Ankle strain refers to a painful condition of the ankle joint brought about by inflammation, overuse or simply awkward (or unbalanced) use. It includes inflammation of muscles and tendons such as the Achilles tendon at the back of the heel.
Ankle sprain also known as a twisted ankle or rolled ankle, is a common injury where sprain occurs on one or more ligaments of the ankle. A sprained ankle is an injury that occurs when you roll, twist or turn your ankle in an awkward way. This can stretch or tear the tough bands of tissue (ligaments) that help hold your ankle bones together. Ligaments help stabilize joints, preventing excessive movement. A sprained ankle occurs when the ligaments are forced beyond their normal range of motion. Most sprained ankles involve injuries to the ligaments on the outer side of the ankle.
A sprain is an injury to the band which connects two or more bones to a joint. This band is called a ligament. A sprain is usually caused by the joint being forced suddenly outside its usual range of movement. Most sprains heal within a few weeks. A severe sprain may look and feel like a fracture, and it can be difficult for health professionals to tell the difference between the two.
A fracture is a break in one of the bones which make up the ankle joint. These are the leg bones (the tibia and fibula) and the heel and forefoot bones (the calcaneus and talus). Depending upon the exact cause of the fracture, one or more bones may be involved.
Ankle pain may also arise from existing conditions of the joint itself, such as arthritis or gout, which may be aggravated by movement, impact or strain
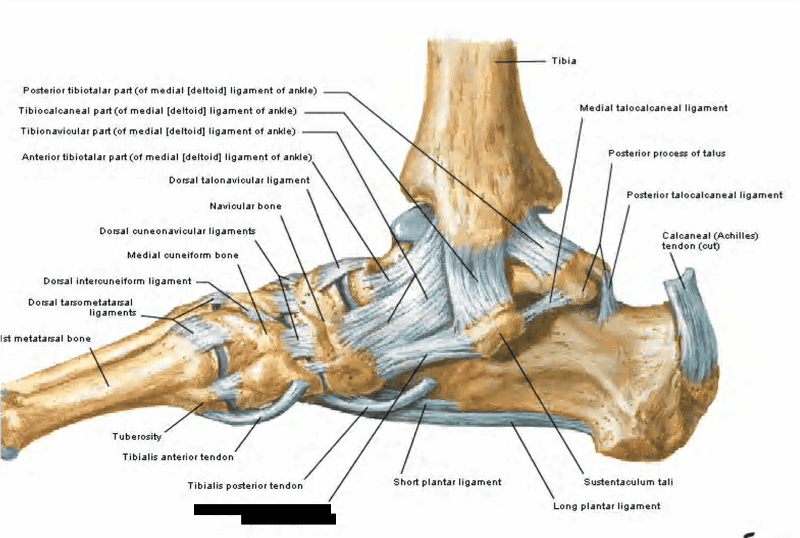
Anatomy of Ankle Sprain / Strain
Ligaments > distal tibiofibular syndesmosis includes
Anterior-inferior tibiofibular ligaments (AITFL)
- originates from anterolateral tubercle of the tibia (Chaput’s)
- inserts on anterior tubercle of the fibula (Wagstaffe’s)
Posterior-inferior tibiofibular ligament (PITFL)
- originates from posterior tubercle of the tibia (Volkmann’s)
- inserts on the posterior part of the lateral malleolus
- the strongest component of the syndesmosis
- interosseous membrane
Interosseous ligament (IOL)
- distal continuation of the interosseous membrane
- the main restraint to proximal migration of the talus
- inferior transverse ligament (ITL)
Syndesmosis Biomechanics
- function > maintains integrity between the tibia and fibula & resists axial, rotational, and translational forces
- normal gait >syndesmosis widens 1mm during gait
- deltoid ligament >indirectly stabilizes the medial ankle mortise
Types of Ankle Sprain / Strain with Fracture
Classifications are based on particular patterns of breakage which are seen after particular types of injury. These include
- Pott’s fracture: involving both the tibia and fibula leg bones (bimalleolar fractures). These fractures are unstable and require urgent treatment.
- Pilon fracture: a fracture of the very end of the tibia and top of the talus forefoot bone. The talus is ‘driven’ into the tibia as may happen in a fall from a height or a foot braced against the floor of a car in a collision.
