The circulatory system, also called the cardiovascular system or the vascular system, is an organ system that permits blood to circulate and transport nutrients (such as amino acids and electrolytes), oxygen, carbon dioxide, hormones, and blood cells to and from the cells in the body to provide nourishment and help in fighting diseases, stabilize temperature and pH, and maintain homeostasis.
The heart is the organ that pumps blood through the vessels. It pumps blood directly into arteries, more specifically the aorta or the pulmonary artery. Blood vessels are critical because they control the amount of blood flow to specific parts of the body. Blood vessels include arteries, capillaries, and veins. Arteries carry blood away from the heart and can divide into large and small arteries. Large arteries receive the highest pressure of blood flow and are more thick and elastic to accommodate the high pressures. Smaller arteries, such as arterioles, have more smooth muscle which contracts or relaxes to regulate blood flow to specific portions of the body. Arterioles face a smaller blood pressure, meaning they don’t need to be as elastic. Arterioles account for most of the resistance in the pulmonary circulation because they are more rigid than larger arteries. Furthermore, the capillaries branch off of arterioles and are a single cell layer. This thin layer allows for the exchange of nutrients, gases, and waste with tissues and organs. Also, the veins transport blood back to the heart. They contain valves to prevent the backflow of blood.
Heart Circulation
Coronary circulation is the circulation of blood in the blood vessels of the heart.
Key Points
The vessels that supply blood to the myocardium are called coronary arteries and coronary veins.
The left and right coronary arteries branch off into smaller arteries, such as the important left anterior descending (LAD) coronary artery.
The vessels that deliver oxygen-rich blood to the myocardium are known as coronary arteries. The vessels that remove the deoxygenated blood from the heart muscle are known as cardiac veins.
Most tissue perfusion in the heart occurs when the coronary arteries open during diastole.
Failure of the coronary arteries to provide sufficient blood supply to the heart can lead to ischemia, angina, and myocardial infarction.
Norepinephrine will cause vasodilation in the coronary arteries but vasoconstriction in the other arteries of the body.
Myocardial infarctions are the result of ruptured atherosclerotic plaques or arterial thrombosis, which cause the death of heart tissue from prolonged ischemia.
Key Terms
- myocardial infarction: Necrosis of heart muscle caused by an interruption to the supply of blood to the heart, often as a result of prolonged ischemia.
- ischemia: Oxygen deprivation in tissues due to mechanical obstruction of the blood supply, such as by a narrowed or blocked artery or clot.
- angina: Chest pain that indicates ischemia in the heart. It may be either transient (unstable) or stable, and stable anginas typically lead to infarction.
EXAMPLES
Atherosclerotic plaques in a coronary artery will slowly occlude (block) the vessel. As the vessel diameter narrows, less blood and oxygen will pass through and a region of the myocardium will consequently not receive an adequate supply of oxygen. This could result in angina and ultimately a myocardial infarction.
Coronary circulation is the circulation of blood in the blood vessels of the heart muscle. The vessels that deliver oxygen-rich blood to the myocardium are known as coronary arteries. The vessels that remove the deoxygenated blood from the heart muscle are known as cardiac veins. The blood supply to the heart is greater than that of other body tissues since the heart has a constant metabolic demand that must be satisfied to keep the heart pumping at all times.
Coronary Circulation: Coronary arteries labeled in red text and other landmarks in blue text.
Coronary Artery Structure
The coronary arteries originate from the left side of the heart descending from the aorta. There are multiple coronary arteries derived from the larger right and left coronary arteries. For example, important coronary arteries that branch off from the larger arteries include the left anterior descending (LAD) coronary and the right posterior coronary.
Coronary arteries run both along the surface of the heart and deep within the myocardium, which has the greatest metabolic demands of all the heart tissues due to its muscle content. Epicardial coronary arteries, which run along on the surface of the heart, are capable of autoregulating vasodilation and vasoconstriction to maintain coronary blood flow at appropriate levels to fit the metabolic demands of the heart muscle. These vessels are relatively narrow and thus vulnerable to blockage, which may cause a myocardial infarction. Subendocardial coronary arteries run deep within the myocardium to provide oxygen throughout the muscle tissue of the cardiac wall.
Systole and Diastole
In systole, the ventricular myocardium contracts, generating high intraventricular pressure and compressing the subendocardial coronary vessels while allowing the epicardial coronary vessels to remain fully open. With the subendocardial coronary vessels compressed, blood flow essentially stops below the surface of the myocardium.
In diastole, the ventricular myocardium contracts, lowering the intraventricular pressure and allowing the subendocardial vessels to become open again. Due to the high pressures generated in the ventricular myocardium during systole, most myocardial tissue perfusion occurs during diastole. Additionally, catecholamines such as norepinephrine, which normally cause vasoconstriction will instead cause vasodilation within the coronary arteries. This mechanism is due to beta-adrenergic receptors in the coronary arteries and helps enable the increased cardiac output associated with fight-or-flight responses.
Myocardial Infarctions
A myocardial infarction (heart attack) may be caused by prolonged ischemia (oxygen deprivation) in the heart, which occurs due to blockage of any of the coronary arteries. Since there is very little unnecessary blood supply to the myocardium, blockage of these vessels can cause serious damage. When these vessels become blocked, the myocardium becomes oxygen-deprived, a condition called ischemia. Brief periods of ischemia in the heart are associated with intense chest pain called angina, which may either be transient if the clot breaks up on its own or stable if it does not. As the time period of ischemia increases, the hypoxic conditions cause muscle tissue to die, causing myocardial infarction (heart attack).
Myocardial infarction is one of the most common causes of death worldwide. The clots that cause the infarction are usually the result of ruptured atherosclerotic plaques that break off and occlude the coronary arteries, but arterial thrombosis from injury or pooled blood may also cause a heart attack. The tissues of the heart do not regenerate, so those that survive a myocardial infarction will generally have scar tissue in their myocardium and may be more susceptible to other heart problems in the future.
