Pneumonia is an inflammation of the airspaces in the lung most commonly caused by infections. Bacteria, viruses, or fungi (infrequently) can cause the infection. There are also a few noninfectious types of pneumonia that are caused by inhaling or aspirating foreign matter or toxic substances into the lungs. It is generally more serious when it affects older adults, infants, and young children, those with chronic medical conditions, or those with weakened immune function.
Types by the Germ of Pneumonia
Pneumonia can be classified according to the organism that caused the infection.
Bacterial pneumonia
The most common cause of bacterial pneumonia is Streptococcus pneumoniae. Chlamydophila pneumonia and Legionella pneumophila can also cause bacterial pneumonia.
Types of Bacterial Pneumonia
-
CAP: The acute infection of lung tissue in a patient who has acquired it from the community.
-
HAP: The acute infection of lung tissue that develops 48 hours or longer after the hospitalization of a non-intubated patient.
-
VAP: A type of nosocomial infection of lung tissue that usually develops 48 hours or longer after intubation for mechanical ventilation.
-
HCAP: The acute infection of lung tissue acquired from healthcare facilities such as nursing homes, dialysis centres, and outpatient clinics or a patient with hospitalization within the past 3 months (previously included in HAP but becomes a separate category after some cases presenting as outpatients with pneumonia have been found to be infected with multidrug-resistant (MDR) pathogens previously associated with HAP).
Viral pneumonia
Respiratory viruses are often the cause of pneumonia, especially in young children and older people. Viral pneumonia is usually not serious and lasts for a shorter time than bacterial pneumonia.
Mycoplasma pneumonia
Mycoplasma organisms are not viruses or bacteria, but they have traits common to both. Mycoplasmas generally cause mild cases of pneumonia, most often in older children and young adults.
Fungal pneumonia
Fungi from soil or bird droppings can cause pneumonia in people who inhale large amounts of the organisms. They can also cause pneumonia in people with chronic diseases or weakened immune systems.
Types by the Location of Pneumonia
Pneumonia is also classified according to where it was acquired.
Hospital-acquired pneumonia (HAP)
This type of bacterial pneumonia is acquired during a hospital stay. It can be more serious than other types, because the bacteria involved may be more resistant to antibiotics.
Community-acquired pneumonia (CAP)
This refers to pneumonia that is acquired outside of a medical or institutional setting.
Aspiration pneumonia
This type of pneumonia occurs when you inhale bacteria into your lungs from food, drink, or saliva. This type is more likely to occur if you have a swallowing problem or if you become too sedate from the use of medications, alcohol, or some types of illicit drugs.
Ventilator-associated pneumonia (VAP)
When people who are using a ventilator get pneumonia, it’s called VAP.
Healthcare
Healthcare-associated pneumonia (HCAP) is an infection associated with recent exposure to the health care system including hospital, outpatient clinic, nursing home, dialysis center, chemotherapy treatment, or home care.HCAP is sometimes called MCAP (medical care–associated pneumonia).
According to Season/ Time
-
Typical pneumonia – refers to pneumonia caused by Streptococcus pneumoniae, Haemophilus influenzae, S. aureus, Group A streptococci, Moraxella catarrhalis, anaerobes and aerobic gram-negative bacteria.
-
Atypical pneumonia – is mostly caused by Legionella spp, Mycoplasma pneumoniae, Chlamydia pneumoniae, and C. psittaci.
Histopathology
Pathologically, lobar pneumonia is the acute exudative inflammation of a lung lobe. It has the following four advanced stages if left untreated:
-
Congestion: In this stage, pulmonary parenchyma is not fully consolidated, and microscopically, the alveoli have serous exudates, pathogens, few neutrophils, and macrophages.
-
Red hepatization: Here the lobe is now consolidated, firm, and liver-like. Microscopically, there is an addition of fibrin along with serous exudate, pathogens, neutrophils, and macrophages. The capillaries are congested, and the alveolar walls are thickened.
-
Gray hepatization: The lobe is still liver-like inconsistency but gray in color due to suppurative and exudative filled alveoli.
-
Resolution: After a week, it starts resolving as lymphatic drainage or a productive cough clear the exudate.
Causes of Pneumonia
- Babies and toddlers – particularly those born prematurely
- People who have had a recent viral infection – such as a cold or influenza (the flu)
- Smokers
- People with chronic lung conditions such as asthma, bronchitis or bronchiectasis
- People with suppressed immune systems
- People who drink excessive alcohol
- Patients in hospital
- People who have had swallowing or coughing problems following a stroke or other brain injury
- People aged 65 years or older.