- Snowboarder’s fracture: this is a fracture of the outer side of the talus produced by forced turning down and inwards of the foot at the ankle.
- Stress fracture: this is a small crack in a bone. Stress fractures often develop from overuse, such as from high-impact sports like distance running – the repeated stress of the foot striking the ground can cause problems. Stress fractures differ from other ankle fractures in that they result from overuse rather than sudden trauma. The cracks are small (although they may be multiple) so that, although they are painful, the swelling may be only slight. In the ankle, the heel (calcaneus) and the lower leg (fibula) are most commonly affected.
-

www.rxharun.com
Grade of Ankle Sprain
Depending on the severity of the injury, an ankle sprain is classified as:
- Grade I — The ankle is painful, but there is little ligament damage and little loss of function.
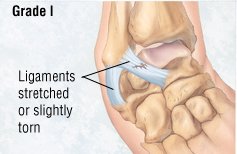
- Grade II — There is moderate ligament damage, and the ankle joint is somewhat loose.
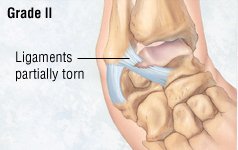
- Grade III — One or more ligaments are torn, and the ankle joint is very loose or unstable.
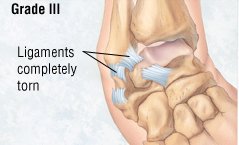
Classification of Ankle Sprains
| GRADE | SIGNS AND SYMPTOMS |
|---|---|
|
I: partial tear of a ligament |
Mild tenderness and swelling |
|
Slight or no functional loss (i.e., patient is able to bear weight and ambulate with minimal pain) |
|
|
No mechanical instability (negative clinical stress examination) |
|
|
II: incomplete tear of a ligament, with moderate functional impairment |
Moderate pain and swelling |
|
Mild to moderate ecchymosis |
|
|
Tenderness over involved structures |
|
|
Some loss of motion and function (i.e., patient has pain with weight-bearing and ambulation) |
|
|
Mild to moderate instability (mild unilateral positivity of clinical stress examination) |
|
|
III: complete tear and loss of integrity of a ligament |
Severe swelling (more than 4 cm about the fibula) |
|
Severe ecchymosis |
|
|
Loss of function and motion (i.e., patient is unable to bear weight or ambulate) |
|
|
Mechanical instability (moderate to severe positivity of clinical stress examination) |
| A grade of scientific evidence | |
|---|---|
| Class I |
|
| Class II |
and case control studies) |
| Class III |
|
Level of recommendation
| 1 |
|
| Level 2 |
|
| Level 3 |
|
Causes of Ankle Sprain
These are the main causes that can lead to the appearance of high ankle sprain:
- Walking or exercising on an uneven surface
- Falling down
- Participating in sports that require cutting actions or rolling and twisting of the foot—such as trail running, basketball, tennis, football, and soccer
- During sports activities, someone else may step on your foot while you are running, causing your foot to twist or roll to the side.
Rotational injuries
- Ankle fractures
Impact sports
- Football tackles
- Falling or being pushed forward
- Side-to-side running
- Starting and stopping feet in a repetitive manner
- Turning while moving
- Other sports: hockey, wrestling, soccer
Mechanism
- Foot is planted on the ground
- Foot is then twisted outward (excessively)
- Bones pull away from each other and the syndesmotic ligaments that connect them are torn
Increased risk
- Severe load on the ankle
- Excessive dorsiflexion of the foot – toes go beyond their normal range of motion, towards the shin
- When a person is tangled under another person.
Symptoms of an ankle sprain
In an ankle sprain, the following signs and symptoms may occur
- Localized pain at the site of the sprain – For example, if the deltoid ligament has been sprained, pain would be localized to the inside of the ankle. Pain is often described as sudden and sharp, and worsens with movement or placing weight on the ankle. Pain may be relieved somewhat by rest and elevation of the ankle.
- Swelling at the site of the sprain – In the case of a deltoid ligament sprain, the inside of the ankle may be noticeably swollen. Or swelling may occur on the outside of the ankle if one or more ligaments in the lateral ligament complex are sprained.
- Bruising over the site of the sprain – In addition to swelling, patients may notice bluish, reddish, or purplish skin discolorations over the sprain site as an indication that ligaments have torn and blood is rushing to the area.
