What Is Facial Hemiplegia?/Facial Hemiplegia also referred to as partial facial paralysis, this is a form of partial hemiplegia where the muscles on one side of the face are paralyzed. Often caused by a stroke or similar brain injury. This may or may not be associated with complete/incomplete hemiplegia in other areas of the body.
Hemiplegia is a neurological condition that affects paralysis is on one vertical half of the body. Its most obvious result is a varying degree of weakness and lack of control on one side of the body. It affects everyone differently but its most obvious result is a varying degree of weakness and lack of control in one side of the body. You may be reading this because your child or someone you know has hemiplegia.
Hemiplegia, paralysis of the muscles of the lower face, arm, and leg on one side of the body. The most common cause of hemiplegia is a stroke, which damages the corticospinal tracts in one hemisphere of the brain. The corticospinal tracts extend from the lower spinal cord to the cerebral cortex. They decussate, or cross, in the brainstem; therefore, damage to the right cerebral hemisphere results in paralysis of the left side of the body. Damage to the left hemisphere of a right-handed person may also result in aphasia. Other causes of hemiplegia include trauma, such as spinal cord injury; brain tumors; and brain infections.
Hemiplegia is a condition where half of the body is paralyzed due to damage to the parts of the brain responsible for movement. Hemiparesis and hemiplegia can be caused by different medical conditions, including congenital causes, trauma, tumors, or stroke, etc.
Types of Hemiplegia
- Alternate hemiplegia – paralysis of one side of the face and the opposite side of the body.
- Cerebral hemiplegia – that due to a brain lesion.
- Crossed hemiplegia – alternate hemiplegia. It affects the alter side of the body instated of the affected side.
- Facial hemiplegia paralysis – of one side of the face.
- Spastic hemiplegia – with spasticity of the affected muscles and increased tendon reflexes.
- Spinal hemiplegia – due to a lesion of the spinal cord.
While hemiplegia is typically characterized as paralysis on one side of the body, there are multiple types of hemiplegia—some of which may be more limited in scope than others. A few different types of hemiplegia include:
- Facial Hemiplegia – Also referred to as partial facial paralysis, this is a form of partial hemiplegia where the muscles on one side of the face are paralyzed. Often caused by a stroke or similar brain injury. This may or may not be associated with complete/incomplete hemiplegia in other areas of the body.
- Cerebral Hemiplegia – When hemiplegia is caused by cerebral palsy (or other conditions affecting the brain), it can be referred to as cerebral hemiplegia. Cerebral hemiplegia symptoms are often similar to other forms of hemiplegia but may vary in severity and duration depending on the condition causing the paralysis.
- Spastic Hemiplegia – A variation of hemiplegia where the muscles on one side of the body are in a state of constant contraction. This type of hemiplegia may result in muscle pain, deformities in affected limbs (in extreme cases), and difficulty walking or maintaining motor control. Closely linked to cerebral palsy, and the severity (as well as the duration) of spastic hemiplegia symptoms may vary from case to case.
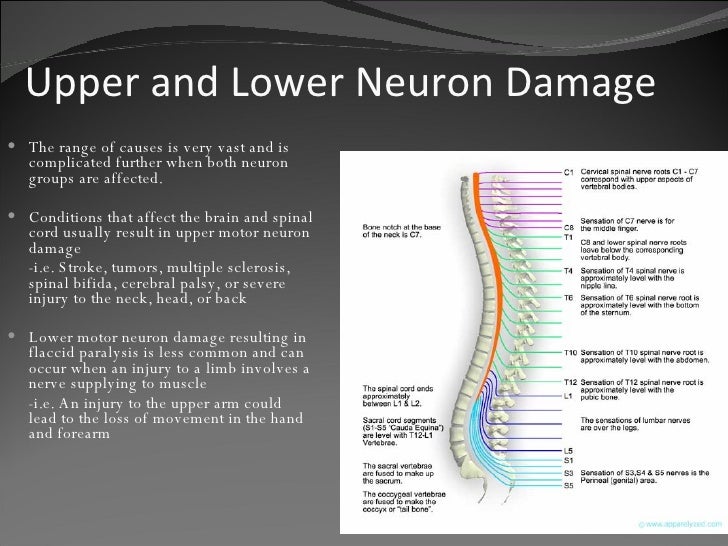
- Spinal Hemiplegia – Often the result of an incomplete injury to the spinal cord or lesions on spinal nerves (especially at the C6 vertebra or higher). Spinal cord injury hemiplegia is often a long-term condition.
