The Pituitary Gland/The pituitary endocrine gland, which is located in the bony sella turcica, is attached to the base of the brain and has a unique connection with the hypothalamus. The pituitary gland consists of two anatomically and functionally distinct regions, the anterior lobe (adenohypophysis) and the posterior lobe (neurohypophysis). Between these lobes lies a small region called the intermediate lobe. The hypothalamus regulates the pituitary gland secretion.[rx][rx][rx][rx][rx]
The Anterior Pituitary (Adenohypophysis)
The anterior pituitary is derived from the embryonic ectoderm. It secretes five endocrine hormones from five different types of epithelial endocrine cells. The release of anterior pituitary hormones is regulated by hypothalamic hormones (releasing or inhibitory), which are synthesized in the cell bodies of neurons located in several nuclei that surround the third ventricle. These include the arcuate, the paraventricular and ventromedial nuclei, and the medial preoptic and paraventricular regions. In response to neural activity, the hypothalamic hormones are released from the nerve endings into the hypophyseal portal blood and are then carried down to the anterior pituitary.[rx][rx][rx]
Anterior Pituitary (AP) Hormones
Growth hormone (GH)
Other names: somatotropic hormone or somatotropin
- Precursor cells: somatotrophs in the AP
- Target cells: almost all tissues of the body
- Transport: 60% circulates free and 40% bound to specific GH-binding proteins (GHBPs)
- Mechanism of action: GH binds to growth hormone receptors (GHRs) causing dimerization of GHR, activation of the GHR-associated JAK2 tyrosine kinase, and tyrosyl phosphorylation of both JAK2 and GHR. This causes recruitment and/or activation of a variety of signaling molecules, including MAP kinases, insulin receptor substrates, phosphatidylinositol 3′ phosphate kinase, diacylglycerol, protein kinase C, intracellular calcium, and Stat transcription factors. These signaling molecules contribute to GH-induced changes in enzymatic activity, transport function, and gene expression that ultimately culminate in changes to growth and metabolism.
- Regulation of GH secretion: The release of GH is under dual control by the hypothalamus. GH secretion is stimulated by growth hormone-releasing hormone (GHRH) but suppressed by another hormone peptide, somatostatin (also known as growth hormone-inhibiting hormone (GHIH)). Insulin-like growth factor-1 (IGF-1) provides negative feedback for inhibiting GH release from somatotrophs. Thyroid hormones (T3 and T4) up-regulate GH gene expression in somatotrophs.
- Physiological Functions: GH acts almost on every type of cell. Its principal targets are bones and skeletal muscles. It has direct metabolic effects on fats, proteins, and carbohydrates and indirect actions that result in skeletal growth.
- Direct Metabolic Functions: GH is anabolic. It stimulates the growth of almost all tissues of the body that are capable of growing (increase in the number of cells). GH also increases the rate of protein synthesis in most cells of the body and decreases the rate of glucose utilization throughout the body (diabetogenic action). Also, it increases the mobilization of fatty acids from adipose tissue and increases levels of free fatty acids in the blood.
- Indirect Actions on Skeletal Growth: GH stimulates the production of IGF-1 from hepatocytes. IGF-1 mediates the growth-promoting effects of GH on the skeleton. IGF-1 exerts direct actions on both cartilage and bone to stimulate growth and differentiation. These effects are crucial for growth from childhood to the end of adolescence.
Prolactin
- Precursor cells: mainly from lactotrophs in the AP
- Target cells: main target cells are mammary glands and gonads
- Mechanism of action: binds to peptide hormone receptor (single transmembrane domain) to activate the JAK2-STAT intracellular signaling pathway similar to that of GH
- Regulation: Like GH, dual hypothalamic inhibitory (from dopamine) and stimulatory hormones (PRH) regulate prolactin secretion. The predominant hypothalamic influence is inhibitory.
- Physiological Functions: The main functions of prolactin are stimulating mammary gland growth and development (mammographic effect) and milk production (lactogenic effect). It also has effects on the hypothalamic-pituitary-gonadal axis and can inhibit pulsatile GnRH secretion from the hypothalamus.
