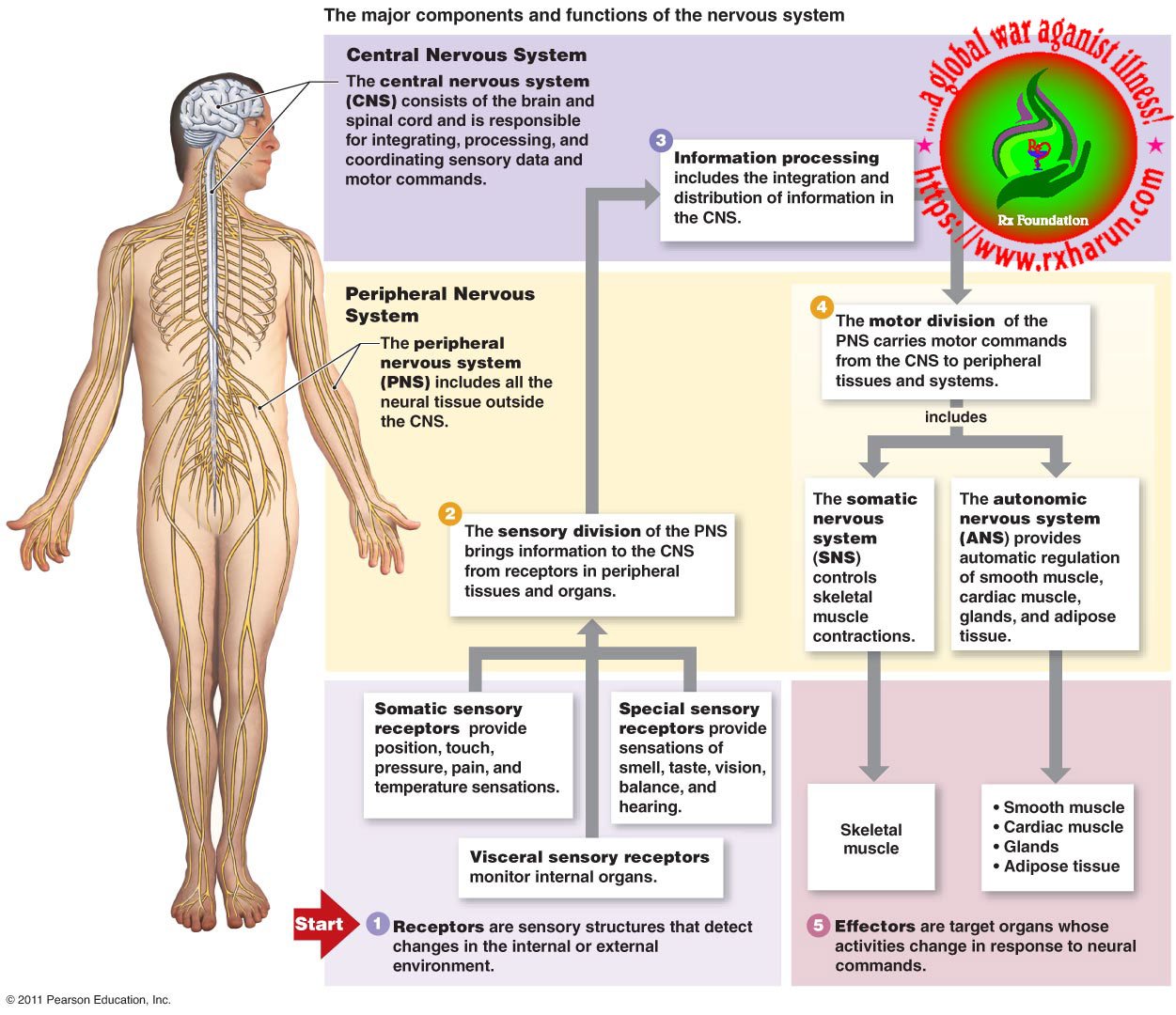
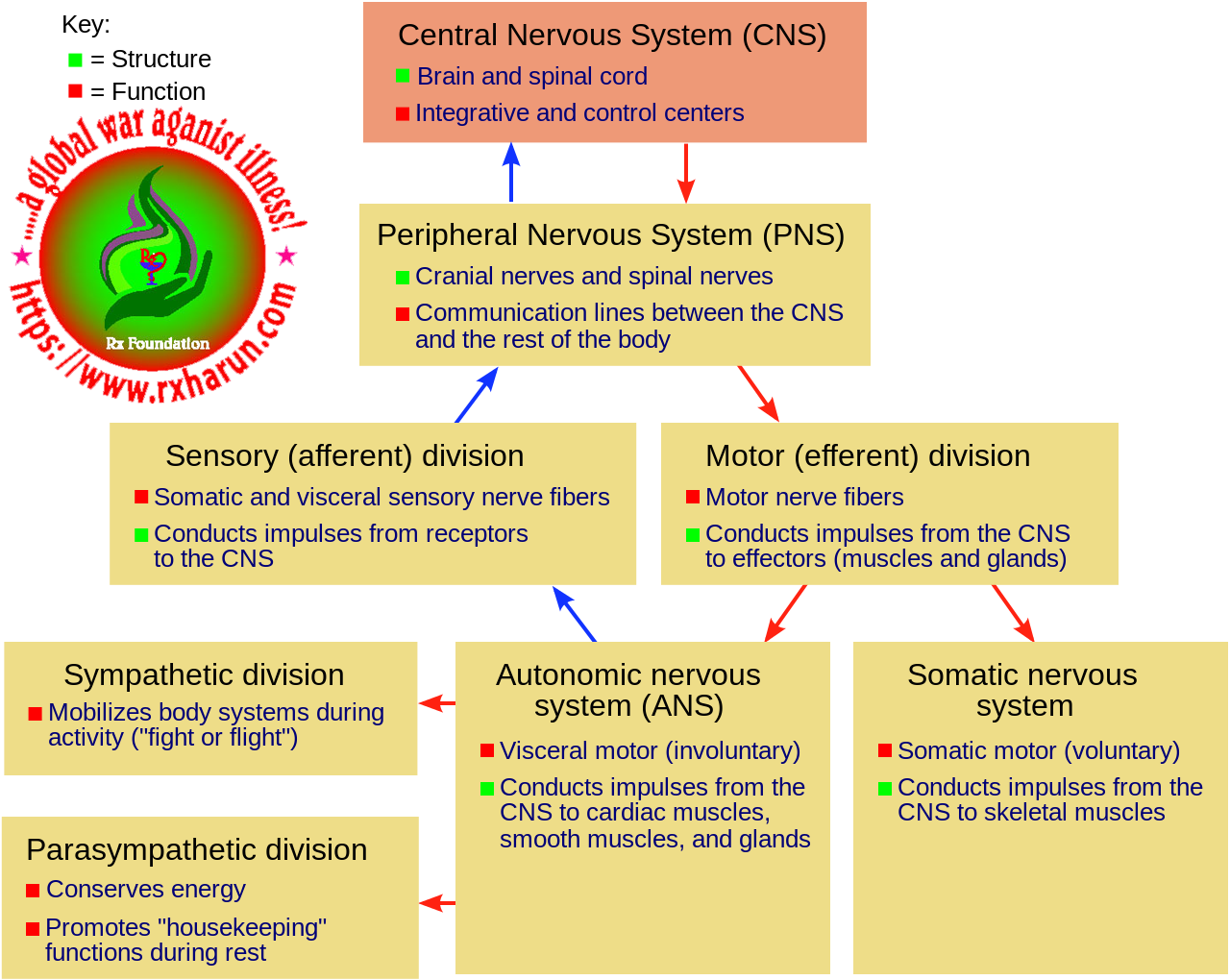
Multiple sclerosis (MS) is a disorder of the central nervous system marked by weakness, numbness, a loss of muscle coordination, and problems with vision, speech, and bladder control. Multiple sclerosis is thought to be an autoimmune disease in which the body’s immune system destroys myelin.