Causes of Facial Hemiplegia
Though the arms, legs, and possibly torso are the regions of the body most obviously affected by hemiplegia, in most cases of hemiplegia these body regions are actually perfectly healthy. Instead, the problem resides in the brain, which is unable to produce, send, or interpret signals due to disease or trauma-related damage. Less frequently, hemiplegia results from damage to one side of the spinal cord, but these sorts of injuries more typically produce global problems, not just paralysis on one side of the body.
- Traumatic brain injuries to one side of the brain only. These may be caused by car accidents, falls, acts of violence, and other factors.
- Cardiovascular problems, particularly aneurysms and hemorrhages in the brain.
- Strokes and transient ischemic attacks (better known as TIA or mini-strokes).
- Infections, particularly encephalitis and meningitis. Some serious infections, particularly sepsis and abscesses in the neck, may spread to the brain if left untreated.
- Conditions that cause demyelination of the brain, including multiple sclerosis and some other autoimmune diseases.
- Traumatic brain injuries to one side of the brain only. These may be caused by car accidents, falls, acts of violence, and other factors.
- Cardiovascular problems, particularly aneurysms and hemorrhages in the brain.
- Strokes and transient ischemic attacks (better known as TIA or mini-strokes).
- Infections, particularly encephalitis and meningitis. Some serious infections, particularly sepsis and abscesses in the neck, may spread to the brain if left untreated.
- Conditions that cause demyelination of the brain, including multiple sclerosis and some other autoimmune diseases.
- Reactions to surgery, medication, or anesthesia.
- Loss of oxygen to the brain due to choking or anaphylactic shock.
- Brain cancers.
- Lesions in the brain, even if non-cancerous, since these lesions can impede function on one side of the brain.
- Congenital abnormalities, including cerebral palsy and neonatal-onset multi-inflammatory disease.
- Rarely, psychological causes; some states of catatonia can cause hemiplegia, and people with parasomnia—a sleep disorder leading to unusual nighttime behavior—may experience nighttime episodes of hemiplegia.
- Reactions to surgery, medication, or anesthesia.
- Loss of oxygen to the brain due to choking or anaphylactic shock.
- Brain cancers.
- Lesions in the brain, even if non-cancerous, since these lesions can impede function on one side of the brain.
- Congenital abnormalities, including cerebral palsy and neonatal-onset multi-inflammatory disease.
- Rarely, psychological causes; some states of catatonia can cause hemiplegia, and people with parasomnia—a sleep disorder leading to unusual nighttime behavior—may experience nighttime episodes of hemiplegia.
Rx
Some common causes of hemiplegia include
Stroke is the commonest cause of hemiplegia. Insufficient blood supply to the brain leads to loss of brain functions. The stroke may be caused by:
- A clot formed within the blood vessel blocking the blood supply -> a thrombus
- A thrombus breaks away from its site of origin and forms a block elsewhere in the circulation -> an emboli
- A bleed from a blood vessel supplying the brain -> a hemorrhage
- A thrombus breaks away from its site of origin and forms a block elsewhere in the circulation. -> an emboli
- A bleed from a blood vessel supplying the brain -> a hemorrhage
- Traumatic brain injuries to one side of the brain only. These may be caused by car accidents, falls, acts of violence, and other factors.
- Cardiovascular problems, particularly aneurysms and hemorrhages in the brain.
- Infections, particularly encephalitis and meningitis. Some serious infections, particularly sepsis and abscesses in the neck, may spread to the brain if left untreated.
- Migraine syndrome -> recurrent headaches of severe intensity occasionally accompanied by sensations of numbness and tingling in one half of the body.
- Conditions that cause demyelination of the brain, including multiple sclerosis and some other autoimmune diseases.
- Reactions to surgery, medication, or anesthesia.
- Loss of oxygen to the brain due to choking or anaphylactic shock.
- Brain cancers.
- Lesions in the brain, even if non-cancerous, since these lesions can impede function on one side of the brain.
- Congenital abnormalities, including cerebral palsy and neonatal-onset multi-inflammatory disease.
- Rarely, psychological causes; some states of catatonia can cause hemiplegia, and people with parasomnia—a sleep disorder leading to unusual nighttime behavior—may experience nighttime episodes of hemiplegia.