Symptoms of Pneumonia
Symptoms of pneumonia caused by bacteria usually come on quickly. They may include:
- Cough. You will likely cough up mucus (sputum) from your lungs. Mucus may be rusty or green or tinged with blood.
- Fever.
- Fast breathing and feeling short of breath.
- Shaking and “teeth-chattering” chills.
- Chest pain that often feels worse when you cough or breathe in.
- Fast heartbeat.
- A high temperature – you might also sweat and shiver
- Difficulty breathing or getting out of breath quicker than normal
- Chest pain or discomfort
- Loss of appetite
- Feeling very tired or very weak.
- Nausea and vomiting.
- Confusion
- Low blood pressure
- Coughing up blood
- Diarrhea.
Symptoms that are seen less commonly include
- Coughing up blood
- Headaches
- Fatigue
- Nausea
- Vomiting
- Wheezing
- Joint pain
- Muscle pain
- Confusion, disorientation, especially when elderly people have pneumonia.
Diagnosis of Pneumonia
History and Physical
The history findings of bacterial pneumonia may vary from indolent to fulminant. Clinical manifestation includes both constitutional findings and findings due to damage to the lung and related tissue. The following are major history findings:
-
Fever with tachycardia and/or chills and sweats.
-
A cough may be either nonproductive or productive with mucoid, purulent or blood-tinged sputum.
-
Pleuritic chest pain, if the pleura is involved.
-
Shortness of breath with normal daily routine work.
-
Other symptoms include fatigue, headache, myalgia, and arthralgia.
Physical findings also vary from patient to patient and mainly depend on the severity of lung consolidation and existence or nonexistence of pleural effusion. The following are major clinical findings:
-
Increased respiratory rate.
-
Percussion sounds vary from flat to dull.
-
Tactile fremitus.
-
Crackles, rales, and bronchial breath sounds are heard on auscultation.
Confusion manifests earlier in older patients. A critically ill patient may present with sepsis or multi-organ failure.
Evaluation
The approach to evaluate and diagnose pneumonia depends on different modalities but primarily it is like a tripod stand which has 3 legs which are summed up as:
-
Clinical Evaluation: It includes taking a careful patient history and performing a thorough physical examination to judge the clinical signs and symptoms mentioned above.
-
Laboratory Evaluation: This includes lab values such as complete blood count with differentials, inflammatory biomarkers like ESR and C-reactive protein, blood cultures, sputum analysis or Gram staining and/or urine antigen testing or polymerase chain reaction for nucleic acid detection of certain bacteria.
Differential Diagnosis
Differential Diagnosis in Children
-
Asthma or reactive airway disease
-
Bronchiolitis
-
Croup
-
Respiratory distress syndrome
Differential Diagnosis in Adults
-
Acute and chronic bronchitis
-
Aspiration of a foreign body
-
Asthma
-
Atelectasis
-
Bronchiectasis
-
Bronchiolitis
-
Chronic obstructive pulmonary disease
-
Fungal
-
Lung abscess
-
Pneumocystis jiroveci pneumonia
-
Respiratory failure
-
Viral
Lab Test
- Blood test – This test can confirm an infection, but it may not be able to identify what’s causing it.
- Sputum test – This test can provide a sample from your lungs that may identify the cause of the infection.
- Pulse oximetry – An oxygen sensor placed on one of your fingers can indicate whether your lungs are moving enough oxygen through your bloodstream.
- Urine test – This test can identify the bacteria Streptococcus pneumoniae and Legionella pneumophila.
- Chest X-ray – This helps your doctor diagnose pneumonia and determine the extent and location of the infection. However, it can’t tell your doctor what kind of germ is causing the pneumonia.
- CT scan – This test provides a clearer and more detailed picture of your lungs.
- Fluid sample – If your doctor suspects there is fluid in the pleural space of your chest, they may take fluid using a needle placed between your ribs. This test can help identify the cause of your infection.
- Ultrasound of the chest – Ultrasound may be used if fluid surrounding the lungs is suspected. An ultrasound exam will help determine how much fluid is present and can aid in determining the cause of the fluid.
- MRI of the chest – MRI is not generally used to evaluate for pneumonia but may be used to look at the heart, vessels of the chest and chest wall structures. If the lungs are abnormal because of excess fluid, infection or tumor, an MRI may provide additional information about the cause or extent of these abnormalities.
- Needle biopsy of the lung – Your doctor may request a biopsy of your lung to determine the cause of pneumonia. This procedure involves removing several small samples from your lung(s) and examining them. Biopsies of the lung can be done using x-ray, CT, ultrasound and/or MRI.