Operation of Atrioventricular Valves
The atrioventricular valves separate the atria from the ventricles and prevent backflow from the ventricles into the atria during systole.
Key Points
The atrioventricular valves, the bicuspid (mitral) and tricuspid valves, separate the atria from the ventricles.
The bicuspid valve is on the left side of the heart and the tricuspid valve is on the right side of the heart.
Blood flows through an atrioventricular (AV) valve when blood pressure in the atria becomes high during atrial systole and blood pressure in the ventricles becomes low enough during ventricular diastole, creating a blood pressure gradient.
Papillary muscles, finger-like projections from the wall of the ventricles, connect the chordate tendineae (heartstrings) to the cusps of the atrioventricular valves. This connection prevents the valve from prolapsing under pressure.
Papillary muscles, together with the chordate tendineae, make up the subvalvular apparatus.
Key Terms
- Atrioventricular valves: These valves separate the atria from the ventricles on each side of the heart and prevent backflow from the ventricles into the atria during systole. They include the mitral and tricuspid valves.
- Subvalvular apparatus: The papillary muscles and the chordae tendineae, known as the subvalvular apparatus, hold the valves closed so that they do not prolapse.
- mitral valve: The bicuspid valve that divides the left atrium and left ventricle of the heart
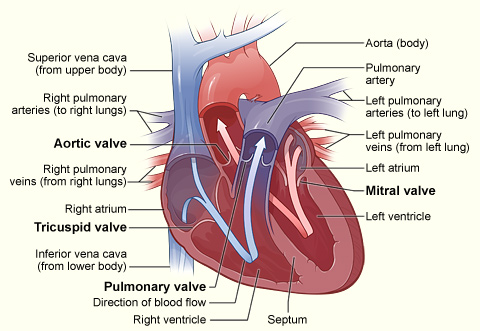
A heart valve allows blood flow in only one direction through the heart, and the combination of the atrioventricular and semi-lunar heart valves determines the pathway of blood flow. Valves open or close based on pressure differences across the valve. The atrioventricular (AV) valves separate the atria from the ventricles on each side of the heart and prevent the backflow of blood from the ventricles into the atria during systole.
Cross-section of the heart indicating heart valves: The four valves determine the pathway of blood flow (indicated by arrows) through the heart
Subvalvular Apparatus
The subvalvular apparatus describes the structures beneath the AV valves that prevent the valves from prolapsing. Valve prolapse means that the valves do not close properly, which may cause regurgitation or backflow of blood from the ventricle back into the atria, which is inefficient. The subvalvular apparatus includes the chordae tendineae and the papillary muscles. The AV valves are anchored to the wall of the ventricle by chordae tendineae (heartstrings), small tendons that prevent backflow by stopping the valve leaflets from inverting. The chordae tendineae are inelastic and attached at one end to the papillary muscles and at the other end to the valve cusps.
Papillary muscles are finger-like projections from the wall of the ventricle that anchor the chordae tendineae. This connection provides tension to hold the valves in place and prevent them from prolapsing into the atria when they close, preventing the risk of regurgitation. The subvalvular apparatus has no effect on the opening and closing of the valves, which is caused entirely by the pressure gradient of blood across the valve as blood flows from high pressure to low pressure areas.
The Mitral Valve
The mitral valve is on the left side of the heart and allows the blood to flow from the left atrium into the left ventricle. It is also known as the bicuspid valve because it contains two leaflets (cusps). The relaxation of the ventricular myocardium and the contraction of the atrial myocardium causes a pressure gradient that allows for rapid blood flow from the left atrium into the left ventricle across the mitral valve. Atrial systole (contraction) increases the pressure in the atria, while ventricular diastole (relaxation) decreases the pressure in the ventricle, causing the pressure-induced flow of blood across the valve. The mitral annulus, a ring around the mitral valve, changes in shape and size during the cardiac cycle to prevent backflow. The ring contracts at the end of the atrial systole due to the contraction of the left atrium around it, which aids in bringing the leaflets together to provide firm closure during ventricular systole.
The Tricuspid Valve
The tricuspid valve is the three-leaflet valve on the right side of the heart between the right atrium and the right ventricle and stops the backflow of blood between the two. The tricuspid valve functions similarly to the bicuspid valve except that three chordae tendineae connect the cusps of the valve to three papillary muscles, rather than the pair that connects the bicuspid valve. Blood passes through the tricuspid valve the same as it does through the bicuspid valve, based on a pressure gradient from high pressure to low pressure during systole and diastole.
The reason that the valves have different numbers of leaflets is not fully understood but may arise from differences in tissue structure and pressure that occur during fetal development.
Operation of Semilunar Valves
The semilunar valves allow blood to be pumped into the major arteries while preventing the backflow of blood from the arteries into the ventricles.
Key Points
The semilunar valves act to prevent backflow of blood from the arteries to the ventricles during ventricular diastole and help maintain pressure on the major arteries.
The aortic semilunar valve separates the left ventricle from the opening of the aorta.
The aortic and pulmonary valves are semilunar valves which separate the ventricles from the aorta and pulmonary artery, respectively.
Partial pressure gradient changes during systole and diastole cause the opening and closing of the valves.
Valve stenosis is when valves narrow and can’t open fully, while regurgitation is when they cannot close completely. In both instances, the heart must work harder to compensate for the faulty valves.
Key Terms
- semilunar valves: Located at the base of both the trunk of the pulmonary artery and the aorta, and prevent backflow of blood from the arteries into the ventricles.
- stenosis: The narrowing of valves, which prevents them from opening completely.