- Head injury
- Diabetes
- Brain tumor
- Infections –> meningitis, encephalitis, meningitis, brain abscess
- Migraine syndrome -> recurrent headaches of severe intensity occasionally accompanied by sensations of numbness and tingling in one half of the body.
- Inflammation of the blood vessels -> vasculitis
- Diseases affecting the nerves -> like Multiple Sclerosis; acute necrotizing myelitis.
- Conditions presenting from birth -> cerebral palsy. Lack of blood supply damages nerve cells in the brain. Birth trauma, difficult labor, perinatal strokes in infants within 3 days of birth can all cause cerebral palsy.
- Hereditary diseases –> leukodystrophies. This is a rare disorder affecting the myelin sheath which covers and protects nerve cells in the brain. The condition usually appears in infancy or childhood.
- Vascular – cerebral hemorrhage
- Neoplastic – glioma-meningioma
- Demyelination – disseminated sclerosis, lesions to the internal capsule
- Traumatic – cerebral lacerations, subdural hematoma rare cause of hemiplegia is due to local anesthetic injections given intra-arterially rapidly, instead of given in a nerve branch.
- Congenital – cerebral palsy, Neonatal-Onset Multisystem Inflammatory Disease (NOMID)
- Disseminated – multiple sclerosis
- Psychological – parasomnia (nocturnal hemiplegia)
- Severe headache
- Impairment or loss of vision
- Memory loss
- Confusion
- Loss of balance or co-ordination
- Poor balance and dizziness
- Sudden numbness, paralysis or weakness of an arm, leg or side of the face.
- Slurred or abnormal speech
- Loss of consciousness
- Incontinence
Symptoms of Facial Hemiplegia
The main symptom of hemiplegia is weakness or paralysis on one side of the child’s body. The condition can vary in severity and affects each child differently. It will only affect one side of the child’s body. General symptoms include
- Total or partial loss of sensation on just one side.
- Changes in cognition, mood, or perception.
- Difficulty speaking.
- Changes on the other side of the body, since those muscles, may begin to atrophy or become painful due to chronic muscle spasms.
- Spastic attacks during which the muscles move without your conscious control.
- Seizures.
- Pusher syndrome – With this symptom, hemiplegics shift their weight to the paralyzed side of the body, resulting in significant loss of motor control.
- Severe, throbbing pain, often on one side of your head
- A pins-and-needles feeling, often moving from your hand up your arm
- Numbness on one side of your body, which can include your arm, leg, and half of your face
- Weakness or paralysis on one side of your body
- Loss of balance and coordination
- Dizziness or vertigo
- Nausea and vomiting
You may also have problems with your senses, communication, and drowsiness
- Seeing zigzag lines, double vision, or blind spots
- Extreme sensitivity to light, sound, and smell
- Language difficulties, such as mixing words or trouble remembering a word
- Slurred speech
- Confusion
- Loss of consciousness or coma
- Difficulty walking
- Poor balance
- Little or no use of one hand or leg
- Speech problems
- Visual problems
- Behavioral problems
- Learning difficulties
- Epilepsy
- Developmental delay, for example learning to walk later than other children
amzn_assoc_placement = “adunit0”;
amzn_assoc_search_bar = “false”;
amzn_assoc_tracking_id = “raharun-20”;
amzn_assoc_ad_mode = “search”;
amzn_assoc_ad_type = “smart”;
amzn_assoc_marketplace = “amazon”;
amzn_assoc_region = “US”;
amzn_assoc_title = “Shop Related Products”;
amzn_assoc_default_search_phrase = “stroke home machine “;
amzn_assoc_default_category = “All”;
amzn_assoc_linkid = “8bd8f033dd014012f0966d32f581235c”;
Diagnosis of Facial Hemiplegia
To diagnose a stroke doctor hemiplegia will usually make an assessment using several of the following
- Examination of current signs and symptoms
- Review of medical history
- Electrocardiogram (ECG) – measures electrical activity in the heart
- Echocardiogram – to assess for any abnormalities in heart function and structure
- Electroencephalogram (EEG) – measures electrical activity in the brain
- Ultrasound scanning – of the neck arteries (carotids)
- Computerized tomography (CT) scan – specialized x-rays that can provide detailed cross-sectional images of the brain
- Magnetic resonance imaging (MRI) – a specialized scan that produces a detailed image of the brain
- Blood tests
- Chest x-rays.
