The heart is a muscular organ situated in the center of the chest behind the sternum. It consists of four chambers: the two upper chambers are called the right and left atria, and the two lower chambers are called the right and left ventricles. The right atrium and ventricle together are often called the right heart, and the left atrium and left ventricle together functionally form the left heart.[rx][rx][rx][rx]
The heart provides the body’s organs and tissues with a constant supply of blood – and with it vital oxygen and nutrients. You can think of the heart as a central pump that keeps the blood circulating around the body.
At rest, an adult heart beats about 60 to 80 times a minute. Each time the heart beats it pumps blood through the body. When we exert ourselves physically, our heart beats faster. This increases the speed at which blood flows through our body. The blood can then absorb more oxygen from the lungs per minute in order to supply the body’s cells with more oxygen.
Your heart is about the same size as your fist and weighs around 300 g (about 0.7 pounds). In people who do endurance sports, it can weigh up to 500 g (about 1.1 pounds). The heart is located more or less in the middle of the chest, slightly to the left, behind the breastbone (sternum). You can normally feel someone’s heart beat if you put your hand on their chest.

The heart is a hollow muscle. A wall through the middle (known as the septum) divides it into two halves. Each half has two chambers called the atrium and ventricle. The left ventricle pumps oxygen-rich blood out of the heart and into the body (systemic circulation) through an artery called the aorta. The first blood vessels that branch off from the aorta are the coronary arteries. They go straight to the muscle of the heart itself, and supply the heart with oxygen and nutrients.
The blood that has been “used” by the body – and is then low in oxygen – flows back to the heart. More specifically, it enters the right atrium and from there it flows into the right ventricle. The right ventricle pumps the low-oxygen blood into the pulmonary artery, which leads to the lungs (pulmonary circulation). In the lungs, the blood releases carbon dioxide and picks up oxygen. Then it flows back to the heart through the pulmonary veins – this time to the left side of the heart. From there, the blood is pumped back into the body.
There are 4 heart valves between the right atrium and right ventricle (Tricuspid valve), the left atrium and left ventricle (Mitral valve), and where the blood leaves the heart through the arteries (Pulmonary valve, Aortic valve). They ensure that the blood flows in the right direction and doesn’t flow back.
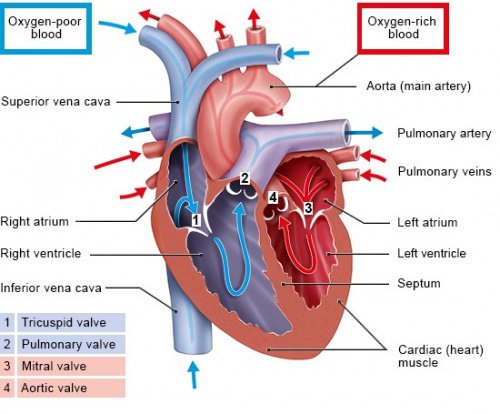
The flow of blood in the heart
Put simply, the valves of the heart function like one-way gates. Each valve is made up of a ring to which two or three flaps of tissue (called cusps or leaflets) are attached. The flaps are always somewhat curved – a bit like sails billowing in the wind. When the blood pushes against these flaps in the direction of the “wind,” they close the valve. When the blood pushes in the other direction, it is able to flow through the valve.
Electrical Events
Cardiac contraction is initiated in the excitable cells of the sinoatrial (SA) node by both spontaneous depolarization and sympathetic activity.
Key Points
The sinoatrial (SA) and atrioventricular (AV) nodes make up the intrinsic conduction system of the heart by setting the rate at which the heartbeats.
The SA node generates action potentials spontaneously.
The SA node fires at a normal rate of 60–100 beats per minute (bpm), and causes depolarization in atrial muscle tissue and subsequent atrial contraction.
The AV node slows the impulses from the SA node, firing at a normal rate of 40-60 bpm, and causes depolarization of the ventricular muscle tissue and ventricular contraction.