Follicle-stimulating hormone (FSH) and luteinizing hormone (LH)
- Precursor cells: gonadotrophs in the AP
- Target cells: gonads (ovaries and testes)
- Mechanism of action: FSH and LH bind to G protein-coupled receptors to activate the adenylyl cyclase enzyme, which in turn increases intracellular cAMP. cAMP activates protein kinase A (PKA) that phosphorylates intracellular proteins. These phosphorylated proteins then accomplish the final physiologic actions.
- Regulation: FSH and LH secretion are under the control of the hypothalamic gonadotropin-releasing hormone (GnRH).
- Physiological Functions: FSH and LH regulate the functions of the ovaries and the testes. In females, FSH stimulates the growth and development of follicles in preparation for ovulation and secretion of estrogens by the mature Graafian follicle. LH triggers ovulation and stimulates the secretion of progesterone by the corpus luteum. In males, FSH is required for spermatogenesis, and LH stimulates testosterone secretion by Leydig cells.
Thyroid-stimulating hormone (TSH)
- Precursor cells: thyrotropes in the AP
- Target cells: thyroid follicular cells
- Mechanism of action: TSH binds to the G-protein-coupled receptors on the basolateral membrane of the thyroid follicular cells. Similar to FSH and LH, it activates the adenylyl cyclase-PKA-cAMP system to phosphorylate several proteins, which in turn achieve the final physiologic actions
- Regulation: TSH secretion is under the control of the hypothalamic thyrotropin-releasing hormone (TRH). Also, T4 feeds back to the anterior pituitary to inhibit TSH secretion.
- Physiological functions: the main function of TSH is to stimulate the synthesis and secretion of thyroid hormones (tri-iodothyronine [T3] and thyroxine [T4]) from thyroid follicles. It also maintains the structural integrity of the thyroid glands.
Adrenocorticotrophic hormone (ACTH)
- Precursor cells: corticotrophs in the AP
- Target cells: cells in the cortex of the adrenal glands (adrenocortical cells)
- Mechanism of Action: ACTH binds to its G-protein coupled receptors on the adrenocortical cells. Similar to TSH, FSH, and LH, it activates the adenylyl cyclase-PKA-cAMP system to phosphorylate several proteins, which in turn achieve the final physiologic functions.
- Regulation: ACTH secretion is under the control of the hypothalamic corticotropin-releasing hormone (CRH). It is subject to negative feedback regulation.
- Physiological functions: the main function of ACTH is to stimulate the secretion of adrenal cortex hormones (mainly glucocorticoids) during stress. [rx]
The Posterior Pituitary (Neurohypophysis)
- The posterior pituitary is neural in origin. Unlike the anterior pituitary, the posterior pituitary is connected directly to the hypothalamus via a nerve tract (hypothalamohypophyseal nerve tract). It secretes two hormones: oxytocin and antidiuretic hormone (ADH) or vasopressin. The hormones are synthesized by the magnocellular neurons located in the supraoptic and paraventricular nuclei of the hypothalamus. The hormones are transported in association with neurophysins proteins along the axons of these neurons to end in nerve terminals within the posterior pituitary.[3]
Oxytocin
- Precursor cells: paraventricular and supraoptic nuclei in the hypothalamus
- Target cells: myoepithelial cells of the mammary glands and the uterine muscles (myometrium) in women and myofibroblast cells in the seminiferous tubules in men.
- Mechanism of action: oxytocin acts on its target cells via a G-protein coupled receptor, which activates phospholipase C that in turn stimulates phosphoinositide turnover. This causes increased intracellular calcium concentration, which activates the contractile machinery of the cell.
- Regulation: oxytocin is released in response to an afferent neural input to the hypothalamic neurons that synthesize the hormone. Suckling and uterine stimulation by the baby’s head during delivery are the major stimuli for oxytocin release. It is subject to positive feedback regulation.
- Physiological Functions: oxytocin stimulates milk ejection from the breast in response to suckling (milk ejection reflex). It causes contraction of myoepithelial cells surrounding the ducts and alveoli of the gland and therefore milk ejection. Oxytocin also stimulates uterine contraction during labor to expel the fetus and placenta.
Antidiuretic Hormone (ADH) or Vasopressin
- Precursor cells: paraventricular and supraoptic nuclei of the hypothalamus.
- Target cells: renal distal convoluted tubules and collecting duct and vascular smooth muscle cells.
- Mechanism of action: similar to oxytocin, it acts on its target cells via a G-protein coupled receptor, which activates phospholipase C that in turn stimulates phosphoinositide turnover and causes an increase in intracellular calcium concentration which in turn achieves the final physiologic actions.