- Bronchoscopy – This test looks into the airways in your lungs. It does this using a camera on the end of a flexible tube that’s gently guided down your throat and into your lungs. Your doctor may do this test if your initial symptoms are severe, or if you’re hospitalized and your body is not responding well to antibiotics.
- Sputum test – A sample of fluid from your lungs (sputum) is taken after a deep cough and analyzed to help pinpoint the cause of the infection.
- Pleural fluid culture – A fluid sample is taken by putting a needle between your ribs from the pleural area and analyzed to help determine the type of infection.
- Microbiology tests to identify the causative organism – Tests may be performed on blood or sputum. Rapid urine tests are available to identify Streptococcus pneumoniae and Legionella pneumophila. Cultures of blood or sputum not only identify the responsible organism but can also be examined to determine which antibiotics are effective against a particular bacterial strain.
Treatment of Pneumonia
-
Chest physiotherapy
-
Intravenous fluids (and, conversely, diuretics), if indicated
-
Pulse oximetry with or without cardiac monitoring, as indicated
-
Oxygen supplementation
-
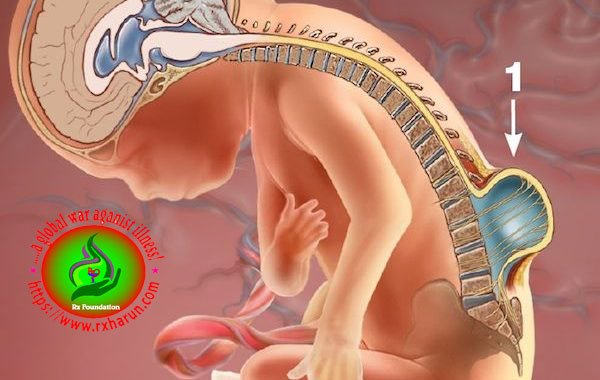
Positioning of the patient to minimize aspiration risk
-
Respiratory therapy, including treatment with bronchodilators and N-acetylcysteine
-
Suctioning and bronchial hygiene
-
Ventilation with low tidal volumes (6 mL/kg of ideal body weight) in patients requiring mechanical ventilation secondary to bilateral pneumonia or acute respiratory distress syndrome (ARDS)
-
Systemic support -May include proper hydration, nutrition, and mobilization
| Severity class | Primary treatment (standard dose) | Alternative treatment (standard dose) |
| Mild pneumonia without comorbidity, outpatient treatment | Amoxicillin (750–1000 mg tid) | Moxifloxacin (400 mg qd) Levofloxacin (500 mg qd or bid) Clarithromycin (500 mg bid) Azithromycin (500 mg qd × 3 d) Doxycycline (200 mg qd) |
| Mild pneumonia with comorbidity, outpatient treatment – Congestive heart failure – Neurologic disease with dysphagia – Severe COPD, bronchiectasis – Bedridden state, PEG |
Amoxicillin/clavulanic acid (1 g tid) | Moxifloxacin (400 mg qd) Levofloxacin (500 mg qd or bid) |
CAP,community-acquired pneumonia; COPD, chronic obstructive pulmonary disease; PEG, percutaneous endoscopic gastrostomy
| Severity class | Primary treatment (standard dose) | Alternative treatment (standard dose) |
| Moderately severe CAP (no acute organ dysfunction) |
Beta-lactam IV – Amoxicillin/clavulanic acid (2.2 g q8h) – Ampicillin/sulbactam (3 g q8h) – Cefuroxime (1.5 g q8h) – Ceftriaxone (2 g qd) – Cefotaxime (2 g q8h)+ Optional* macrolide IV or po for 3 days – Clarithromycin (500 mg q12h) – Azithromycin (500 mg qd) |
Fluoroquinolone IV or po Moxifloxacin (400 mg qd) Levofloxacin (500 mg qd or q12h) |
| Severe CAP (acute organ dysfunction) |
Beta-lactam IV – Piperacillin/tazobactam (4.5 g q6-8h) – Ceftriaxone (2 g qd) – Cefotaxime (2 g q6-8h)+ Macrolide IV for 3 days – Clarithromycin (500 mg q12h) – Azithromycin (500 mg qd) |
Fluoroquinolone IV Moxifloxacin (400 mg qd) Levofloxacin (500 mg q12h) (no monotherapy in patients with septic shock) |
* The additional administration of a macrolide is optional because prospective, placebo-controlled trials have not clearly shown that they improve the outcome
- Antibiotics – These medicines are used to treat bacterial pneumonia. It may take time to identify the type of bacteria causing your pneumonia and to choose the best antibiotic to treat it. If your symptoms don’t improve, your doctor may recommend a different antibiotic.