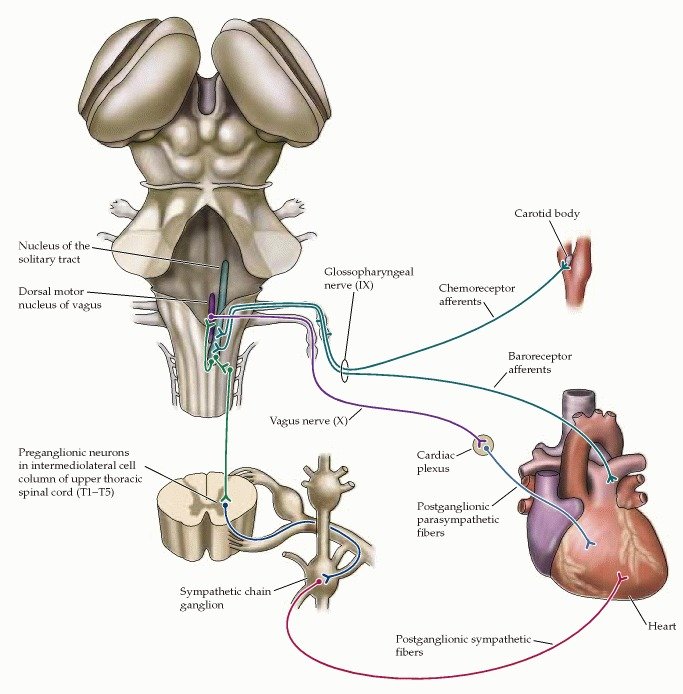
Sympathetic nervous stimulation increases the heart rate, while parasympathetic nervous stimulation decreases the heart rate.
Key Terms
- pacemaker: A structure that sets the rate at which the heartbeats. Under normal conditions, the SA node serves this function for the heart.
- atrioventricular (AV) node: The bundle of conducting tissue that receives impulses from the SA node and delays them before stimulating depolarization in the muscles of the ventricles.
The heart’s activity is dependent on the electrical impulses from the sinoatrial (SA) node and atrioventricular (AV) node, which form the intrinsic conduction system of the heart. The SA and AV nodes act as a pacemaker for the heart, determining the rate at which it beats, even without signals from the larger nervous system of the human body. The SA and AV nodes initiate the electrical impulses that cause contraction within the atria and ventricles of the heart.
Sinoatrial Node
The SA node is a bundle of nerve cells located on the outer layer of the right atria. These cells are specialized to undergo spontaneous depolarization and generation of action potentials without stimulation from the rest of the nervous system. The SA node nerve impulses travel through the atria and cause direct muscle cell depolarization and contraction of the atria. The SA node stimulates the right atria directly and stimulates the left atria through the Bachmann’s bundle. The SA node impulses also travel to the AV node, which stimulates ventricular contraction.
The SA node generates its own action potentials but may be influenced by the autonomic nervous system. Without autonomic nervous stimulation, the SA node will set the heart rate itself, acting as the primary pacemaker for the heart. The SA node fires to set a heart rate in a range of 60–100 beats per minute (bpm), a normal range that varies from person to person.
Atrioventricular Node
The AV node is a bundle of conducting tissue (not formally classified as nerve tissue) located at the junction between the atria and ventricles of the heart. The AV node receives action potentials from the SA node, and transmits them through the bundle of His, left and right bundle branches, and Purkinje fibers, which cause depolarization of ventricular muscle cells leading to ventricular contraction. The AV node slightly slows the neural impulse from the SA node, which causes a delay between depolarization of the atria and the ventricles.
The normal firing rate in the AV node is lower than that of the SA node because it slows the rate of neural impulses. Without autonomic nervous stimulation, it sets the rate of ventricular contraction at 40–60 bpm. Certain types of autonomic nervous stimulation alter the rate of firing in the AV node. Sympathetic nervous stimulation still increases heart rate, while parasympathetic nervous stimulation decreases heart rate by acting on the AV node.