- Regulation: The main stimulus for ADH release is an increase in osmolality of circulating blood. Osmoreceptors located in the hypothalamus detect this increase and activate the paraventricular and supraoptic nuclei to release ADH. It also releases in response to hypovolemia.4Physiological Functions: ADH binds to V2 receptors on the distal tubule and collecting ducts of the kidney to up-regulate aquaporin channel expression on the basolateral membrane and increase water reabsorption. It, as its name suggests, also acts as a vasoconstrictor upon binding to V1 receptors on the arteriolar smooth muscle.
Overview of the Pituitary Gland
The pituitary gland is connected to the hypothalamus and secretes nine hormones that regulate body homeostasis.
Key Points
The pituitary gland, or hypophysis, is an endocrine gland about the size of a pea. Although located at the base of the brain and often considered to be part of the brain, the pituitary gland is in fact a separate organ and is not part of the brain.
The pituitary gland is divided into two parts, the anterior pituitary, and the posterior pituitary. The anterior pituitary receives signaling molecules from the hypothalamus, and in response, synthesizes and secretes seven hormones.
The posterior pituitary does not produce any hormones of its own; instead, it stores and secretes two hormones made in the hypothalamus.
Key Terms
pituitary gland: An endocrine gland, about the size of a pea, that sits in a small, bony cavity at the base of the brain whose secretions control the other endocrine glands and influence growth, metabolism, and maturation.
hypothalamus: A region of the forebrain located below the thalamus, forming the basal portion of the diencephalon, and functioning to regulate body temperature, some metabolic processes, and governing the autonomic nervous system.
The pituitary gland, or hypophysis, is an endocrine gland about the size of a pea. Although located at the base of the brain and often considered to be part of the brain, the pituitary gland is in fact a separate organ. It protrudes off the bottom of the hypothalamus at the base of the brain, and rests in a small, bony cavity.

Pituitary location: The location of the pituitary gland in the human brain.
The pituitary is functionally connected to the hypothalamus by a small tube called the infundibular stem, or, pituitary stalk. The pituitary gland secretes hormones that regulate homeostasis.
The pituitary gland is divided into two parts, the anterior pituitary, and the posterior pituitary.
- The anterior pituitary receives signaling molecules from the hypothalamus, and in response, synthesizes and secretes seven important hormones including thyroid-stimulating hormone and growth hormone.
- The posterior pituitary does not produce any hormones of its own, rather, it stores and secretes two hormones made in the hypothalamus— oxytocin and
anti-diuretic hormone.

The pituitary gland: In this image, the pituitary gland is referred to by its other name, the hypophysis.
Control of the Pituitary Gland by the Hypothalamus
The pituitary gland consists of the anterior pituitary and the posterior pituitary.
Key Points
While the pituitary gland is known as the master endocrine gland, both of its lobes are under the control of the hypothalamus: the anterior pituitary receives its signals from the parvocellular neurons, and the posterior pituitary receives its signals from the magnocellular neurons.
The pituitary gland is connected by a system of blood vessels to the hypothalamus. This system of blood vessels is known as the hypophyseal portal system, and it allows endocrine communication between the two structures.
The mechanism for hormone transport via hypothalamoportal vessels involves cells that are regulated by different nuclei in the hypothalamus; for instance, neurons that release neurotransmitters as hormones in the connective link between the pituitary and the brain.
Key Terms
pituitary gland: An endocrine gland, about the size of a pea, that sits in a small, bony cavity at the base of the brain whose secretions control the other endocrine glands and influence growth, metabolism, and maturation.
hypothalamus: A region of the forebrain located below the thalamus, forming the basal portion of the diencephalon, that regulates body temperature, some metabolic processes, and governs the autonomic nervous system.
hypophyseal portal system: The system of blood vessels that link the hypothalamus and the anterior pituitary in the brain.
The pituitary gland consists of two components: the anterior pituitary and the posterior pituitary, and is functionally linked to the hypothalamus by the pituitary stalk (also named the infundibular stem, or simply the infundibulum).
Whilst the pituitary gland is known as the master endocrine gland, both of the lobes are under the control of the hypothalamus: the anterior pituitary receives its signals from the parvocellular neurons, and the posterior pituitary receives its signals from magnocellular neurons.