- Limited ability to move the ankle – In more severe sprains, patients may not be able to turn, bend, or flex the foot. Weight-bearing activities such as walking may become difficult or impossible.
- Popping sound or sensation – When the injury occurs, patients may hear or feel a “pop” as the ligament is stretched or torn.
- Intense pain at the time of the trauma – In cases of severe sprains when the ligament(s) is partially or completely torn, the pain is sudden and severe enough to make patients stop whatever they are doing and become immobile.
- Sensibility affected – This is due to the inflammation which increases the pressure in the area.
- Stiffness – Mainly after some time without moving your ankle.
- Limited range of motion – All movements are going to be limited, although the most restricted (as it will cause pain) is ankle inversion.
- Instability – When the ankle sprain is a severe one.
- Difficulty or impossibility of bearing your weight – The more severe the ankle sprain, the more difficult to bear your weight and walk.
- Pop sound in some severe ankle sprains
Ankle Sprain assessment

The therapist will perform a series of tests which may include the following
Observation
- Observation is usually the first stage of any injury assessment.
- The therapist will usually observe the patient in both standing and lying down and will be looking closely for swelling, bruising and deformity, as well as postural issues such as over pronation of the feet or problems putting the foot on the floor.
Palpation
- The therapist will then palpate the entire ankle joint and surrounding area to assess if the joint is warm (due to acute inflammation) and swollen and if the ligaments are painful to touch.
Range of Motion
- The therapist will usually assess both active (the patient moves) and passive (the therapist moves the joint) movements of the ankle with the knee both straight and then bent.
- The ankle is often painful to move after an ankle sprain.
- Passive range of motion is usually pain-free as the muscles are not contracting, although the end of range into dorsiflexion (toes pointing upwards) may be painful as the muscles stretch.
Assessing Ankle flexibility
- Depending on the severity of the ankle injury, the therapist may assess the patient in standing to test the movement of the ankle when weight bearing.
Resisted Muscle Tests
- These tests are used to assess strength of the muscles around the ankle joint compared to the other side.
- They may be tested with the knee straight and then bent.
Special Tests
Special tests are used to assess the integrity of the ligaments and how badly damaged they are.
- “Anterior drawer test” will be used to assess the ATFL ligament
- “Talar Tilt” test will be used to test the CFL ligament
- External rotation and squeeze tests will be used to assess the high ankle ligaments (syndesmosis complex)
Imaging of Ankle Sprain
Radiographs > indications for radiographs with an ankle injury include (Ottawa ankle rules)
- inability to bear weight
- medial or lateral malleolus point tenderness
- 5MT base tenderness
- navicular tenderness
Radiographic views to obtain > standard ankle series (weight bearing)
- AP
- lateral
- mortise
ER rotation stress view
- useful to diagnosis syndesmosis injury in high ankle sprain
- look for asymmetric mortise widening
- medial clear space widening > 4mm
- tibiofibular clear space widening of 6 mm
Varus stress view
- used to diagnose injury to ATFL or CFL
- measures ankle instability by looking at talar tilt and anterior talar translation
Radiographs more
- X-rays – X-rays provide images of dense structures, such as bone. Your doctor may order x-rays to rule out a broken bone in your ankle or foot. A broken bone can cause similar symptoms of pain and swelling.
- Stress x-rays – In addition to plain x-rays, your doctor may also order stress x-rays. These scans are taken while the ankle is being pushed in different directions. Stress x-rays help to show whether the ankle is moving abnormally because of injured ligaments.
- Magnetic resonance imaging (MRI) scan – Your doctor may order an MRI if he or she suspects a very severe injury to the ligaments, damage to the cartilage or bone of the joint surface, a small bone chip, or another problem. The MRI may not be ordered until after the period of swelling and bruising resolves.