Treatment of Facial Hemiplegia
Some potential hemiplegia exercises to consider include
- Strength Training Exercises – Some strength training exercises can prove to be beneficial for hemiplegics. The training recommended may vary depending on the type of hemiplegia, but common exercises include knee rolling, single-leg dropouts, and single-leg bridges, among others. In some cerebral hemiplegia patients, this can help improve range of motion and functionality in the affected limbs—though this isn’t certain.
- Muscle Stretches – Stretching specific muscle groups helps hemiplegics stave off some of the side effects of hemiplegia, such as joint/muscle pain from not moving limbs for too long and muscular atrophy. Spastic hemiplegics may need assistance in safely moving their contracted muscles without injury.
- Seated Aerobics – Seated aerobics provide a relatively safe way to burn calories and improve health from virtually anywhere. This form of exercise is recommended for hemiplegics recovering from a spinal cord injury.
- Water Aerobics – This hemiplegia exercise allows hemiplegics to relax their muscles and support the full weight of their bodies relatively easily as they stretch and work on their range of motion. Some rehabilitation programs use water aerobics as a chance to help people with paralysis to get out of the chair and experience some freedom of movement as they work muscles that are often neglected during in-chair exercises.
- Muscle relaxant – that help to increase muscle strength. It can be done either by any drugs or manually applying heat and electromagnetic radiation.
- Physical therapy – designed to help the brain work around the injuries. Physical therapy can also strengthen the unaffected side and help you reduce the loss of muscle control and tone.
- Support groups – family education, and advocacy by family support, friend circle, etc.
- Psychotherapy – to help you deal with the psychological effects of the disease.
- Exercise therapy – to help you remain healthy in spite of your disability.
Initial Treatment of Hemiplegia
Immediate treatment is aimed at limiting the size of the stroke and preventing further stroke. Acute stroke therapies try to stop a stroke while it is happening by quickly dissolving the blood clot causing an ischaemic stroke or by stopping the bleeding of a hemorrhagic stroke. This will involve administering medications and may involve surgery in some cases.
Medications

RX
- Thrombolytic therapy – These medications dissolve blood clots allowing blood flow to be re-established
- Anticoagulants (eg: heparin) or aspirin – These medications help to prevent blot clots from getting bigger and prevent new blood clots from forming
- Antihypertensives – In cases of hemorrhagic stroke these medications may be prescribed to help lower high blood pressure
- Medications– to reduce swelling in the brain and medications to treat underlying causes for the stroke eg: heart rhythm disorders may also be given.
- Blood thinners – to reduce cardiovascular blockages and decrease the chances of future strokes.
- Antibiotics – usually delivered intravenously, to combat brain infections.
- Muscle relaxant drugs – Tolperisone or eperisone hcl
- Surgery to address secondary issues-particularly involuntary muscle contractions, spinal damage, or damage to the ligaments or tendons on the unaffected side of the body.
- Physical therapy – designed to help the brain work around the injuries. Physical therapy can also strengthen the unaffected side and help you reduce the loss of muscle control and tone.
- Support groups – family education, and advocacy.
- Psychotherapy to help you deal with the psychological effects of the disease.
- Exercise therapy to help you remain healthy in spite of your disability.
amzn_assoc_placement = “adunit0”;
amzn_assoc_search_bar = “false”;
amzn_assoc_tracking_id = “raharun-20”;
amzn_assoc_ad_mode = “search”;
amzn_assoc_ad_type = “smart”;
amzn_assoc_marketplace = “amazon”;
amzn_assoc_region = “US”;
amzn_assoc_title = “Shop Related Products”;
amzn_assoc_default_search_phrase = “stroke rehab equipment”;
amzn_assoc_default_category = “All”;
amzn_assoc_linkid = “a38e31d09cae256cbcced58ec6497a3a”;
Treatment of Facial Hemiplegia
Brain cells do not generally regenerate. Following a stroke, surviving brain cells can take over the function of areas that are dead or damaged, but only to a certain degree. The adaptive ability of the brain requires the relearning of various skills. As each person who suffers a stroke is affected differently, individual rehabilitation plans are developed in conjunction with the patient, family, and healthcare team. These aim to teach skills and maximize function so that the person can achieve maximum independence.