The anterior lobe of the pituitary receives hypothalamic-releasing hormones from the hypothalamus that bind with receptors on endocrine cells in the anterior pituitary that regulate the release of adrenal hormones into the circulatory system. Hormones from the hypothalamus are rapidly degraded in the anterior pituitary, which prevents them from entering the circulatory system.
The posterior lobe of the pituitary gland develops as an extension of the hypothalamus. As such, it is not capable of producing its own hormones; instead, it stores hypothalamic hormones for later release into the systemic circulation.

Pituitary gland: The anterior and posterior lobes of the pituitary (hypophysis) gland are shown.
The Anterior Pituitary
The anterior pituitary secretes seven hormones that regulate several physiological processes, including stress, growth, and reproduction.
Key Points
A major organ of the endocrine system, the anterior pituitary, also called the adenohypophysis, is the glandular, anterior lobe of the pituitary gland.
The anterior pituitary regulates several physiological processes, including stress, growth, reproduction, and lactation.
The anterior pituitary gland secretes 7 hormones: follicle-stimulating hormone, luteinizing hormone, adrenocorticotropic hormone, thyroid-stimulating hormone, prolactin, endorphins, and growth hormone.
Key Terms
anterior pituitary gland: A major organ of the endocrine system that regulates several physiological processes including stress, growth, reproduction, and lactation.
A major organ of the endocrine system, the anterior pituitary (also called the adenohypophysis) is the glandular, anterior lobe of the pituitary gland. The anterior pituitary regulates several physiological processes including stress, growth, reproduction, and lactation.
Its regulatory functions are achieved through the secretion of various peptide hormones that act on target organs including the adrenal gland, liver, bone, thyroid gland, and gonads. The anterior pituitary itself is regulated by the hypothalamus and by negative feedback from these target organs.
Anatomy of the Anterior Pituitary Gland
The fleshy, glandular anterior pituitary is distinct from the neural composition of the posterior pituitary. The anterior pituitary is composed of multiple parts:
- Pars distalis: This is the distal part that comprises the majority of the anterior pituitary; it is where most pituitary hormone production occurs.
- Pars tuberalis: This is the tubular part that forms a sheath that extends up from the pars distalis and wraps around the pituitary stalk. Its function is poorly understood.
- Pars intermedia: This is the intermediate part that sits between the pars distalis and the posterior pituitary and is often very small in humans.
Major Hormones Secreted by the Anterior Pituitary Gland
- Adrenocorticotropic hormone (ACTH), is a polypeptide whose target is the adrenal gland. The effects of ACTH are upon the secretion of glucocorticoid, mineralocorticoids, and sex corticoids.
- Beta-endorphin is a polypeptide that affects the opioid receptor, whose effects include the inhibition of the perception of pain.
- Thyroid-stimulating hormone is a glycoprotein hormone that affects the thyroid gland and the secretion of thyroid hormones.
- Follicle-stimulating hormone is a glycoprotein hormone that targets the gonads and affects the growth of the reproductive system.
- Luteinizing hormone is a glycoprotein hormone that targets the gonads to effect sex hormone production.
- Growth hormone is a polypeptide hormone that targets the liver and adipose tissue and promotes growth through lipid and carbohydrate metabolism.
- Prolactin is a polypeptide hormone whose target is the ovaries and mammary glands. Prolactin influences the secretion of estrogen/progesterone and milk production.
Regulation
Hormone secretion from the anterior pituitary gland is regulated by hormones secreted by the hypothalamus. Neuroendocrine neurons in the hypothalamus project axons to the median eminence, at the base of the brain. At this site, these neurons can release substances into the small blood vessels that travel directly to the anterior pituitary gland (the hypothalamohypophysial portal vessels).