The Cardiac Conduction System: The system of nerves that work together to set the heart rate and stimulate muscle cell depolarization within the heart.
Electrocardiogram and Correlation of ECG Waves with Systole
An electrocardiogram, or ECG, is a recording of the heart’s electrical activity as a graph over a period of time.
Key Points
An ECG is used to measure the rate and regularity of heartbeats as well as the size and position of the chambers, the presence of damage to the heart, and the effects of drugs or devices used to regulate the heart, such as a pacemaker.
The ECG device detects and amplifies the tiny electrical changes on the skin that are caused when the heart muscle depolarizes during each heartbeat, and then translates the electrical pulses of the heart into a graphic representation.
A typical ECG tracing of the cardiac cycle (heartbeat) consists of a P wave (atrial depolarization ), a QRS complex (ventricular depolarization), and a T wave (ventricular repolarization). An additional wave, the U wave ( Purkinje repolarization), is often visible, but not always.
The ST complex is usually elevated during a myocardial infarction.
Atrial fibrillation occurs when the P wave is missing and represents irregular, rapid, and inefficient atrial contraction, but is generally not fatal on its own.
Ventricular fibrillation occurs when all normal waves of an ECG are missing, represents rapid and irregular heartbeats, and will quickly cause sudden cardiac death.
Key Terms
- fibrillation: A condition in which parts of the ECG do not appear normally, representing irregular, rapid, disorganized, and inefficient contractions of the atria or ventricles.
- ST-segment: The line between the QRS complex and the T wave, representing the time when the ventricles are depolarized before repolarization begins.
An electrocardiogram (ECG or EKG) is a recording of the heart’s electrical activity as a graph over a period of time, as detected by electrodes attached to the outer surface of the skin and recorded by a device external to the body. The graph can show the heart’s rate and rhythm. It can also detect enlargement of the heart, decreased blood flow, or the presence of current or past heart attacks. ECGs are the primary clinical tool to measure the electrical and mechanical performance of the heart.
The ECG works by detecting and amplifying tiny electrical changes on the skin that occur during heart muscle depolarization. The output for the ECG forms a graph that shows several different waves, each corresponding to a different electrical and mechanical event within the heart. Changes in these waves are used to identify problems with the different phases of heart activity.

ECG: Illustration of a patient undergoing a 12-lead ECG.
The P Wave

Normal Systole ECG: The U wave is not visible in all ECGs.
The first wave on an ECG is the P wave, indicating atrial depolarization in which the atria contract (atrial systole ). The P wave is the first wave on the ECG because the action potential for the heart is generated in the sinoatrial (SA) node, located on the atria, which sends action potentials directly through Bachmann’s bundle to depolarize the atrial muscle cells.
Increased or decreased P waves can indicate problems with the potassium ion concentration in the body that will alter nerve activity. A missing P wave indicates atrial fibrillation, a cardiac arrhythmia in which the heart beats irregularly, preventing efficient ventricular diastole. This is generally not fatal on its own.
The QRS Complex
The QRS complex refers to the combination of the Q, R, and S waves, and indicates ventricular depolarization and contraction (ventricular systole). The Q and S waves are downward waves while the R wave, an upward wave, is the most prominent feature of an ECG. The QRS complex represents action potentials moving from the AV node, through the bundle of His and left and right branches and Purkinje fibers into the ventricular muscle tissue. Abnormalities in the QRS complex may indicate cardiac hypertrophy or myocardial infarctions.
The T Wave and ST Segment

Animation of a Normal ECG Wave: The red lines represent the movement of the electrical signal through the heart.
The T Wave indicates ventricular repolarization, in which the ventricles relax following depolarization and contraction. The ST segment refers to the gap (flat or slightly upcurved line) between the S wave and the T wave and represents the time between ventricular depolarization and repolarization. An elevated ST segment is the classic indicator for myocardial infarctions, though missing or downward-sloping ST segments may indicate myocardial ischemia.