Physiotherapy
Treatment of hemiplegia requires coordination of several health professionals. A physiotherapist, occupational therapist, a physician, a surgeon and support from family, etc.
- Treatment is focused – to find the causative factor and check its further progression. Secondly, after a few days, rehabilitation therapy helps to minimize disability.
- Several medicines – are prescribed to control the primary cause such as antihypertensive, anti-thrombolytic agents to dissolve the clot, drugs to control cerebral edema, etc.
- Intensive physical therapy – is begun after a few days. Activities such as walking, standing are done repeatedly under the guidance of a physiotherapist. It helps to improve the muscular functions which have become rigid. It is aimed to make the patient self-sufficient to perform his daily activities.
- The patient is taught – to move his affected arm with his strong arm. With exercise, it is possible to maintain the flexibility of joints and it also prevents tightening and shortening of muscles. Speech therapy is simultaneously begun to improve communication and speaking skills.
- Speech therapy – to improve communication
- Occupational therapy – to improve daily functions such as eating, cooking, toileting, and washing.
Occupational therapy
- Occupational therapy – Occupational Therapists may specifically help with hemiplegia with tasks such as improving hand function, strengthening the hand, shoulder, and torso, and participating in activities of daily living (ADLs), such as eating and dressing.
- Therapists – may also recommend a hand splint for active use or for stretching at night. Some therapists actually make the splint; others may measure your child’s hand and order a splint. OTs educate patients and family on compensatory techniques to continue participating in daily living, fostering independence for the individual – which may include, environmental modification, use of adaptive equipment, sensory integration, etc.
Rehabilitation & Therapy for Hemiplegia
1. Improving motor control
a. Neurofacilitatory Techniques
In Stroke Physical Therapy these therapeutic interventions use sensory stimuli (e.g. quick stretch, brushing, reflex stimulation, and associated reactions), which are based on neurological theories, to facilitate movement in patients following stroke. The following are the different approaches
- Bobath Concept- Berta & Karel Bobath’s approach focuses to control responses from the damaged postural reflex mechanisms. Emphasis is placed on affected inputs facilitation and normal movement patterns (Bobath, 1990).
- ii.Brunnstrom – Brunnstrom approach is one form of neurological exercise therapy in the rehabilitation of stroke patients. The relative effectiveness of Neuro-developmental treatment versus the Brunnstrom method was studied by Wagenaar and colleagues from the perspective of the functional recovery of stroke patients. The result of this study showed no clear differences in the effectiveness of the two methods within the framework of functional recovery.
- iii.Rood – Emphasise the use of activities in developmental sequences, sensation stimulation, and muscle work classification. Cutaneous stimuli such as icing, tapping, and brushing are employed to facilitate activities.
- iv. Proprioceptive neuromuscular facilitation (PNF) – Developed by Knott and Voss, they advocated the use of peripheral inputs as stretch and resisted movement to reinforce existing motor response. Total patterns of movement are used in the treatment and are followed in a developmental sequence.
b. Learning theory approach
- i. Conductive education – In Stroke Physical Therapy, Conductive education is one of the methods in treating neurological conditions including hemiplegic patients. Cotton and Kinsman (1984) demonstrated a neuropsychological approach using the concept of CE for adult hemiplegia. The patient is taught how to guide his movements towards each task-part of the task by using his own speech – rhythmical intention.
- ii. Motor relearning theory – Carr & Shepherd, both are Australian physiotherapists, developed this approach in 1980. It emphasizes the practice of functional tasks and the importance of relearning real-life activities for patients. Principles of learning and biomechanical analysis of movements and tasks are important. There is no evidence adequately supporting the superiority of one type of exercise approach over another. However, the aim of the therapeutic approach is to increase physical independence and to facilitate the motor control of skill acquisition and there is strong evidence to support the effect of rehabilitation in terms of improved functional independence and reduced mortality.
c. Functional electrical stimulation (FES)
- FES is a modality that applied a short burst of electrical current to the hemiplegic muscle or nerve. In Stroke Physical Therapy, FES has been demonstrated to be beneficial to restore motor control, spasticity, and reduction of hemiplegic shoulder pain and subluxation. A recent meta-analysis of the randomized controlled trial study showed that FES improves motor strength. A study by Faghri has identified that FES can significantly improve arm function, electromyographic activity of posterior deltoid, the range of motion and reduction of severity of subluxation and pain of the hemiplegic shoulder.
d. Biofeedback
- Biofeedback is a modality that facilitates the cognizant of electromyographic activity in selected muscle or awareness of joint position sense via visual or auditory cues. In Stroke Physical Therapy the result of studies in biofeedback is controversial. A meta-analysis of 8 randomized controlled trials of biofeedback therapy demonstrated that electromyographic biofeedback could improve motor function in stroke patients.