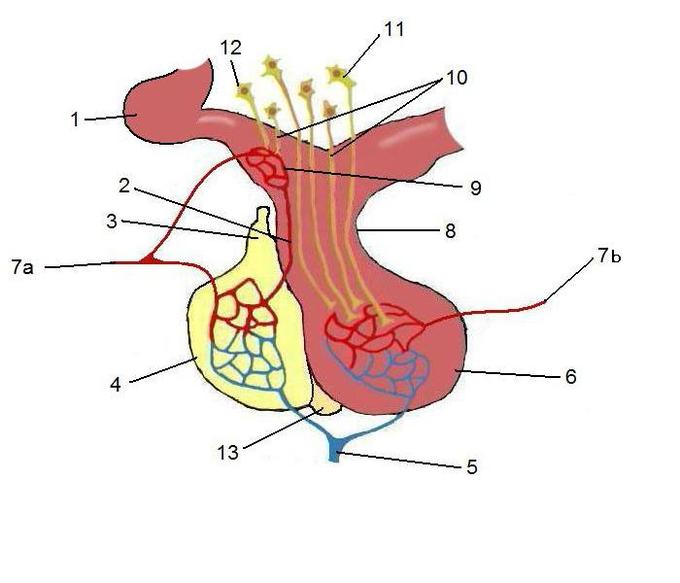
The anterior pituitary: The anterior pituitary, in yellow, is linked to the hypothalamus by a portal system. The hypothalamus releases signaling molecules that incite the anterior pituitary to produce hormones.
The Posterior Pituitary
The posterior pituitary secretes two important endocrine hormones—oxytocin and antidiuretic hormone.
Key Points
The posterior pituitary (or neurohypophysis) comprises the posterior lobe of the pituitary gland and is part of the endocrine system.
Hormones known as posterior pituitary hormones are synthesized by the hypothalamus, and include oxytocin and antidiuretic hormone.
The hormones are then stored in neurosecretory vesicles (Herring bodies) before being secreted by the posterior pituitary into the bloodstream.
Key Terms
oxytocin: A hormone that stimulates contractions during labor.
posterior pituitary: The posterior pituitary (or neurohypophysis) comprises the posterior lobe of the pituitary gland and is part of the endocrine system. Despite its name, the posterior pituitary gland is not a true gland; rather, it is largely a collection of axonal projections from the hypothalamus that terminate behind the anterior pituitary gland.
Antidiuretic hormone: A hormone that stimulates water reabsorption in the kidneys.
Posterior Pituitary Gland

Pituitary: Pituitary gland representation.
The posterior pituitary (or neurohypophysis) comprises the posterior lobe of the pituitary gland and is part of the endocrine system. Despite its name, the posterior pituitary gland is not a gland; rather, it is largely a collection of axonal projections from the hypothalamus that terminate behind the anterior pituitary gland.
The posterior pituitary consists mainly of neuronal projections ( axons ) extending from the supraoptic and paraventricular nuclei of the hypothalamus. These axons release peptide hormones into the capillaries of the hypophyseal circulation. These are then stored in neurosecretory vesicles (Herring bodies) before being secreted by the posterior pituitary into the systemic bloodstream.
Anatomy of the Posterior Pituitary Gland
The posterior pituitary is derived from the hypothalamus and is distinct from the more fleshy, vascularized anterior lobe. The posterior pituitary is composed of two parts:
- The pars nervosa also called the neural lobe or posterior lobe constitutes the majority of the posterior pituitary and is the storage site of oxytocin and vasopressin.
- The infundibular stalk, also known as the infundibulum or pituitary stalk, bridges the hypothalamic and hypophyseal systems.
Major Hormones Secreted by the Posterior Pituitary Gland
The posterior pituitary stores two hormones secreted by the hypothalamus for later release:
- Oxytocin, most of which is released from the paraventricular nucleus in the hypothalamus. Oxytocin is one of the few hormones that create a positive feedback loop.
- Antidiuretic hormone (ADH, also known as vasopressin), the majority of which is released from the supraoptic nucleus in the hypothalamus. ADH acts on the collecting ducts of the kidney to facilitate the reabsorption of water into the blood.
Clinical Significance
The following are some of the critical disease conditions associated with the pituitary gland.
- Pituitary Adenoma – The most common pathology in the sellar region is the pituitary tumor. They classify into microadenomas (less than 10 mm) and macroadenomas (more than 10 mm). These macroadenomas can compress the adjacent structures. When it extends laterally, the cavernous sinus is compressed, producing ophthalmoplegia. The patients will present with diplopia due to cranial nerve compression. They may also present asymptomatically or with headaches. All the cell lines are capable of producing an adenoma.
- Prolactinoma – This is the most common type of functioning secretory adenoma. They remain asymptomatic for an extended period until they cause compression or mass effect on the normal surrounding tissue causing hormonal dysfunction, visual changes, hydrocephalus, and hypogonadism.