- Cough medicine –This medicine may be used to calm your cough so that you can rest. Because coughing helps loosen and move fluid from your lungs, it’s a good idea not to eliminate your cough completely. In addition, you should know that very few studies have looked at whether over-the-counter cough medicines lessen coughing caused by pneumonia. If you want to try a cough suppressant, use the lowest dose that helps you rest.
- Oxygen therapy – to ensure the body gets the oxygen it needs
- Intravenous fluids – to correct dehydration or if the person is too unwell to eat or drink
- Physiotherapy – to help clear the sputum from the lungs.
The following image-guided treatments may be used for pneumonia:
- Thoracentesis – Fluid may be taken from your chest cavity and studied to help your doctor determine which germ is causing your illness. X-ray, CT and/or ultrasound may be used during thoracentesis. The fluid removed during this procedure may also help provide symptom relief.
- Chest tube placement – During this procedure, also known as thoracostomy, a thin plastic tube is inserted into the pleural space (the area between the chest wall and lungs. The tube can help remove excess fluid or air. The procedure is performed under the guidance of CT or ultrasound.
- Image-guided abscess drainage – Image-guidance helps direct placement of a needle into the abscess cavity and can aid during insertion of a drainage tube. If an abscess has formed in the lungs, it may be drained by inserting a small drainage tube (catheter). Image guidance, including fluoroscopy, x-ray, ultrasound or CT, is used.
Vaccines
Two types of pneumonia vaccines are available in the United States. Your doctor can tell you which one might be better for you.
Prevnar 13: This vaccine is effective against 13 types of pneumococcal bacteria. The Centers for Disease Control and Prevention (CDC) recommends this vaccine for:
- babies and children under the age of 2
- adults ages 65 years or older
- people between ages 2 and 65 years with chronic conditions that increase their risk of pneumonia
Pneumovax 23: This vaccine is effective against 23 types of pneumococcal bacteria. The CDC recommends it for:
- adults ages 65 years or older
- adults ages 19–64 years who smoke
- people between ages 2 and 65 years with chronic conditions that increase their risk of pneumonia
Pathogen-Driven Antibiotic Choices
| Organism | First-Line Antimicrobials | Alternative Antimicrobials | |
| Streptococcus pneumoniae | |||
| Penicillin susceptible
(MIC < 2 mcg/mL) |
Penicillin G, amoxicillin | Macrolide, cephalosporin (oral or parenteral), clindamycin, doxycycline, respiratory fluoroquinolone | |
| Penicillin resistant
(MIC ≥2 mcg/mL) |
Agents chosen on the basis of sensitivity | Vancomycin, linezolid, high-dose amoxicillin (3 g/d with MIC ≤4 mcg/mL | |
| Staphylococcus aureus | |||
| Methicillin susceptible | Antistaphylococcal penicillin | Cefazolin, clindamycin | |
| Methicillin resistant | Vancomycin, linezolid | Trimethoprim- sulfamethoxazole | |
| Haemophilus influenzae | |||
| Non–beta-lactamase producing | Amoxicillin | Fluoroquinolone, doxycycline, azithromycin, clarithromycin | |
| Beta-lactamase producing | Second- or third-generation cephalosporin, amoxicillin/clavulanate | Fluoroquinolone, doxycycline, azithromycin, clarithromycin | |
| Mycoplasma pneumoniae | Macrolide, tetracycline | Fluoroquinolone | |
| Chlamydophila pneumoniae | Macrolide, tetracycline | Fluoroquinolone | |
| Legionella species | Fluoroquinolone, azithromycin | Doxycycline | |
| Chlamydophila psittaci | Tetracycline | Macrolide | |
| Coxiella burnetii | Tetracycline | Macrolide | |
| Francisella tularensis | Doxycycline | Gentamicin, streptomycin | |
| Yersinia pestis | Streptomycin, gentamicin | Doxycycline, fluoroquinolone | |
| Bacillus anthracis(inhalational) | Ciprofloxacin, levofloxacin, doxycycline | Other fluoroquinolones, beta-lactam (if susceptible), rifampin, clindamycin, chloramphenicol | |
| Enterobacteriaceae | Third-generation cephalosporin, carbapenem | Beta-lactam/beta-lactamase inhibitor, fluoroquinolone | |
| Pseudomonas aeruginosa | Antipseudomonal beta-lactam plus ciprofloxacin, levofloxacin, or aminoglycoside | Aminoglycoside plus ciprofloxacin or levofloxacin | |
| Bordetella pertussis | Macrolide | Trimethoprim- sulfamethoxazole | |
| Anaerobe (aspiration) | Beta-lactam/beta-lactamase inhibitor, clindamycin | Carbapenem | |
| MIC = Minimal inhibitory concentration. |
References