- A conflicting meta-analysis study by showing that biofeedback was not efficacious in improving the range of motion in the ankle and shoulder in a stroke patient. Moreland conducted another meta-analysis that concluded that EMG biofeedback alone or with conventional therapy did not superior to conventional physical therapy in improving upper- extremity function in the adult stroke patient.
2. Hemiplegic shoulder management
Shoulder subluxation and pain of the affected arm is not uncommon in at least 30% of all patient after stroke, whereas subluxation is found in 80% of stroke patients. It is associated with the severity of the disability and is common in patients in rehabilitation settings. Suggested interventions are as follows:
- a. Exercise – Active weight-bearing exercise can be used as a means of improving motor control of the affected arm; introducing and grading tactile, proprioceptive, and kinesthetic stimulation; and preventing edema and pain. In Stroke Physical Therapy, Upper extremity weight bearing can be used to lengthen or inhibit tight or spastic muscles while simultaneously facilitating muscles that are not active (Donatelli, 1991). According to Robert (1992), the amount of shoulder pain in hemiplegia was related most to loss of motion. He advocated that the provision of ROM exercise (caution to avoid improvement) as treatment as early as possible.
- b. Functional electrical stimulation – Functional electrical stimulation (FES) is an increasingly popular treatment for hemiplegic stroke patients. It has been applied in stroke physical therapy for the treatment of shoulder subluxation spasticity and functionally, for the restoration of function in the upper and lower limb. In Stroke Physical Therapy, Electrical stimulation is effective in reducing pain and severity of subluxation, and possibly in facilitating recovery of arm function
- c. Positioning & proper handling – In Stroke Physical Therapy, proper positioning and handling of the hemiplegic shoulder, whenever in bed, sitting and standing or during lifting, can prevent shoulder injury is recommended in the AHCPR & SIGN guidelines for stroke rehabilitation. In Stroke Physical Therapy, positioning can be therapeutic for tone control and neuro-facilitation of stroke patients (Davies, 1991). Braus et al 94 found shoulder hand syndrome reduced from 27% to 8% by the instruction to everyone including family on handling technique.
- d. Neuro-facilitation
- e. Passive limb physiotherapy – Maintenance of a full pain-free range of movement without traumatizing the joint and the structures can be carried out. In Stroke Physical Therapy, at no time should pain in or around the shoulder joint be produced during treatment.
- f. Pain relief physiotherapy – Passive mobilization as described by Maitland can be useful in gaining relief of pain and range of movement. In Stroke Physical Therapy other treatment modalities such as thermal, electrical, cryotherapy, etc. can be applied for shoulder pains or musculoskeletal in nature.
- g. Reciprocal pulley – The use of reciprocal pulley appears to increase the risk of developing shoulder pain in stroke patients. It is not related to the presence of subluxation or to muscle strength.
- h. Sling – In Stroke Physical Therapy the use of a sling is controversial. No shoulder support will correct a glenohumeral joint subluxation. However, it may prevent the flaccid arm from hanging against the body during functional activities, thus decreasing shoulder joint pain. They also help to relieve downward traction on the shoulder capsule caused by the weight of the arm.
3. Limb physiotherapy
- Limb physiotherapy/Stroke Physical Therapy includes passive, assisted-active and active range-of-motion exercise for the hemiplegic limbs. This can be effective management for the prevention of limb contractures and spasticity and is recommended within AHCPR. Self-assisted limb exercise is effective for reducing spasticity and shoulder protection. Adams and coworkers recommended passive full-range-of-motion exercise for a paralyzed limb for potential reduction of complication for stroke patients
4. Chest physiotherapy
- In Stroke Physical Therapy, evidence shows that both cough and forced expiratory technique (FET) can eliminate induced radio aerosol particles in the lung field. Directed coughing and FET can be used as a technique for bronchial hygiene clearance in stroke patients.