- Ultrasound – This imaging scan allows your doctor to observe the ligament directly while he or she moves your ankle. This helps your doctor to determine how much stability the ligament
Sonography
Sonography is a valuable tool for examining the tendons of the ankle joint such as the Achilles or the peroneal tendons for rupture or displacement.[rx] Only a few studies have evaluated the capacity of sonography to diagnose injuries of the lateral ligaments of the ankle. Milz et al. performed the sonographic evaluation in 20 patients using MRI as the gold standard with a sensitivity of 92% and a specificity of 83% for injury and rupture of ATFL.[rx] In 34 patients, sonography was confirmed at arthroscopy with a sensitivity of 100% and a specificity of 33%.[rx] However, sonographic evaluation is strongly dependent on the expertise of the technician.[rx] Furthermore, state of the art equipment and examination techniques are the prerequisite to assess ligament integrity.[rx]
Arthrography
Rupture of the ATFL can be diagnosed with a sensitivity of 96–100% using arthrography.[rx] For the PTFL, sensitivity decreases to 75% for anatomical reasons.[rx] Further arthrography is invasive and is not able to provide images of the ligament itself, but it is an indirect tool for the diagnosis of rupture. Therefore, it should not be considered a standard tool for diagnosis of ligament rupture in the ankle.
Recommendation: arthrography shows a similar sensitivity only in diagnosing injuries of the ATLF compared to delayed physical examination. It is, however, an invasive procedure and should not, therefore, be recommended for routine practice.
Treatment of Ankle Sprain
PRICE therapy
PRICE stands for
Protection – protect the affected area from further injury by using a support or, in the case of an ankle injury, wearing shoes that enclose and support your feet, such as lace-ups.
Rest – stop the activity that caused the injury and rest the affected joint or muscle. Avoid activity for the first 48 to 72 hours after injuring yourself. Your GP may recommend you use crutches.
Ice – Ice helps decrease swelling, bruising, pain, and muscle spasms. Putting ice on your ankle is helpful, but you need to be careful. The cold can damage your nerves if you leave ice in place too long. You should only use ice for up to 20 minutes at a time. If your skin feels numb, it’s time to remove the ice. Use ice treatments every 2 to 4 hours for the first 3 days after your injury. Ice treatments can consist of ice packs, ice baths, or ice massages.
- To make an ice pack, partly fill a plastic bag with ice. Put a thin, damp cloth on your ankle to create a layer between your skin and the ice. Wrap an elastic bandage around the ice pack to hold it in place.
- For an ice bath, fill a large bucket with water and ice. Place your ankle in the bucket until the skin starts to get numb.
- Ice massages can work well for small areas. Freeze water in 4- to 8-ounce Styrofoam (coffee) cups. Tear the top part of the cup away from the ice. Hold the covered end and slowly rub the ice over the sprained area in a circular motion. Don’t hold the ice on one spot for more than 30 seconds.
Compression – compress or bandage the injured area to limit any swelling and movement that could damage it further. You can use a simple elastic bandage or an elasticated tubular bandage available from a pharmacy. It should be wrapped snuggly around the affected area, but not so tightly that it restricts blood flow. Remove the bandage before you go to sleep.
Elevation – keep the injured area raised and supported on a pillow to help reduce swelling. If your leg is injured, avoid long periods of time where your leg isn’t raised.
Support devices – such as a brace, cast, or splint, may be needed to limit your movement and protect your joint. You may need to use crutches to decrease your pain as you move around.
Acute care/immobilization – Immediately after a LAS the primary goals are to manage pain, control inflammation and protect the joint so that the healing process can begin. In the acute phase of healing, the most important structures to protect are the lateral ligaments of the ankle because the traumatic mechanism has caused increased laxity. In the past, the majority of the literature has focused on functional rehabilitation after a LAS. But with the high recurrence rates of LAS, development of CAI and potential for the development of ankle OA, functional rehabilitation may not allow adequate time for the ligaments of the ankle to heal and stability to be restored. Indeed, increased laxity has been reported using both subjective (ankle giving way, or feelings of instability) and objective (manual stress tests, radiographs) outcome measures.[Rx]
Cryotherapy – Cryotherapy has been proved to be effective in the treatment of soft tissue injuries.[Rx] The quality of studies of sprained ankles is poor, as cryotherapy has usually been combined with other treatments. However, it seems to reduce swelling and the need for painkillers, particularly when used soon after the injury, and it should, therefore, be part of the initial standard regimes.[rx] Furthermore, it improves the reliability of the clinical examination.[rx] The duration, frequencies and the technique of ice application remain controversial.[rx]
Medicines
- NSAIDs – such as ibuprofen, help decrease swelling, pain, and fever. This medicine is available with or without a doctor’s order. NSAIDs can cause stomach bleeding or kidney problems in certain people. If you take blood thinner medicine, always ask your healthcare provider if NSAIDs are safe for you. Always read the medicine label and follow directions.