It is a demyelinating disease in which the insulating covers of nerve cells in the brain and spinal cord are damaged. When this occurs, axons (the parts of the nerve cells that conduct impulses to other cells), don’t work as well. Myelin acts like insulation on electrical wires. As more areas or nerves are affected by this loss of myelin, patients develop symptoms because the ability of axons to conduct impulses is diminished or lost. This damage disrupts the ability of parts of the nervous system to communicate, resulting in a range of signs and symptoms, including physical, mental, and sometimes psychiatric problems. Specific symptoms can include double vision, blindness in one eye, muscle weakness, trouble with sensation, or trouble with coordination. MS takes several forms, with new symptoms either occurring in isolated attacks (relapsing forms) or building up over time (progressive forms)
Types of Multiple Sclerosis
Currently, the United States National Multiple Sclerosis Society and the Multiple Sclerosis International Federation describes four types of MS (revised in 2013)
- Clinically isolated syndrome (CIS)
- Relapsing-remitting MS (RRMS) – Relapsing-remitting multiple sclerosis (RRMS) is the most common form of MS. People with this form of the disease develop symptoms that respond to treatment and then resolve. The development of symptoms is often referred to as an exacerbation of the disease. Episodes of remission may last for weeks to years.
- Primary progressive MS (PPMS) – Primary-progressive multiple sclerosis (PPMS) progresses over time, without episodes of remission or improvement of symptoms.
- Secondary progressive MS (SPMS) – Secondary-progressive multiple sclerosis (SPMS) is diagnosed when the problems caused by an exacerbation don’t fully resolve during a remission. This often occurs in patients who were initially diagnosed with RRMS. Over time, patients are identified with progressive debility.
- Progressive-relapsing multiple sclerosis (PRMS) – Progressive-relapsing multiple sclerosis (PRMS) is identified when patients experience escalating symptoms over time, as well as intermittent episodes of remission.
According to the duration/ onset of action
Primary progressive MS – occurs in approximately 10–20% of individuals, with no remission after the initial symptoms. It is characterized by progression of disability from onset, with no, or only occasional and minor, remissions and improvements. The usual age of onset for the primary progressive subtype is later than of the relapsing-remitting subtype. It is similar to the age that secondary progressive usually begins in relapsing-remitting MS, around 40 years of age.
Secondary progressive MS – occurs in around 65% of those with initial relapsing-remitting MS, who eventually have progressive neurologic decline between acute attacks without any definite periods of remission. Occasional relapses and minor remissions may appear. The most common length of time between disease onset and conversion from relapsing-remitting to secondary progressive MS is 19 years.
Other, unusual types of MS – have been described; these include Devic’s disease, Balo concentric sclerosis, Schilder’s diffuse sclerosis, and Marburg multiple sclerosis. There is a debate on whether they are MS variants or different diseases. Multiple sclerosis behaves differently in children, taking more time to reach the progressive stage.
Causes of Multiple Sclerosis
Gender – Women are 2 to 3 times as likely as men to get the disease.
The family history of MS – A family history increases the risk of developing MS. The closer the relationship, the higher the risk. For example, if your identical twin develops the illness, your chances are about 30%. But research has shown that there is no single “MS gene.” It will take many more years to understand the role that genetics play in MS.
Race – MS appears more commonly in Caucasians than in groups of another racial origin.
Environmental factors – MS occurs most commonly in those living in northern climates, including anywhere north of Denver or Philadelphia in North America. MS is also common in Northern Europe and Japan. Where you spend the first 15 years of your life plays a crucial role in your odds of developing MS.
Vitamin D – There’s more and more evidence that low levels of vitamin D, especially before you become an adult, could be a factor in why people get MS.
Our skin makes most of our vitamin D when we’re out in the summer sun. We also get some from food like oily fish, eggs, spreads, and breakfast cereals with added vitamin D in them. You can also get extra vitamin D from supplements (but too much can be harmful).
Symptoms of Multiple Sclerosis
Multiple sclerosis symptoms are dependent on the area of the destruction of the myelin sheath protecting the nerves (demyelination).
- Bladder and bowel problems – You may have to pee more often, need to go at night, or have trouble emptying your bladder fully. Bowel issues like constipation are also common.
- Clumsiness or lack of coordination – MS can make it hard to get around. You might have trouble walking, hard time keeping your balance, changes in your gait
- Dizziness – You may feel lightheaded. You probably won’t have vertigo, that feeling that the room is spinning.
- Emotional changes and depression – It’s tough to adjust to the idea that you have a chronic disease, let alone one that’s hard to predict and that will take a physical toll. Fear of the unknown can make you anxious. Plus the disease damages nerve fibers in your brain, and that can affect your emotions. So can medications, like corticosteroids, used to treat MS.
- Eye problems – In addition to the optic neuritis that comes with CIS, MS can cause nystagmus involuntary eye movements to double vision
- Fatigue –It often comes on in the afternoon and causes weak muscles, slowed thinking, or sleepiness. It isn’t usually related to the amount of work you do. Some people with MS say they can feel tired even after a good night’s sleep.