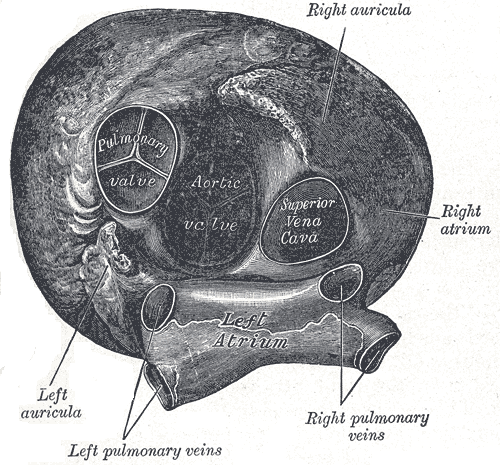
The semilunar valves are located at the connections between the pulmonary artery and the right ventricle, and the aorta and the left ventricle. These valves allow blood to be pumped forward into the arteries but prevent the backflow of blood from the arteries into the ventricles. These valves do not have subvalvular apparatus and are more similar to the semilunar valves in veins and lymphatic vessels than to atrioventricular (AV) valves.
The semilunar valves act in concert with the AV valves to direct blood flow through the heart. When the atrioventricular valves are open, the semilunar valves are shut and blood is forced into the ventricles. When the AV valves shut, the semilunar valves open, forcing blood into the aorta and pulmonary artery. The mechanism for this process depends on blood pressure gradients in the heart, which provide the force that pushes blood through the semilunar valves.
The Aortic Valve
The aortic valve separates the left ventricle from the aorta and has three cusps. During ventricular systole, pressure rises in the left ventricle. When the pressure in the left ventricle exceeds the pressure in the aorta, the aortic valve opens and blood flows from the left ventricle into the aorta. When ventricular systole ends, pressure in the left ventricle drops rapidly, and the valve closes due to a lack of pressure imposed on them from the left ventricle. Blood pressure within the aorta following systole also causes the closing of the valve. The closing of the aortic valve produces a sound that is a component of the second heart sound.
Heart viewed from above: This anterior view of the heart indicates the semilunar valves, and the aortic and pulmonary valves.
The Pulmonary Valve
The pulmonary valve (also called the pulmonic valve), which also has three cusps, separates the right ventricle from the pulmonary artery. Similar to the aortic valve, the pulmonary valve opens in ventricular systole when the pressure in the right ventricle exceeds the pressure in the pulmonary artery. When ventricular systole ends, pressure in the right ventricle drops rapidly, and the pressure in the pulmonary artery forces the pulmonary valve to close. The closure of the pulmonary valve also produces a sound, however, it is softer than the aortic sound because the blood pressure in the right side of the heart is lower compared to the left side, due to the differences between pulmonary and systemic circulation.
Valve Problems
Valves are vulnerable to several conditions that impair their normal functions. Two of the most common problems with the semilunar valves are stenosis and regurgitation. Valve stenosis refers to a narrowing of the valves, which prevents the valve from opening fully, causing an obstruction of blood flow. Valve stenosis is often caused by calcium buildup and scarring from rheumatic fever and may cause cardiac hypertrophy and heart failure. Valve regurgitation is backflow through the valves that occurs when they cannot close completely. It is the cause of most heart murmurs and is generally a minor problem, but if severe enough, it can cause heart failure. Stenosis and regurgitation can occur in both the semilunar and atrioventricular valves.
Systemic and Pulmonary Circulation
The cardiovascular system has two distinct circulatory paths, pulmonary circulation and systemic circulation.
Key Points
The cardiovascular system is composed of two circulatory paths: pulmonary circulation, the circuit through the lungs where blood is oxygenated, and systemic circulation, the circuit through the rest of the body to provide oxygenated blood.
In the pulmonary circulation, blood travels through capillaries on the alveoli, air sacs in the lungs which allow for gas exchange.
As blood flows through circulation, the size of the vessel decreases from artery/vein to arteriole/venule, and finally to capillaries, the smallest vessels for gas and nutrient exchange.
Systemic and pulmonary circulation transition to the opposite type of circulation when they return blood to the opposite side of the heart.
Systemic circulation is a much larger and higher pressure system than pulmonary circulation.
Key Terms
- alveoli: Air sacs in the lungs that provide the surface for gas exchange between the air and capillaries.
- pulmonary circulation: The part of blood circulation which carries oxygen-depleted blood away from the heart, to the lungs, and returns oxygenated blood back to the heart.
- systemic circulation: The part of blood circulation that carries oxygenated blood away from the heart, to the body, and returns deoxygenated blood back to the heart.
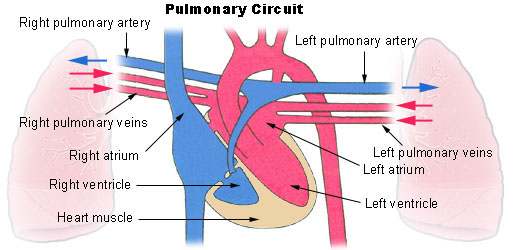
The cardiovascular system is composed of two circulatory paths: pulmonary circulation, the circuit through the lungs where blood is oxygenated; and systemic circulation, the circuit through the rest of the body to provide oxygenated blood. The two circuits are linked to each other through the heart, creating a continuous cycle of blood through the body.
Pulmonary Circulation
Pulmonary circulation is the movement of blood from the heart to the lungs for oxygenation, then back to the heart again. Oxygen-depleted blood from the body leaves the systemic circulation when it enters the right atrium through the superior and inferior venae cavae. The blood is then pumped through the tricuspid valve into the right ventricle. From the right ventricle, blood is pumped through the pulmonary valve and into the pulmonary artery. The pulmonary artery splits into the right and left pulmonary arteries and travel to each lung.
At the lungs, the blood travels through capillary beds on the alveoli where gas exchange occurs, removing carbon dioxide and adding oxygen to the blood. Gas exchange occurs due to gas partial pressure gradients across the alveoli of the lungs and the capillaries interwoven in the alveoli. The oxygenated blood then leaves the lungs through pulmonary veins, which return it to the left atrium, completing the pulmonary circuit. As the pulmonary circuit ends, the systemic circuit begins.