- Acetaminophen – decreases pain. It is available without a doctor’s order. Ask how much to take and how often to take it. Follow directions. Acetaminophen can cause liver damage if not taken correctly.
- Prescription pain medicine – may be given. Ask how to take this medicine safely.
Avoiding HARM
For the first 72 hours after a sprain or muscle strain, you should avoid HARM. This means you should avoid:
- Heat – such as hot baths, saunas or heat packs.
- Alcohol – drinking alcohol will increase bleeding and swelling, and slow healing.
- Running – or any other form of exercise that could cause more damage.
- Massage – which may increase bleeding and swelling.
Other treatments
- Laser therapy,[rx] ultrasound,[rx] electrotherapy,[rx] homeopathic therapy, hyperbaric oxygen therapy,[rx] prolotherapy, platelet-rich plasma, hyaluronic acid[rx] or topical nitroglycerin injection[rx] were not effective, or available data were insufficient to prove their benefit in the treatment of acute ankle injuries. In order to prove their benefit, new treatment options must be superior to placebo and to the current gold standard, i.e. functional treatment. Consequently, they should not be part of a standard protocol for the treatment of acute ankle sprains.[rx]
- Recommendation: so far, none of these treatments have been shown to enhance recovery from acute ankle injuries. Therefore, they should not be considered as part of the standard regime in treating acute ankle injuries.
Balance exercises
- One of the most commonly examined sensorimotor outcome measures following a LAS is single leg postural control. A prospective investigation has shown that single leg postural control is impaired for at least four weeks after injury.[rx] Further, recent systematic reviews have demonstrated that postural control is impaired on both the involved limb[rx] and the uninvolved limb[rx] relative to an uninjured control group within six weeks of a LAS. The presence of bilateral balance impairments (ie, impaired balance on the involved and uninvolved limb relative to a healthy reference group)[rx], as well as bilateral alterations at joints proximal to the ankle7,68, suggest changes in motor control patterns that are centrally mediated (ie, feed-forward neuromuscular control) have occurred.
Joint mobilizations
- To date, manipulative therapy techniques; including Maitland’s mobilizations,[rx] Mulligan’s mobilizations with movement,[rx] and high-velocity low-amplitude (HVLA) thrusts,[rx]have all been postulated to be effective treatments for acute LAS. Indeed, manipulative therapy techniques are theorized to reduce pain, improve function and increase ROM via the restoration of arthrokinematic motions (ie, roll, glide, spin),[rx] thus recommendations to use these techniques make intuitive sense. Further, there is a great deal of anecdotal evidence in the form of published case studies supporting the use of manipulative therapies to improve various outcome measures in acute LAS.[rx]
Physiotherapy for Ankle Sprain
- Reduce Pain and Swelling – You will learn how to avoid or modify your daily and sports activities to allow healing to begin. Your physical therapist may use different types of treatments and technologies to control and reduce your pain and swelling, including ice, heat, ultrasound, electrical stimulation, taping, specific exercises, and hands-on therapy, such as specialized massage.
- Improve Motion – Your physical therapist will choose specific activities and treatments to help restore normal movement in the ankle. These might begin with “passive” motions that the physical therapist performs for you to gently move your ankle and foot, and progress to “active” exercises and stretches that you do yourself.
- Improve Flexibility – Your physical therapist will determine if any foot, ankle, or lower leg muscles are tight, begin to stretch them, and teach you how to stretch them.
- Improve Strength – Ankle sprains may be related to weak, injured, or uncoordinated leg muscles. Certain exercises will aid healing at each stage of recovery; your physical therapist will choose and teach you the correct exercises and equipment to use, to steadily and safely restore your strength. These may include using cuff weights, stretch bands, and weight-lifting equipment.
- Improve Endurance – Regaining your muscular endurance in the ankle and leg is important after an injury. Your physical therapist will teach you exercises to improve endurance, so you can return to your normal activities. Cardio-exercise equipment may be used, such as treadmills or stationary bicycles.
- Improve Balance – Regaining your sense of balance is important after an injury. Your physical therapist will teach you exercises to improve your balance ability.