5. Positioning
- In Stroke, Physical Therapy consistent “reflex-inhibitory” patterns of posture in resting is encouraged to discourage physical complication of stroke and to improve recovery (Bobath, 1990).
- Meanwhile, therapeutic positioning is a widely advocated strategy to discourage the development of abnormal tone, contractures, pain, and respiratory complications. It is an important element in maximizing the patient’s functional gains and quality of life.
6. Tone management
- A goal of Stroke Physical Therapy interventions has been to “normalize tone to normalize movement.” Therapy modalities for reducing tone include stretching, prolonged stretching, passive manipulation by therapists, weight-bearing, ice, contraction of muscles antagonistic to spastic muscles, splinting, and casting.
- Research on tone-reducing techniques has been hampered by the inadequacies of methods to measure spasticity and the uncertainty about the relationship between spasticity and volitional motor control.
- The manual stretch of finger muscles, pressure splints, and dantrolene sodium do not produce apparent long-term improvement in motor control. Dorsal resting hand splints reduced spasticity more than volar splints, but the effect on motor control is uncertain while TENS stimulation showed improvement for chronic spasticity of lower extremities.
7. Sensory re-education
- Bobath and other therapy approaches recommend the use of sensory stimulation to promote the sensory recovery of stroke patients.
8. Balance retraining
- Re-establishment of balance function in patients following stroke has been advocated as an essential component in the practice of stroke physical therapy. Some studies of patients with hemiparesis revealed that these patients have a greater amount of postural sway, the asymmetry with greater weight on the non-paretic leg, and a decreased ability to move within a weight-bearing posture. Meanwhile, research has demonstrated moderate relationships between balance function and parameters such as gait speed, independence, wheelchair mobility, reaching, as well as dressing. Some tenable support on the effectiveness of treatment of disturbed balance can be found in studies comparing the effects of balance retraining plus physiotherapy treatment and physiotherapy treatment alone.
9. Fall prevention
- In Stroke Physical Therapy, falls are one of the most frequent complications and the consequences of which are likely to have a negative effect on the rehabilitation process and its outcome.
- According to the systematic review of the Cochrane Library, which evaluated the effectiveness of several fall prevention interventions in the elderly, there was significant protection against falling from interventions that targeted multiple, identified, risk factors in individual patients. The same is true for interventions which focused on behavioral interventions targeting environmental hazards plus other risk factors
10. Gait re-education
- Recovery of independent mobility is an important goal for the immobile patient, and much therapy is devoted to gait-reeducation. Bobath assumes abnormal postural reflex activity is caused by dysfunction so gait training involved tone normalization and preparatory activity for gait activity.
- In contrast, Carr and Shepherd advocate task-related training with methods to increase strength, coordination and flexible MS system to develop skill in walking while Treadmill training combined with the use of a suspension tube. Some patient’s body weight can effective in regaining walking ability when used as an adjunct to convention therapy 3 months after active training.
11. Functional Mobility Training
- To handle the functional limitations of stroke patients, functional tasks are taught to them based on movement analysis principles. In Stroke Physical Therapy these tasks include bridging, rolling to sit to stand and vice versa, transfer skills, walking and staring, etc.
- Published studies report that many patients improve during rehabilitation. The strongest evidence of benefit is from studies that have enrolled patients with chronic deficits or have included a no-treatment control group.
- Meanwhile, early mobilization helps prevent compilations e.g. DVT, skin breakdown contracture and pneumonia. Evidence has shown better orthostatic tolerance and earlier ambulation.
12. Upper limb training
By 3 months poststroke, approximately 37% of the individuals continue to have decreased upper extremities (UE) function. Recovery of UE function lags behind that of the lower extremities because of the more complex motor skill required of the UE in daily life tasks. That means many individuals who have a stroke are at risk for a lowered quality of life. Many approaches to the physical rehabilitation of adults post-stroke exist that attempt to maximize motor skill recovery. However, the literature does not support the efficacy of any single approach. The followings are the current approaches to motor rehabilitation of the UE.
- a. Facilitation models – They are the most common methods of intervention for the deficits in UE motor skills including Bobath, proprioceptive neuromuscular facilitation, Brunnstrom’s movement therapy, and Rood’s sensorimotor approach. There is some evidence that practice based on the facilitation models can result in improved motor control of UE. However, an intervention based on the facilitation models has not been effective in restoring the fine hand coordination required for the performance of actions.