- Heat-related problems – You might notice them as you warm up during exercise. You could feel tired and weak or have trouble controlling certain body parts, like your foot or leg. As you rest and cool down, these symptoms are likely to go away.
- Muscle spasms – They usually affect your leg muscles. They’re an early symptom for almost half the people with MS. They also affect people with progressive MS. You might feel mild stiffness or strong, painful spasms.
- Sexual troubles – These include vaginal dryness in women and erection problems in men. Both men and women may be less responsive to touch, have a lower sex drive, or have trouble reaching orgasm.
- Speech problems – MS could cause long pauses between your words and slurred or nasal speech. You might have swallowing problems as the disease advances.
- Thinking problems – It might be hard to focus from time to time. This will probably mean slowed thinking, poor attention, or fuzzy memory. Some people have severe problems that make it hard to do daily tasks, but that’s rare. MS doesn’t usually change your intellect or ability to read and understand the conversation.
- Tremors – About half of people with MS have them. They can be minor shakes or so intense it’s hard to do everyday activities.
- Trouble walking – MS can cause muscle weakness or spasms, which make it tough to walk. Balance problems, numb feet, and fatigue can also happen.
- Unusual sensations – In addition to the pins and needles sensation that’s part of CIS, you might also have severe itching, burning, stabbing, or tearing pains. You could feel a tightness around your ribs or upper belly known as the MS hug.
More common symptoms of multiple sclerosis (MS)
| Primary symptoms | More common symptoms | Sensory disturbances (numbness, tingling, itching, burning)Walking difficulties (due to fatigue, weakness, spasticity, loss of balance and tremor)Vision problems (diplopia, blurred, and pain on eye movement)Intestinal and urinary system dysfunction (constipation and bladder dysfunction)Cognitive and emotional impairment (inability to learn and depression)Dizziness and vertigoSexual problems |
| Less common symptoms | Swallowing problems (dysphagia)Speech problems (dysarthria)Breathing problems hearing lossSeizuresHeadache | |
| Secondary symptoms | Urinary tract infectionsInactivityImmobility | |
| Tertiary symptoms | Social complicationsVocational complicationsPsychological complicationsDepression | |
Early signs and symptoms are vision problems like double vision or vision loss.
Other symptoms and signs may include
- Visual changes, including loss of vision if the optic nerve has been affected
- Double vision
- A sensation or feeling of numbness, tingling, or weakness. The weakness may be mild or severe enough to cause paralysis of one side of the body
- Vertigo (a sense of spinning) or dizziness
- Lack of coordination of the arms or legs, problems with balance, problems walking, and falling
- Slurred speech
- A sense of an electrical charge traveling down the spine with neck flexion
- In some cases, a person may develop incontinence or even an inability to empty their bladder.
- As the condition progresses, some people are left with muscle spasticity or an involuntary painful contraction of certain muscles.
Diagnosis of Multiple Sclerosis
Diagnostic testing may include the following
- MRI scan – Using a contrast dye allows the MRI to detect active and inactive lesions throughout your brain and spinal cord.
- Evoked potentials test –This requires stimulation of nerve pathways to analyze electrical activity in your brain. The three types of evoked potentials doctors use to help diagnose MS are visual, brainstem, and sensory.
- Spinal tap (also called a lumbar puncture) – a test involving a long needle that’s inserted into your spine to remove a sample of fluid circulating around your brain and spinal cord
- Blood tests – Doctors use blood tests to eliminate other conditions with similar symptoms.
- Evoked potential tests – which record the electrical signals produced by your nervous system in response to stimuli. An evoked potential test may use visual stimuli or electrical stimuli, in which you watch a moving visual pattern, or short electrical impulses are applied to nerves in your legs or arms.