- Cushing Disease – This results from an ACTH secreting pituitary adenoma. They present with symptoms such as proximal myopathy, psychiatric disturbances, obesity, purple striae over the abdomen, extra fat around the neck termed buffalo hump, and hypertension. The standard method for resection of the tumor is transsphenoidal adenectomy. The route is via the posterior wall of the sphenoid sinus, which forms the inferior border of the pituitary gland.
- GH Secreting Adenoma – This adenoma produces a lot of GH, which can cause acromegaly or gigantism. The patient may present with carpal tunnel syndrome, proximal myopathy, and rarely hypertension or diabetes mellitus.
- Stalk Compression Syndrome – The patient presents with symptoms of hyperprolactinemia with raised prolactin concentration in the presence of a sellar or suprasellar mass compressing the stalk.
- Pituitary Apoplexy – Pituitary adenomas that are often asymptomatic may enlarge in size and acquire additional arterial blood supply directly and undergo hemorrhagic infarction. The clinical presentation includes abrupt onset headache, visual symptoms like diplopia due to cavernous sinus compression, panhypopituitarism with low blood pressure, focal neurological deficits. The apoplexy triad includes headaches, visual changes, and vomiting. Clinicians can misdiagnose this condition as a subarachnoid hemorrhage. An emergency CT will show an enlarged pituitary fossa with some blood, and an MRI will confirm the diagnosis.
- Sheehan Syndrome – This is due to the infarction and necrosis of the pituitary gland. It can be described as postpartum hypopituitarism, as postpartum hemorrhage is closely associated with its etiology. The gland enlarges during pregnancy, which causes the superior hypophyseal artery to get compressed. If the patient experiences a drop in her blood pressure during childbirth, this causes infarction and necrosis of the gland. The patient will commonly present with failure to lactate during the postpartum period, ultimately leading to a deficiency of the anterior pituitary hormones.
- Lymphocytic Hypophysitis – This condition is commonly associated with pregnancy. It is an autoimmune condition with diffuse lymphocytic infiltration that destroys normal tissue with scaring. Imaging with an MRI shows homogenously enhancing and enlarged glands.
- Granulomatous Hypophysitis – This is a non-caseating granuloma with Langerhans type giant cell. When it is present in the posterior lobe, it may be due to neurosarcoidosis.
- Empty Sella Syndrome – There are two types of empty sella syndrome that are differentiated according to the cause. The primary empty sella syndrome is a defect in the diaphragm sellae that allows the contents above to herniate into the sella, thus compressing the gland. The secondary empty sella syndrome is due to causes such as tumors or surgery. This syndrome is associated with multiparous women, obesity, and benign intracranial hypertension. In multiparous women, this may be due to the repeated enlargement and involution of the gland leading to the gland becoming flattened. This condition must be differentiated from craniopharyngioma and Rathke’s cleft cyst as they may also present with a cyst within the same location.
- Syndrome of Inappropriate Antidiuretic Hormone(SIADH) This is a condition with excessive production of antidiuretic hormone, which can result from various conditions such as nervous system disorders, neoplastic, ectopic sources such as paraneoplastic syndromes, head trauma, and drugs. The patients will present with altered mental status, seizures, or even more severe cases with coma. There will be hyponatremia due to dilution with free water. The urine analysis will show increased concentration and osmolality.
- Craniopharyngiomas – Two variants are classified based on clinical and genetic features, which are the adamantinomatous (aCP) and papillary (pCP) craniopharyngiomas. The aCP occurs in children, and pCP is exclusive to adults. The embryonic theory proposed states that this develops from the ectopic embryonic remnants of Rathke’s pouch. The metaplastic theory states that the squamous epithelium that is part of the gland undergoes metaplasia and transforms.
- Rathke’s Cleft Cyst – This is a benign cyst that originates from the mucinous substances in the remnants of Rathke’s pouch. The cyst contains the pink eosinophilic substance. Due to chronic inflammation, they may develop xanthogranulomas or cholesterol crystals.
- Multiple Endocrine Neoplasia-1(MEN-1) – This is a genetic, endocrine neoplastic syndrome. There is an abnormal growth in the pituitary gland, parathyroid gland, and the pancreas.[rx][rx][rx]
References
About the author