- b. Functional electric stimulation – In Stroke Physical Therapy, Functional electric stimulation (FES) can be effective in increasing the electric activity of muscles or increased active range of motion in individuals with stroke. Some evidence showed that FES may be more effective than facilitation approaches.
- c. Electromyographic biofeedback – In Stroke Physical Therapy, biofeedback can contribute to improvements in motor control at the neuromuscular and movement levels. Some studies have shown improvements in the ability to perform actions during post-testing after biofeedback training. However, the ability to generalize these skills and incorporate them into daily life is not measured.
- d. Constraint-induced therapy – Constraint-Induced (CI) therapy was designed to overcome the learned nonuse of the affected UE. In the most extreme form of CI therapy, individual post-stroke is prevented from using the less affected UE by keeping it in a splint and sling for at least 90% of their waking hours. Studies have found that the most extreme of CI therapy can effect rapid improvement in UE motor skill and that is retained for at least as long as 2 years. However, CI therapy currently is effective only in those with distal voluntary movement.
13. Mobility appliances and equipment
- Small changes in an individual’s local ‘environment’ can greatly increase independence, use of a wheelchair or walking stick. However, little research has been done for these ‘treatments’. It is acknowledged that walking aids and mobility appliances may benefit selected patients.
14. Acupuncture
- The World Health Organisation (WHO) has listed acupuncture as a possible treatment for pariesis after stroke. Studies had sown its beneficial effects on stroke rehabilitation.
- Hua had reported a significant difference in changes of neurological score between the acupuncture group and the control group after 4 weeks of treatment in an RCT and no adverse effects were observed in patients treated with acupuncture.
15. Vasomotor training
- Early stimulation of the muscle pump can reduce the venous stasis and enhance the general circulation of the body. It then hastens the recovery process.
16. Edema management
- Use of intermittent pneumatic pump, elastic stocking or bandages and massage can facilitate the venous return of the oedematous limbs. Therefore, the elasticity and flexibility of the musculoskeletal system can be maintained and enhance the recovery process and prevent complications like pressure ulcers.
Homeopathic Medicines for Hemiplegia
Homeopathic medicines cannot cure hemiplegia. However, the medicines can be administered to improve the state of paralysis, improve blood circulation, help control loss of power, improve the power of muscles to come extent and improve the overall health of the patient.
Some common medicines for hemiplegia and such states of paralysis are:
- Plumbum Metallicum – This medicine is sourced by processing and potentizing the metal lead. It helps the neuro-muscular system of the body. It is administered with the intention to improve some muscle power. Plumbum met, as it is called, may be indicated all kinds of paralysis such as hemiplegia, paraplegia, and quadriplegia. As said earlier, it cannot cure paralysis as such.
- Causticum – Similar to the above medicine, Causticum is also a friend to all paralysis patients. It is aimed at improving some muscle power and not cure it.
- Nux vomica – This herbal medicine helps in the early stages of hemiplegia and not after some months or years.
- Lathyrus sativus – This is another example of a toxin transformed into medicine. It is safe, There are some spasticity and stiffness in some muscles, in the cases of hemiplegia, where Lathyrus may be called for.
- Gelsemium – This plant remedy is useful for early cases of paralysis including hemiplegia. It is supposed to improve muscle strength in the cases of paralysis.
amzn_assoc_placement = “adunit0”;
amzn_assoc_search_bar = “false”;
amzn_assoc_tracking_id = “raharun-20”;
amzn_assoc_ad_mode = “search”;
amzn_assoc_ad_type = “smart”;
amzn_assoc_marketplace = “amazon”;
amzn_assoc_region = “US”;
amzn_assoc_title = “Shop Related Products”;
amzn_assoc_default_search_phrase = “stroke recovery machine”;
amzn_assoc_default_category = “All”;
amzn_assoc_linkid = “a38e31d09cae256cbcced58ec6497a3a”;
Prevention
Reducing the number of controllable risk factors is the best way to prevent a stroke. This can include:
- Stopping smoking
- Losing weight
- Eating a balanced diet low in sodium and saturated and trans fat
- Moderating alcohol intake (no more than 2 small drinks per day)
- Exercising regularly in order to stay physically fit
- Maintaining good control of existing medical conditions such as diabetes, high blood pressure and high cholesterol.
Referances