Treatment of Multiple Sclerosis
All immunotherapeutic drugs target relapsing-remitting MS (RRMS) and it still remains a medical challenge in MS to develop a treatment for progressive forms. The most common injectable disease-modifying therapies in RRMS include β-interferons 1a or 1b and glatiramer acetate. However, one of the major challenges of injectable disease-modifying therapies has been poor treatment adherence with approximately 50% of patients discontinuing the therapy within the first year. Herein, we go back to the basics to understand the immunopathophysiology of MS to gain insights into the development of new improved drug treatments. We present current disease-modifying therapies (interferons, glatiramer acetate, dimethyl fumarate, teriflunomide, fingolimod, mitoxantrone), humanized monoclonal antibodies (natalizumab, ofatumumb, ocrelizumab, alentuzumab, daclizumab) and emerging immune modulating approaches (stem cells, DNA vaccines, nanoparticles, altered peptide ligands) for the treatment of MS. [5]
Medications
Several disease-modifying drugs are approved for the relapsing forms of MS.
- Corticosteroids – such as oral prednisone and intravenous methylprednisolone, are prescribed to reduce nerve inflammation. Side effects may include insomnia, increased blood pressure, mood swings and fluid retention.
- Plasma exchange (plasmapheresis) – The liquid portion of the part of your blood (plasma) is removed and separated from your blood cells. The blood cells are then mixed with a protein solution (albumin) and put back into your body. Plasma exchange may be used if your symptoms are new, severe and haven’t responded to steroids.
- Interferon Beta 1a or 1b – These may slow down the progression of symptoms, but they must be used with care, as they can cause liver damage.
- Copaxone – This aims to stop the immune system from attacking myelin. It is injected once a day. Flushing and shortness of breath may occur after receiving the injection.
- Tysabri – This is used for patients who either cannot tolerate other treatments or have not benefitted from them. It increases the risk of developing multifocal leukoencephalopathy, a fatal brain infection.
- Cannabis extract – Studies have suggested that this may help relieve pain, muscles stiffness, and insomnia.
- Aubagio – This is a once-daily tablet for adults with relapsing forms of MS.
- Beta interferons – These medications are among the most commonly prescribed medications to treat MS. They are injected under the skin or into muscle and can reduce the frequency and severity of relapses.
- Ocrelizumab – This humanized immunoglobulin antibody medication is the only DMT approved by the FDA to treat both the relapse-remitting and primary progressive forms of MS. Clinical trials showed it reduced relapse rate in relapsing disease and slowed worsening of disability in both forms of the disease.
- Glatiramer acetate – This medication may help block your immune system’s attack on myelin and must be injected beneath the skin. Side effects may include skin irritation at the injection site.
- Dimethyl fumarate – This twice-daily oral medication can reduce relapses. Side effects may include flushing, diarrhea, nausea and lowered white blood cell count.
- Fingolimod – This once-daily oral medication reduces the relapse rate.
- Teriflunomide – This once-daily medication can reduce the relapse rate. Teriflunomide can cause liver damage, hair loss and other side effects. It is harmful to a developing fetus and should not be used by women who may become pregnant and are not using appropriate contraception, or their male partner.
- Natalizumab – This medication is designed to block the movement of potentially damaging immune cells from your bloodstream to your brain and spinal cord. It may be considered a first-line treatment for some people with severe MS or as a second-line treatment in others. This medication increases the risk of a viral infection of the brain called progressive multifocal leukoencephalopathy in some people.
- Alemtuzumab – This drug helps reduce relapses of MS by targeting a protein on the surface of immune cells and depleting white blood cells. This effect can limit potential nerve damage caused by the white blood cells, but it also increases the risk of infections and autoimmune disorders.
- Teriflunomide – In September 2012, the FDA approved teriflunomide (Aubagio, Genzyme Corporation, Cambridge, MA), a pyrimidine synthesis inhibitor indicated for the treatment of patients with relapsing forms of MS. It works as an immunomodulation agent that results in antiproliferative and anti-inflammatory properties which may decrease the number of activated lymphocytes in the CNS.14
- Dimethyl Fumarate – The third and latest oral medication, dimethyl fumarate (Tecfidera, Biogen Idec, Inc), was approved by the FDA in March 2013. It is indicated for the treatment of patients with relapsing forms of MS and is categorized as a fumaric acid derivative and a systemic immunomodulator. Its mechanism is not fully known, but dimethyl fumarate is thought to activate the nuclear factor (erythroid-derived 2)-like 2 (Nrf2) pathway,17which is involved in the cellular response to oxidative stress. Therefore, dimethyl fumarate reduces peripheral and central inflammatory response and protects the CNS from oxidative stress.