Alveoli: A diagram of the alveoli, showing the capillary beds where gas exchange with the blood occurs.
Pulmonary circuit: Diagram of pulmonary circulation. Oxygen-rich blood is shown in red; oxygen-depleted blood in blue.
Systemic Circulation
Systemic circulation is the movement of blood from the heart through the body to provide oxygen and nutrients to the tissues of the body while bringing deoxygenated blood back to the heart. Oxygenated blood enters the left atrium from the pulmonary veins. The blood is then pumped through the mitral valve into the left ventricle. From the left ventricle, blood is pumped through the aortic valve and into the aorta, the body’s largest artery. The aorta arches and branches into major arteries to the upper body before passing through the diaphragm, where it branches further into the iliac, renal, and suprarenal arteries which supply the lower parts of the body.
The arteries branch into smaller arteries, arterioles, and finally capillaries. Gas and nutrient exchange with the tissues occurs within the capillaries that run through the tissues. Metabolic waste and carbon dioxide diffuse out of the cell into the blood, while oxygen and glucose in the blood diffuse out of the blood and into the cell. Systemic circulation keeps the metabolism of every organ and every tissue in the body alive, with the exception of the parenchyma of the lungs, which are supplied by pulmonary circulation.
The deoxygenated blood continues through the capillaries which merge into venules, then veins, and finally the venae cavae, which drain into the right atrium of the heart. From the right atrium, the blood will travel through the pulmonary circulation to be oxygenated before returning gain to the system circulation, completing the cycle of circulation through the body. The arterial component of systemic circulation the highest blood pressure in the body. The venous component of systemic circulation has considerably lower blood pressure in comparison, due to their distance from the heart, but contains semi-lunar valves to compensate. Systemic circulation as a whole is a higher pressure system than pulmonary circulation simply because systemic circulation must force greater volumes of blood farther through the body compared to pulmonary circulation.
The nervous system regulates the cardiovascular system with the help of baroreceptors and chemoreceptors. Both receptors are located in the carotids and aortic arch. Also, both have afferent signals through the vagus nerve from the aortic arch and afferent signals through the glossopharyngeal nerve from the carotids.
-
Baroreceptors are more specifically located in the carotid sinus and aortic arch. They respond quickly to changes in blood pressure.
-
A decrease in blood pressure or blood volume causes hypotension, which leads to a decrease in arterial pressure, which creates a decrease in the stretch of the baroreceptors and decreases afferent baroreceptor signaling. This decrease in afferent signaling from the baroreceptor causes an increase in efferent sympathetic activity and a reduction in parasympathetic activity, which leads to vasoconstriction, increase heart rate, increase contractility, and an increase in BP. The vasoconstriction increases TPR in the equation MAP=CO*TPR to bring pressure (MAP) back up.
-
An increase in blood pressure or blood volume causes hypertension which increases the stretch of the baroreceptors
-
Chemoreceptors come in 2 types: peripheral and central. Peripheral chemoreceptors are specifically located in the carotid body and aortic arch. They respond to oxygen levels, carbon dioxide levels, and pH of the blood. They become stimulated when oxygen decreases, carbon dioxide increases, and the pH decreases. Central chemoreceptors are located in the medulla oblongata and measure the pH and carbon dioxide changes of the cerebral spinal fluid.
Autoregulation
Autoregulation is the method by which an organ or tissue maintains blood flow despite a change in perfusion pressure. When blood flow becomes decreased to an organ, arterioles dilate to reduce resistance.
-
Myogenic theory: Myogenic regulation is intrinsic to the vascular smooth muscle. When there is an increase in perfusion, the vascular smooth muscle stretches, causing it to constrict the artery. If there is a decrease in pressure to the arteriole, then there is decreased stretching of the smooth muscle, which would lead to the relaxation of the smooth muscles and dilation of the arteriole.
-
Metabolic theory: Blood flow is closely related to metabolic activity. When there is an increase in metabolism to muscle or any tissue, there is an increase in blood flow to that location. Metabolic activity creates substances that are vasoactive and stimulate vasodilation. The increase or decrease in metabolism leads to an increase or decrease in metabolic byproducts that cause vasodilation. Increased adenosine, carbon dioxide, potassium, hydrogen ion, lactic acid levels, and decreased oxygen levels, and increased oxygen demand all lead to vasodilation. Adenosine is from AMP, which derives from the hydrolysis of ATP and increases during hypoxia or increased oxygen consumption. Potassium is increased extracellularly during metabolic activity (muscle contraction) and has a direct effect on relaxing smooth muscles. Carbon dioxide is produced as a byproduct of the oxidative pathway and increases with metabolic activity. Carbon dioxide diffuses to vascular smooth muscle and triggers an intracellular pathway to relax the vascular smooth muscle.
-
Heart: Metabolites that cause coronary vasodilation include adenosine, NO, carbon dioxide, and low oxygen.
-
Brain: The primary metabolite controlling cerebral blood flow is carbon dioxide. An increase in arterial carbon dioxide causes vasodilation of cerebral vasculature. A decrease in arterial carbon dioxide causes vasoconstriction of the cerebral vasculature. Hydrogen ions do not cross the blood-brain barrier and thus are not a factor in regulating cerebral blood flow. A decrease in oxygen pressure in arteries causes vasodilation of the cerebral arteries; however, an increase in oxygen pressure in arteries does not cause vasoconstriction.
-
Kidneys: Autoregulation of the kidneys is myogenic and with tubuloglomerular feedback. In severe cases of hypotension, kidney arterioles constrict, and renal function is lost.
-
Lungs: Hypoxia of the lungs causes vasoconstriction, creating a shunt away from poorly ventilated areas of the lung and redirects perfusion to ventilated portions of the lung.
