wraps):
Generally, it is accepted that heat on soft tissue (muscles, tendons, ligaments) provides the following desirable therapeutic effects:
- Electromagnetic heat increases the extensibility of collagen tissues – Tissues heated to 45 degrees Celsius and then stretched exhibit a nonelastic residual elongation of about 0.5 to 0.9 percent that persists after the stretch is removed. This does not occur in these same tissues when stretched at normal tissue temperatures. Therefore 20 stretching sessions can produce a 10 to 18 percentage increase in the length of tissues heated and stretched.
Stretching of tissue in the presence of heat would be especially valuable in working with ligaments, joint capsules, tendons, fascia, and synovium that have become scarred, thickened, or contracted. Such stretching at 45 degrees Celsius caused much less weakening in stretched tissues for a given elongation than a similar elongation produced at normal tissue temperatures.
Experiments cited clearly showed low-force stretching could produce significant residual elongation when heat is applied together with stretching or range-of-motion exercises. This is safer than stretching tissues at normal tissue temperatures. - Electromagnetic heat decreases joint stiffness –There was a 20 percent decrease in rheumatoid finger joint stiffness at 45 degrees Celsius (112 degrees Fahrenheit) as compared with 33 degrees Celsius (92 degrees Fahrenheit), which correlated perfectly to both subjective and objective observation of stiffness. Speculation has it that any stiffened joint and thickened connective tissues may respond in a similar fashion.
- Electromagnetic heat relieves muscle spasms – Muscle spasms have long been observed to be reduced through the use of heat, be they secondary to underlying skeletal, joint, or neuropathological conditions. This result is possibly produced by the combined effect of heat on both primary and secondary afferent nerves from spindle cells and from its effects on Golgi tendon organs. The results produced demonstrated their peak effect within the therapeutic temperature range obtainable with electromagnetic heat.
- Electromagnetic heat treatment leads to pain relief – Pain may be relieved via the reduction of attendant or secondary spasms. Pain is also at times related to ischemia (lack of blood supply) due to tension or spasm that can be improved by the hyperemia that heat-induced vasodilatation produces, thus breaking the feedback loop in which the ischemia leads to further spasm and then more pain.
The heat has been shown to reduce pain sensation by direct action on both free-nerve endings in tissues and on peripheral nerves. In one dental study, repeated heat applications led finally to the abolishment of the whole nerve response responsible for pain arising from dental pulp.
Localized electromagnetic therapy using lamps tuned to the 2 to 25-micron waveband is used for the treatment and relief of pain by over 40 reputable Chinese medical institutes. - Electromagnetic heat increases blood flow – Heating muscles produces an increased blood flow level similar to that seen during exercise. Temperature elevation also produces an increased blood flow and dilation directly in capillaries, arterioles, and venules, probably through direct action on their smooth muscles. The release of bradykinin, released as a consequence of sweat-gland activity, also produces increased blood flow and vasodilatation.
- Electromagnetic heat assists in resolution of inflammatory infiltrate, edema and exudates Increased peripheral circulation provides the transport needed to help evacuate edema, which can help inflammation, decrease pain, and help speed healing.
- Electromagnetic heat affects soft tissue injury – Electromagnetic healing is now becoming leading-edge care for soft tissue injuries to promote both reliefs in chronic or intractable “permanent” cases and accelerated healing in newer injuries.
Associate
- Supraspinatus Tendonitis
- Subacromial Impingement
- Supraspinatus Tear
References

About the author