- Glatiramer Acetate – Glatiramer acetate (Copaxone) was originally approved in 1996 and has been available in an extended dosage form since January 2014.9 It is indicated for reducing the frequency of relapses in patients with RRMS. The exact mechanism of action is unknown, but it is thought that glatiramer acetate induces and activates T-lymphocyte suppressor cells.18
- Alemtuzumab – Alemtuzumab (Lemtrada, Genzyme Corporation) was FDA approved in November 2014 for relapsing forms of MS. It is an anti-CD52 directed monoclonal antibody that binds to CD52 antigens present on the surface of B lymphocytes, T lymphocytes, monocytes, macrophages, natural killer cells, and some granulocytes, halting their ability to enter the brain and destroy myelin.21
- Mitoxantrone – This immunosuppressant drug can be harmful to the heart and is associated with the development of blood cancers. As a result, its use in treating MS is extremely limited. Mitoxantrone is usually used only to treat severe, advanced MS.
- Daclizumab – Daclizumab (Zinbryta, Biogen Idec, Inc) received FDA approval in May 2016 for the treatment of relapsing forms of MS. It is an anti-interleukin-2 directed monoclonal antibody that binds to CD25 subunits on high-affinity interleukin-2 (IL-2) receptors to prevent signaling. Because IL-2 plays a role in activating and regulating the immune system, antagonism at IL-2 receptors may produce benefits in MS.25
- Ocrelizumab – Ocrelizumab (Ocrevus, Genentech, Inc, San Francisco, CA) was FDA approved March 2017 and is the latest medication approved for the treatment of patients with relapsing forms of MS. Ocrelizumab is also the first treatment for PPMS. Ocrelizumab is a recombinant humanized monoclonal antibody that specifically targets and depletes CD-20-positive B lymphocytes.27 Similar to alemtuzumab, antibody-dependent cellular cytolysis, and complement-mediated lysis occur, which results in a decrease of circulating immune cells.27 Recommended initial dosing for RRMS and PPMS is ocrelizumab 300 mg IV infusion followed by a second dose 2 weeks later.
Disease-modifying treatments -As of 2017, ten disease-modifying medications are approved by regulatory agencies for relapsing-remitting multiple sclerosis (RRMS). They are interferon beta-1a, interferon beta-1b, glatiramer acetate, mitoxantrone, natalizumab, fingolimod, teriflunomide, dimethyl fumarate, alemtuzumab, and ocrelizumab.
Their cost effectiveness as of 2012 is unclear. In March 2017 the FDA approved ocrelizumab, a humanized anti-CD20 monoclonal antibody, as a treatment for RRMS, with requirements for several Phase IV clinical trials.
In RRMS they are modestly effective at decreasing the number of attacks. The interferons and glatiramer acetate are first-line treatments and are roughly equivalent, reducing relapses by approximately 30%. Early-initiated long-term therapy is safe and improves outcomes. Natalizumab reduces the relapse rate more than first-line agents; however, due to issues of adverse effects is a second-line agent reserved for those who do not respond to other treatments or with severe disease
Rehabilitation of Multiple Sclerosis
Rehabilitation aims to help patients improve or maintain their ability to perform effectively at home and at work.
Physical therapy – This aims to provide people with the skills to maintain and restore maximum movement and functional ability.
Occupational therapy – The therapeutic use of work, self-care, and play activities to increase development and prevent disability.
Speech and swallowing therapy – A speech and language therapist will carry out special training.
Cognitive rehabilitation – This helps people manage specific problems in thinking and perception.
Vocational rehabilitation -This helps people with disabilities make career plans, learn job skills, get and keep a job.
Plasma exchange – Plasmapheresis involves withdrawing blood from the patient, removing the plasma, and replacing it with new plasma. The blood is then transfused back into the patient. This process removes the antibodies in the blood that are attacking parts of the patient’s body, but whether it can help patients with MS is unclear. Studies have produced mixed results.
Vitamin D and Omega-3 supplements – Researchers have found a link between vitamin D deficiency and MS, but they are still investigating whether vitamin D supplements might help in treatment. It has been suggested that omega-3 fatty acid supplements may help patients with MS, but scientists in Norway concluded that they do not.
Hyperbaric oxygen therapy – It has been suggested that hyperbaric oxygen therapy (HBOT) may help people with MS, but this is unproven.
Keywords: multiple sclerosis, RRMS, relapsing-remitting, disease-modifying agents, treatment, pharmacotherapy
References