-
Skeletal muscle: Adenosine, potassium, hydrogen ion, lactate, and carbon dioxide all increase during exercise and cause vasodilation. When resting, the skeletal muscle is controlled extrinsically by sympathetic activity and not by metabolites.
-
Skin: Regulation of the skin occurs through sympathetic stimulation. The purpose of regulating blood flow in the skin is to regulate body temperature. In a warm environment, skin vasculature dilates due to a decrease in sympathetic stimulation. In cold environments, skin vasculature constricts due to an increase in sympathetic activity. During fever, the regulation of the body temperature is at a higher setpoint.
The starling equation can explain the capillary fluid exchange. This equation describes the forces of oncotic and hydrostatic pressure on the movement of fluid across the capillary membrane. Edema can result from an increase in capillary pressure (heart failure), a decrease in plasma proteins (liver failure), an increase in the interstitial fluid due to lymphatic blockage, or an increase in capillary permeability due to infections or burns.
Your body’s circulation system is responsible for sending blood, oxygen, and nutrients throughout your body. When blood flow to a specific part of your body is reduced, you may experience the symptoms of poor circulation. Poor circulation is most common in your extremities, such as your legs and arms.
Poor circulation isn’t a condition in itself. Instead, it results from other health issues. Therefore, it’s important to treat the underlying causes, rather than just the symptoms. Several conditions can lead to poor circulation. The most common causes include obesity, diabetes, heart conditions, and arterial issues.
Symptoms of poor circulation
The most common symptoms of poor circulation include:
- tingling
- numbness
- throbbing or stinging pain in your limbs
- pain
- muscle cramps
Each condition that might lead to poor circulation can also cause unique symptoms. For example, people with peripheral artery disease may have erectile dysfunction along with typical pain, numbness, and tingling.
There are several different causes of poor circulation.
Peripheral artery disease
Peripheral artery disease (PAD) can lead to poor circulation in your legs. PAD is a circulatory condition that causes narrowing of the blood vessels and arteries. In an associated condition called atherosclerosis, arteries stiffen due to plaque buildup in the arteries and blood vessels. Both conditions decrease blood flow to your extremities and can result in pain.
Over time, reduced blood flow in your extremities can cause:
- numbness
- tingling
- nerve damage
- tissue damage
If left untreated, reduced blood flow and plaque in your carotid arteries may result in a stroke. Your carotid arteries are the major blood vessels that deliver blood to your brain. If plaque buildup takes place in the arteries in your heart, you’re at risk of having a heart attack.
PAD is most common in adults over age 50, but it can also occur in younger people. People who smoke are at a higher risk of developing PAD early in life.
Blood clots
Blood clots block the flow of blood, either partially or entirely. They can develop almost anywhere in your body, but a blood clot that develops in your arms or legs can lead to circulation problems.
Blood clots can develop for a variety of reasons, and they can be dangerous. If a blood clot in your leg breaks away, it can pass through other parts of your body, including your heart or lungs. It may also lead to a stroke. When this happens, the results may be serious, or even deadly. If discovered before it causes a larger problem, a blood clot can often be treated successfully.
Varicose veins
Varicose veins are enlarged veins caused by valve failure. The veins appear gnarled and engorged, and they’re most often found on the back of the legs. The damaged veins can’t move blood as efficiently as other veins, so poor circulation may become a problem. Although rare, varicose veins can also cause blood clots.
Your genes largely determine whether or not you’ll develop varicose veins. If a relative has varicose veins, your risk is higher. Women are also more likely to develop them, as are people who are overweight or obese.
Diabetes
You may think diabetes only affects your blood sugar, but it can also cause poor circulation in certain areas of your body. This includes cramping in your legs, as well as pain in your calves, thighs, or buttocks. This cramping may be especially bad when you’re physically active. People with advanced diabetes may have difficulty detecting the signs of poor circulation. This is because diabetic neuropathy can cause reduced sensation in the extremities.
Diabetes can also cause heart and blood vessel problems. People with diabetes are at an increased risk for atherosclerosis, high blood pressure, and heart disease.
Obesity
Carrying around extra pounds puts a burden on your body. If you’re overweight, sitting or standing for hours may lead to circulation problems.
Being overweight or obese also puts you at an increased risk for many other causes of poor circulation, including varicose veins and blood vessel problems.
Raynaud’s disease
People who experience chronic cold hands and feet may have a condition called Raynaud’s disease. This disease causes the small arteries in your hands and toes to narrow. Narrowed arteries are less capable of moving blood through your body, so you may begin experiencing symptoms of poor circulation. The symptoms of Raynaud’s disease commonly occur when you’re in cold temperatures or feeling unusually stressed.
Other areas of your body can be affected besides your fingers and toes. Some people will have symptoms in their lips, nose, nipples, and ears.
Women are more likely to develop Raynaud’s disease. Also, people who live in colder climates are more likely to have it.
Diagnosing poor circulation
Since poor circulation is symptomatic of numerous conditions, diagnosing the condition will help your doctor diagnose the symptoms. It’s important to first disclose any known family history of poor circulation and any related diseases. This can help your doctor better assess your risk factors, as well as determine which diagnostic tests are most appropriate.
Aside from a physical exam to detect pain and swelling, your doctor may order:
- an antibodies blood test to detect inflammatory conditions, such as Raynaud’s disease
- a blood sugar test for diabetes
- blood testing to look for high levels of D dimer in the case of a blood clot
- an ultrasound or CT scan
- blood pressure tests including testing of the legs
Treating poor circulation
Treatment for poor circulation depends on the condition causing it. Methods may include:
- compression socks for painful, swollen legs
- special exercise program recommended by your doctor to increase circulation
- insulin for diabetes
- laser or endoscopic vein surgery for varicose veins
Medications may include clot-dissolving drugs, as well as blood-thinners depending on your condition. Alpha-blockers and calcium channel blockers are used to treat Raynaud’s disease.