Following the T wave is the U wave, which represents the repolarization of the Purkinje fibers. It is not always visible on an ECG because it is a very small wave in comparison to the others.
Ventricular Fibrillation
When ECG output shows no identifiable P waves, QRS complexes, or T waves, it indicates ventricular fibrillation, a severe arrhythmia. During ventricular fibrillation, the heart beats extremely fast and irregularly and can no longer pump blood, acting as a mass of quivering, disorganized muscle movements. Ventricular fibrillation will cause sudden cardiac death within minutes unless electrical resuscitation (with an AED) is performed immediately. It generally occurs with myocardial infractions and heart failure and is thought to be caused by action potentials that re-enter the AV nodes from the muscle tissue and induce rapid, irregular, weak contractions of the heart that fail to pump blood.
Heart Sounds
The two major heart sounds are “lub” (from the closure of AV valves) and “dub: (from the closure of aortic and pulmonary valves).
Key Points
The heart tone “lub,” or S1, is caused by the closure of the mitral and tricuspid atrioventricular (AV) valves at the beginning of ventricular systole.
The heart tone “dub,” or S2 ( a combination of A2 and P2), is caused by the closure of the aortic valve and pulmonary valve at the end of ventricular systole.
The splitting of the second heart tone, S2, into two distinct components, A2 and P2, can sometimes be heard in younger people during inspiration. During expiration, the interval between the two components shortens and the tones become merged.
Murmurs are a “whoosh” or “slosh” sound that indicates backflow through the valves.
S3 and S4 are “ta” sounds that indicate ventricles that are either too weak or too stiff to effectively pump blood.
Key Terms
dub: The second heart tone, or S2 (A2 and P2), caused by the closure of the aortic valve and pulmonary valve at the end of ventricular systole.
club: The first heart tone, or S1, caused by the closure of the atrioventricular valves (mitral and tricuspid) at the beginning of ventricular contraction or systole.
Heart murmurs A sound made by backflow of blood through either set of valve that cannot close or open properly.
The closing of the heart valves produces a sound. This sound may be described as either a “lub” or a “dub” sound. Heart sounds are a useful indicator for evaluating the health of the valves and the heart as a whole.
S1
The first heart sound, called S1, makes a “lub” sound caused by the closure of the mitral and tricuspid valves as ventricular systole begins. There is a very slight split between the closure of the mitral and tricuspid valves, but it is not long enough to create multiple sounds.
S2
The second heart sound, called S2, makes a “dub” sound caused by the closure of the semilunar (aortic and pulmonary) valves following ventricular systole. S2 is split because aortic valve closure occurs before pulmonary valve closure. During inspiration (breathing in) there is slightly increased blood return to the right side of the heart, which causes the pulmonary valve to stay open slightly longer than the aortic valve. Due to this, the naming convention is to divide the second sound into two-second sounds, A2 (aortic), and P2 (pulmonary). The time between A2 and P2 is variable depending on the respiratory rate, but the split is generally only prominent in children during inspiration. In adults and during expiration, the split is usually not long enough to suggest two sounds.
Abnormal Heart Sounds
Abnormal heart sounds may indicate problems with the health of the valves. Heart murmurs sound like a “whoosh” or “slosh” and indicate regurgitation or backflow of blood through the valves because they cannot close properly. Heart murmurs are common and generally not serious, but some may be more severe and/or caused by severe underlying problems within the heart. Murmurs may also be caused by valve stenosis (improper opening) and cardiac shunts, a severe condition in which a defect in the septum allows blood to flow between both sides of the heart.
Third and fourth heart sounds, S3 and S4, differ from S1 and S2 because they are caused by abnormal contraction and relaxation of the heart instead of the closure of valves and are more often indicative of more severe problems than are heart murmurs. S3 represents a flabby or weak ventricle that fills with more blood than it is able to pump, while S4 represents a stiff ventricle, such as those found in cardiac hypertrophy. S3 makes a “ta” sound after the “lub-dub” while S4 makes a “ta” sound before the “lub-dub.”