- Restore Agility – Speed and accuracy of leg movement is important in athletics and in many daily activities. Your physical therapist will help you regain these skills in preparation for a return to sports and to your daily routine.
- Learn a Home Program – Your physical therapist will teach you strengthening and stretching exercises to perform at home. These exercises will be specific for your needs; if you do them as prescribed by your physical therapist, you can speed your recovery.
- Return to Activities – Your physical therapist will discuss activity goals with you and use them to set your work, sport, and home-life recovery goals. Your treatment program will help you reach your goals in the safest, fastest, and most effective way possible. Your physical therapist will teach you exercises, work retraining activities, and sport-specific techniques and drills to help you achieve your goals.
- Speed Recovery Time – Your physical therapist is trained and experienced in choosing the best treatments and exercises to help you safely heal, return to your normal lifestyle, and reach your goals faster than you are likely to do on your own.
Exercises for Ankle Sprain
Exercise to Improve Range of Motion Following Syndesmotic Sprain or Syndesmotic Ankle Sprain
- Sit straight and try and bring the ankle and foot up as much as possible so that a stretch to the calf is felt. Hold this position for about 10 seconds and repeat this around 10 times.

Exercise to Improve Range of Motion Following Syndesmotic Sprain or Syndesmotic Ankle Sprain
- In this exercise, while seated bring and the ankle down and bend it inwards. Maintain this position for about 10 seconds and repeat it about 10 times.

Exercise to Improve Range of Motion Following Syndesmotic Sprain or Syndesmotic Ankle Sprain
- In this exercise, from a seated position bring the ankle up in an outwards position and maintain this position for about 10 seconds. Repeat this exercise again 10 times.

Exercise to Improve Range of Motion Following Syndesmotic Sprain or Syndesmotic Ankle Sprain
- In this exercise, while in a seated position point the toes down and maintain the position for about 10 seconds and repeat this again 10 times.

Strengthening Exercises for Syndesmotic Sprain or Syndesmotic Ankle Sprain
- The below mentioned exercises should only be done once there has been a substantial improvement in the ankle pain following a syndesmotic sprain or syndesmotic ankle sprain (SAS).
Strengthening Exercise for Syndesmotic Sprain or Syndesmotic Ankle Sprain
- Stand on the edge of a stair, drop the ankles down and maintain this stretching position for about 10 seconds and repeat the exercise about 10 times.

Strengthening Exercise for Syndesmotic Sprain or Syndesmotic Ankle Sprain
- Stand about 10 inches from a wall with the toes pointing towards the wall. Now squat down and maintain this position for about 10 seconds and repeat this maneuver about 10 times.

Isometirc Exercises for Syndesmotic Sprain or Syndesmotic Ankle Sprain
- After achieving near normal range of motion and strength following syndesmotic sprain or a syndesmotic ankle sprain (SAS) then you can start with some isometric exercises by first pushing at a fixed object with the injured ankle. Once this is able to be done with minimal to no pain then the exercises can be advanced by placing resistance and then doing ankle range of motion.
- Place the ankle down and inwards against a fixed object like a couch Place your ankle in the “down and in” position against a fixed object such as a couch. Maintain this position for about 10 seconds and repeat it about 10 times.
- In this exercise, position the ankle upwards and bring it out against a stationary object. Maintain this position for about 10 seconds and repeat it about 10 times.
- This exercise makes use of a resistance band. Take a resistance band and hold the ends of the band in the hands while the band it placed around the foot. Now, try and bring the ankle down as much as possible. Do this for about 10 seconds and repeat it about 10 times. This can also be done by typing the band around a fixed object and then doing this exercise.
Ankle sprain risk factors
- Limited dorsiflexion – (click on the word to see explanation). If your dorsiflexion is limited, this could result in an increase of chance of twisting your ankle.
- High navicular- medial malleolus distance (NMM distance) – If you have a look at the photo below, it is the distance between “D” and the lowest part of “B”. Have a look at this paper.
- Poor proprioception – This will mean that the receptors of your ankle/foot will not inform properly your brain about the position of your foot and, therefore, the risk of getting injured will be higher.
- Higher extension range of motion at the first metatarsophalangeal joint – This means that you can move your toe upwards quite a lot.
- Reduced balance – It can be the result of poor proprioception or due to different conditions.