You should discuss possible symptoms of poor circulation with your doctor. If you’re having uncomfortable symptoms, they may signal an underlying condition. Untreated conditions can lead to serious complications. Your doctor will work to determine the cause of your poor circulation and treat the underlying issue.
When caught early, diseases that lead to poor circulation are treatable. Left untreated, poor circulation may indicate a disease is in a progressive state. Life-threatening complications, such as loose blood clots, can also occur if the condition is not properly treated. Work with your doctor to start a comprehensive treatment plan that also includes a healthy lifestyle.
What’s Causing My Arms to Fall Asleep at Night?
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission.
Is this common?
The feeling is usually painless, but it can be noticeable. It’s a tingling or numbness similar to the sensation that comes when you hit your “funny bone.” When this happens to your arm or another body part, your limb is often said to have “fallen asleep.” This can happen at any time, day or night.
This isn’t an uncommon feeling. Most people experience it at one time or another. Sometimes, though, the sensation may linger for an unexpected period of time or occur alongside other symptoms. If this happens, you should consult your doctor. This sensation may be an indicator of an underlying medical concern.
Learn more about why this feeling happens, and what, if anything, you can do about it.
What causes this sensation?
This pins and needles sensation is known as paresthesia. Most of the time, the cause is simple. It may happen if you’ve lain on your arm or otherwise put pressure on it. This prevents the blood from flowing correctly to your nerves.
Poor positioning may also lead to pressure being placed directly on a nerve. The nerves react to the lack of blood flow or pinching by causing momentary tingling.
If you wake up with this feeling, readjust to relieve this pressure. Your arm will generally “wake up,” and the tingling will stop.
More chronic paresthesia may be a sign of an underlying medical issue. Possible conditions might include:
Vitamin B deficiency
There are many types of vitamin B, and they all help maintain cell health and keep you energized. Although many people get enough B vitamins through their diet, some people may also need to take supplements to meet their recommended daily amount.
If you aren’t getting enough vitamin B, you may experience paresthesia. This is most common among:
- older adults
- vegans
- people who drink alcohol excessively
- people with pernicious anemia
Fluid retention
Fluid retention can be caused by a number of things, including high salt intake and fluctuating hormone levels during menstruation. This can cause swelling to occur throughout the body or it can also be localized in certain body parts. Sometimes this swelling can disrupt circulation and trigger a tingling sensation in the affected area.
Carpal tunnel syndrome
If the numbness or tingling is also affecting your hand, it may be caused by carpal tunnel syndrome. This happens when the median nerve is compressed or pinched.
Making the same motions repeatedly, such as typing on a keyboard or working with machinery, can trigger it.
Peripheral neuropathy
If you have diabetes and are experiencing paresthesia regularly, it may be caused by nerve damage. This damage is called peripheral neuropathy and is caused by persistently high blood sugar levels.
Other conditions
Conditions affecting the central nervous system, such as multiple sclerosis and stroke, can also cause paresthesia. Tumors or growths, particularly those located in the brain or spine, may also trigger it
When should I see a doctor?
You should consult your doctor if this sensation persists beyond a brief period of readjustment, or if it’s causing significant pain or discomfort.
If you’re experiencing other symptoms along with paresthesia, you should speak with your doctor right away. These symptoms may be caused by a more serious condition.
Paresthesia that happens along with any of the following symptoms requires urgent medical attention:
- muscle weakness
- intense pain
- vision problems or vision loss
- difficulties with speech
- difficulties with coordination
- extreme dizziness
How is paresthesia treated?
If your paresthesia is infrequent, you may not need to undergo any treatment. Repositioning yourself to release pressure on the nerve may be enough to relieve any tingling or numbness that you’re experiencing.
Over-the-counter (OTC) pain medication or a cold compress can also be used to relieve any temporary or infrequent pain caused by paresthesia.
If you experience this pins and needles sensation regularly, it may be a sign of an underlying condition. Your doctor will work with you to determine the cause of your paresthesia and develop an appropriate treatment plan.
For example, if your doctor finds that you have carpal tunnel syndrome, they may recommend a wrap for wrist support and specific wrist exercises to soothe the nerve. In more severe cases, cortisone shots or surgery may be needed.
Often this feeling will go away on its own, or as the result of a minor readjustment in how you’re positioning your body.
If the issue persists, jot down when it happens, how long it lasts, and whether you’re experiencing any other symptoms. This can help your doctor determine whether a pinched nerve, a neurological issue, or other cause is behind your symptoms.
Yoga for Blood Circulation
Poor circulation can be caused by a number of things: sitting all day at a desk, high cholesterol, blood pressure issues, and even diabetes. It can also manifest in many ways, including
- numbness
- cold hands and feet
- swelling
- muscle cramps
- brittle hair and nails
- breakouts
- dark circles under your eyes
Luckily, there are almost as many ways to combat it as there are symptoms. You can try
- medication
- diet
- avoiding smoking
- exercise
Movement is key to wellness on many levels, including for circulatory health. Yoga is not only one of the most accessible types of exercise (it’s low impact and can be done by people at all levels), but it’s also one of the best types of exercise for poor circulation.
The below sequence of poses will be a great addition to your self-care and wellness routine. This is especially true if you’re dealing with circulation issues, no matter what their cause or physical manifestation in your body.
Equipment needed: Though yoga can be done without a yoga mat, one is recommended for the below sequence. It can help you maintain firm footing and is used in some of the instructions as well.
Muscles worked: hamstrings, latissimus dorsi, deltoids, glutes, serratus anterior, and quadriceps
- Start on all fours, with your shoulders above your
wrists, your hips above your knees, and toes tucked under. - Take a deep breath in, and as you exhale, press firmly
into your hands as you lift your hips into the air, straightening your
arms and legs. - For some, this may be a good stance immediately. For
others, you may want to walk your feet back just a touch so it feels
comfortable. - Breathe normally but deeply as you press into each
finger and press your heels toward the floor. Your heels may not be on the
ground here, depending on your stance, but you want them working in that
direction, keeping your legs active. - Let your neck relax, but do not let it hang.
- Stay here for three long, deep breaths. (You can repeat
this a few times, though it would be best to do the entire series a few
times, starting each time with this pose.)
Warrior II
Warrior II is wonderful for improving muscle tone in your legs. Your muscles will be compressing and releasing the veins in your legs, thus increasing effective circulation.
Muscles worked: quadriceps, piriformis, hip ligaments, scalenes, and pectoralis minor
- From Downward-Facing Dog, look between your hands and
step your right foot as close as you can get it to between your hands. If
it does not easily go between them, you can help move it forward with a
hand. - Before lifting your hands off the floor, turn your left
foot so that the outside of it runs parallel to the back edge of the mat.
Your front foot should be lined up with the toes facing forward. If you were
to run a line from the back of your right heel to the back of the mat, it
should hit the middle of your back foot. (Note: If you feel unstable in
this stance, step your right foot a bit to the right, but keep the feet
perpendicularly aligned with each other.) - Inhale deeply, and as you exhale, cartwheel your hands
as you stand. This will mean pressing firmly into your feet and beginning
with your left hand coming in front of your body, below your face, then
up, in front of, and finally behind your head, your right-hand following
until you are creating a “T” with your arms. - As you hold this pose, check your alignment: Your right
knee should be at a 90-degree angle, with your knee over your ankle,
pressing into the outside edge of your back foot. Your left leg should be
straight, your chest open to the left side of the mat, and your arms at
shoulder height. Gaze out over your right hand. - Once you’ve settled into the pose and feel comfortable
in your alignment, breath in and out deeply and slowly at least 3 times. - After your third exhalation, breathe in once more, and
when exhaling that breath, cartwheel your hands back to the ground, on
each side of your right foot. Step back to Downward-Facing Dog. Then
repeat with your left foot forward.
Triangle
Triangle is also a standing pose, so it’s another one that’s great for muscle tone and leg circulation. This pose involves opening up your chest and expanding the lungs as well, which improves circulation in your torso.
Muscles worked: sartorius, piriformis, gluteus medius, obliques, and triceps
- Begin by repeating the steps to get into Warrior II.
- Instead of settling into Warrior II, inhale as you straighten
your front leg and keep your arms aligned over your legs, in that “T.” - As you exhale, tip your torso over your right leg from
your hip, keeping your spine long and your arms in line with your
shoulders, so the “T” will tip with you. - Rest your right hand on your foot, ankle, or shin. Your
left arm should be reaching toward the sky. Your gaze can be looking at
the front foot, out to the left, or up at your left hand (if you feel like
you have the balance to do so). - Press into your feet and engage your leg muscles as you
keep your chest open to the side, breathing deeply. - After at least three deep breaths, lift your torso from
your hip using your core as you bend the front leg again. You can then
switch to the other side as you did for Warrior II. (If you are repeating
the sequence, go back to pose 1 and repeat the sequence two more times,
using the next pose as a resting pose to close out the practice.)
Legs up the wall
Putting your legs up the wall is not just an inversion in the sense that it puts your legs above your heart, but it is also an inversion of how most of us sit all day long. This position can help your blood flow normally, relieving the pooling of blood or fluid in your extremities that may happen in old age.
Muscles worked: hamstrings and neck, as well as the front of the torso
- For this pose, move your mat up against a wall where
there is space at the base, where the wall meets the floor, and far enough
up the wall that your legs can stretch up to it without knocking anything
over. - Sit parallel to the wall. Then, lie down with your feet
on the ground, knees bent. - Pivot on your lower back/upper tailbone, lifting your
feet and gently swinging your torso so it intersects the wall and hugs
your sitting bones up against the base of the wall. Once you’re
comfortable (you may have to wiggle a little), extend your legs up the
wall. You can also place a cushion or folded blanket under your lower back
if it feels better. - Rest your arms next to you, palms up. You can stay here
as long as you like.
Take it to the next level
If you feel comfortable in inversions, and if you have good balance, core strength, and yoga props, you can do a “legs in the air” pose, instead of up the wall. It will not be a resting pose in quite the same manner, but it’s great for circulation as well as the core.
- Stay on your mat and get a yoga block so it’s within
reach when you lie down. - Lie down on the mat, with your knees bent, and lift
your hips, placing the block under your sacrum. Be sure it’s firmly on the
floor and you’re firmly resting on it. - Keeping your hands alongside your body, palms pressing
into the ground, lift your knees to your chest. - Inhale deeply. As you exhale, begin to extend your legs
to the ceiling slowly and in a controlled manner. - Pressing your sacrum into the block for support, stay
here for 10 full, deep breaths before exiting in the reverse order you
entered. Bend knees into your chest and gently roll your pelvis down as
you return your feet to the ground. Then press into your feet and lift
your hips to remove the block.
The takeaway
While some circulation problems are caused by specific health conditions, many Americans deal with circulation issues and don’t know them. Why? Because we park it at our desks all day and don’t work our circulatory systems in the ways we should.
By exercising in ways that will compress and decompress the veins in our legs and access gravity in flushing stagnant blood and reversing blood flow, we can improve our circulation and stave off problems. Whether you have a diagnosed issue or not, the above yoga sequence can help your body work more effectively by improving your circulation.
Finger Numbness
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission.
What is finger numbness?
Finger numbness can cause tingling and a prickling feeling as if someone were lightly touching your fingers with a needle. Sometimes the sensation can feel slightly burning. Finger numbness may affect your ability to pick things up. And you may feel clumsy, or like you’ve lost strength in your hands.