- Previous ankle sprains – Apparently people who have had previous ankle sprains are prone to have a new one.
- Sport practiced – To be a football/soccer player, due to contact with opponents and to play volleyball or basketball, as they imply a lot of jumping are risk factors, as well.
Living with an ankle sprain
Ankle sprains are common problems, but they do heal. However, you may not be able to return to normal activities right away. It will depend on the grade of your ankle sprain. If your sprain is mild, it might only be 1 to 3 days. If your sprain is moderate or severe, it could be a few weeks. Your doctor can help provide a timeframe for your condition. Once you return, you still may need to wear an ankle brace or bandage for support and protection.
Your doctor or therapist also will provide a list of ankle exercises to do. This will help strengthen your muscles and prevent future sprains. Try the following exercises:
- Ankle circles – Sit on the floor with your legs stretched out in front of you. Move your ankle from side to side, up and down, and around in circles. Do 5 to 10 circles in each direction at least 3 times per day.
- Alphabet letters – Using your big toe as a “pencil,” write the letters of the alphabet in the air. Do the entire alphabet 2 or 3 times.
- Toe raises – Flex your toes back toward you while keeping your knee as straight as you can. Hold for 15 seconds. Do this 10 times.
- Heel raises – Point your toes away from you while keeping your knees as straight as you can. Hold for 15 seconds. Do this 10 times.
- In and out – Turn your injured foot inward until you can’t turn it anymore and hold for 15 seconds. Straighten your foot again. Turn it outward until you can’t turn it anymore and hold for 15 seconds. Do this 10 times in both directions.
- Resistance in and out – Sit on a chair with your leg straight in front of you. Tie the ends of a large elastic exercise band together to make a knot. Wrap the end of the band around the chair leg. Wrap the other end around the bottom of your injured foot. Keep your heel on the ground and slide your foot outward and hold for 10 seconds. Put your foot in front of you again. Slide your foot inward and hold for 10 seconds. Repeat at least 10 times each direction 2 or 3 times per day.
- Step up – Put your injured foot on the first step of a staircase and your other foot on the ground. Slowly straighten the knee of you injured leg while lifting your other foot off the ground. Return to your starting position. Do this 3 to 5 times at least 3 times per day.
- Sitting and standing raises – Sit in a chair with your feet on the ground. Slowly raise your heels while keeping your toes on the ground. Return your heels to the floor. Repeat 10 times at least 2 or 3 times per day. As you get stronger, you can stand on your feet instead of sitting in a chair and raise your heels.
- Balance Exercises – Stand and place a chair next to your uninjured leg to balance you. To start, stand on your injured foot for 30 seconds. You can slowly increase this to up to 3 minutes at a time. Repeat at least 3 times a day. To increase the difficulty, repeat with your eyes closed
Complications of ankle Sprain
Most ankle breaks (fractures) heal uneventfully. Possible early complications include:
- Infection (especially after open fracture).
- Damage to nerves and blood vessels (especially after displaced fracture).
- Compartment syndrome (severe swelling in the leg soon after the injury, putting pressure on nerves and blood vessels).
- Poor healing.
- Damage to skin and soft tissues by a tight or poorly finished cast.
- Burns to the skin as the plaster hardens.
- Failure of bones to knit together and heal well. This can lead to delayed union, union with poor alignment, or complete non-union even after six months.
- Temporary complications of wearing a cast include thinning of the bones and wasting of the muscles, both of which occur significantly even in a 4-6 week period of casting.
- Inflammation of the veins of the lower leg (thrombophlebitis).
- Clotting (thrombosis) of the deep veins of the leg (deep vein thrombosis) which can relate both to reduced mobility and to pressure on the leg veins from swelling and casting.
- Complications of surgical treatment of ankle fracture can include pain from, and infection around, surgical pins (which can in themselves be distressing and frightening).
Possible later complications include
- Osteoarthritis of the ankle.
- Stiffness and loss of flexibility in the ankle.
- Long-term instability of the ankle joint, needing later correction.
- Algodystrophy (also called Sudeck’s atrophy, or complex regional pain syndrome) is a nerve abnormality which can develop after fracture and which leads to continuous burning pain and gradual loss of strength. Treatment is prolonged and difficult.
- In children, damage to the growing parts of the bones of the ankle can affect overall growth
References