Finger numbness can range from a symptom that occurs occasionally to something that impairs your ability to perform daily tasks. But whatever your symptoms, noninvasive treatments are often available.
What are the potential causes of finger numbness?
The nerves in your body are responsible for transmitting messages to and from your brain. If the nerves are compressed, damaged, or irritated, numbness can occur. Examples of conditions known to cause finger numbness to include:
Carpal tunnel syndrome
Carpal tunnel syndrome occurs when the nerve that provides feeling to your hand becomes pinched or obstructed. This condition often causes numbness in the thumb and index and middle fingers.
Cervical radiculopathy
Cervical radiculopathy occurs when a nerve that leaves your neck becomes inflamed or compressed. This condition can cause numbness like carpal tunnel syndrome. It’s also known as a pinched nerve.
Diabetes
A condition called diabetic neuropathy can lead to nerve damage in the feet and hands. You will usually first experience numbness in the feet.
Raynaud’s disease
Raynaud’s disease causes the small arteries in your fingers to spasm, or open and close very fast. This can cause numbness and affect your circulation.
Rheumatoid arthritis
Rheumatoid arthritis (RA) is an autoimmune disorder that causes swelling, tenderness, and pain in the joints. This condition can also lead to tingling, numbness, and burning in the hands.
Ulnar nerve entrapment
Carpal tunnel syndrome affects the median nerve in the arm, but ulnar nerve entrapment affects the ulnar nerve that runs on the little finger’s side of the arm. This most commonly causes numbness in the pinkie and ring fingers.
Less common causes of finger numbness can include
- amyloidosis
- ganglion cyst
- Guillain-Barré syndrome
- HIV
- AIDS
- Lyme disease
- multiple sclerosis (MS)
- side effects of medications, such as chemotherapy drugs
- Sjögren’s syndrome
- stroke
- syphilis
- vasculitis
- vitamin B-12 deficiency
- Hansen’s disease, or leprosy
- fractures of the wrist or hand
When is it a good idea to see a doctor?
Sometimes tingling and numbness can be symptoms of a medical emergency. This is true when a person is experiencing a stroke, which is when a blood clot or bleeding affects the brain. If you have any of the following symptoms, get medical help immediately:
- confusion
- difficulty breathing
- dizziness
- hand or finger numbness
- a severe headache
- slurred speech
- sudden weakness (asthenia) or paralysis
If your symptoms start to occur regularly, interfere with your daily activities, or cause a significant amount of pain and discomfort, see your doctor.
How is finger numbness diagnosed?
Your doctor will start diagnosing your finger numbness by taking a medical history and examining your arm, hand, and finger. In some cases, your doctor may recommend you see a medical specialist, such as an orthopedic doctor who specializes in caring for hands, or a neurologist who can test your nerve function.
Doctors commonly order an MRI when a person has finger numbness. This scan helps doctors see areas where bones in the following locations may have slipped out of place:
- neck
- shoulders
- arms
- wrists
- fingers
Bones that slip out of place can cause compression on your nerves.
Blood tests may also help a doctor diagnose conditions that cause finger numbness, such as RA or vitamin B-12 deficiency.
How is finger numbness treated?
Your doctor may recommend over-the-counter (OTC) medication to reduce inflammation. Examples include nonsteroidal anti-inflammatory drugs, such as ibuprofen.
Another option is wearing a brace or splint. This will help you keep your elbow or wrist in a good position so that the nerve is less likely to be compressed.
In rare instances, your doctor may recommend more invasive treatments if OTC options don’t work. Steroid injections can help relieve inflammation.
Surgery may decrease the nerve damage, or remove or reduce bones that are pressing on the nerve. These procedures include:
- cubital tunnel release
- ulnar nerve anterior transposition
- medial epicondylectomy
Resting your hand and wrist is usually one of the best ways to reduce inflammation when you’re at home. You can also apply ice to the affected area.
Exercises to stretch the hand and wrist can also reduce discomfort. Examples include:
- stretching out your fingers as wide as you can and holding the position for about 10 seconds
- moving your hands around in a clockwise direction about 10 times, then reversing the direction to reduce muscle tension
- rolling your shoulders backward five times, and then forward five times to keep them relaxed
Repeat these exercises throughout the day to reduce tension in your muscles.
Can finger numbness be prevented?
Several causes associated with finger numbness are due to overuse injuries. These occur when a person engages in repetitive motions that can irritate or damage the nerves and cause numbness.
Ways to avoid repetitive motion injuries include:
- practicing good posture and form when using a tool, keyboard, or another device that can result in repetitive motion injuries
- taking a break from your activity every 30 to 60 minutes
- stretching the muscles you’re using to reduce tension
- purchasing ergonomic or supportive devices, such as a wrist brace or wrist rest for a keyboard
What is the outlook for people with finger numbness?
Finger numbness is usually treatable if it isn’t accompanied by symptoms that require emergency medical attention. Rest can help reduce overuse injuries. A doctor can also recommend more specific medical treatments depending on your condition’s underlying cause.
Usually, the earlier you treat your finger numbness, the less likely the symptoms will be permanent. It’s important not to ignore your symptoms.
Best Meditation
Benefits of meditation
There are a number of benefits that come from practicing meditation. These can include:
- Reducing stress. One of the most popular reasons that people meditate is to lower stress levels, and according to science, meditation does just that. According to a 2014 study, practicing meditation can lower levels of psychological stress and is helpful for overall well-being.
- Improving sleep. If you have insomnia, one study shows that people who meditate are able to improve on their sleep schedules.
- Helping with addictions. Since meditation typically requires a fair amount of self-awareness and discipline, shows that the practice can help acknowledge and avoid triggers.
- Decreasing blood pressure. Meditation is very relaxing, and that relaxation may to lower blood pressure since your body is not responding to stress as often as it usually would.
References