Opening and Closing of Heart Valves: The closing of the heart valves generates the “lub, dub” sounds that can be heard though a stethoscope.
Cardiac Cycle
The cardiac cycle describes the heart’s phases of contraction and relaxation that drive blood flow throughout the body.
Key Points
Every single beat of the heart involves three major stages: cardiac diastole, when chambers are relaxed and filling passively; atrial systole when the atria contract leading to ventricular filling; and ventricular systole when blood is ejected into both the pulmonary artery and aorta.
Pulse is a way of measuring heartbeat, based on the arterial distensions or pulses that occur as blood is pushed through the arteries.
Resting heart rate typically ranges from 60 to 100 bpm (beats per minute). Athletes often have significantly lower than average heart rates while the sedentary and obese typically have elevated heart rates.
Systolic blood pressure is the pressure during heart contraction, while diastolic blood pressure is the pressure during heart relaxation.
The normal range for blood pressure is between 90/60 mmHg and 120/80 mmHg.
Key Terms
- cardiac cycle: The term used to describe the relaxation and contraction that occur as a heart works to pump blood through the body.
- cardiac output: The volume of blood pumped by the heart each minute, calculated as heart rate (HR) X (times) stroke volume (SV).
- pulse: Pressure waves generated by the heart in systole move the arterial walls, creating a palpable pressure wave felt by touch.
The cardiac cycle is the term used to describe the relaxation and contraction that occur as the heart works to pump blood through the body. Heart rate is a term used to describe the frequency of the cardiac cycle. It is considered one of the four vital signs and is a regulated variable. Usually, heart rate is calculated as the number of contractions (heartbeats) of the heart in one minute and expressed as “beats per minute” (bpm). When resting, the adult human heart beats at about 70 bpm (males) and 75 bpm (females), but this varies among individuals. The reference range is normally between 60 bpm (lower is termed bradycardia) and 100 bpm (higher is termed tachycardia). Resting heart rates can be significantly lower in athletes and significantly higher in the obese. The body can increase the heart rate in response to a wide variety of conditions in order to increase the cardiac output, the blood ejected by the heart, which improves oxygen supply to the tissues.
Pulse
Pressure waves generated by the heart in systole, or ventricular contraction, move the highly elastic arterial walls. Forward movement of blood occurs when the arterial wall boundaries are pliable and compliant. These properties allow the arterial wall to distend when pressure increases, resulting in a pulse that can be detected by touch. Exercise, environmental stress, or psychological stress can cause the heart rate to increase above the resting rate. The pulse is the most straightforward way of measuring the heart rate, but it can be a crude and inaccurate measurement when cardiac output is low. In these cases (as happens in some arrhythmias), there is little pressure change and no corresponding change in pulse, and the heart rate may be considerably higher than the measured pulse.
Cardiac Cycle
Every single heartbeat includes three major stages: atrial systole, ventricular systole, and complete cardiac diastole.
- Atrial systole is the contraction of the atria that causes ventricular filling.
- Ventricular systole is the contraction of the ventricles in which blood is ejected into the pulmonary artery or aorta, depending on side.
- Complete cardiac diastole occurs after systole. The blood chambers of the heart relax and fill with blood once more, continuing the cycle.
Systolic and Diastolic Blood Pressure
Throughout the cardiac cycle, the arterial blood pressure increases during the phases of active ventricular contraction and decreases during ventricular filling and atrial systole. Thus, there are two types of measurable blood pressure: systolic during contraction and diastolic during relaxation. Systolic blood pressure is always higher than diastolic blood pressure, generally presented as a ratio in which systolic blood pressure is over diastolic blood pressure. For example, 115/75 mmHg would indicate a systolic blood pressure of 115 mmHg and diastolic blood pressure or 75 mmHg. The normal range for blood pressure is between 90/60 mmHg and 120/80 mmHg. Pressures higher than that range may indicate hypertension, while lower pressures may indicate hypotension. Blood pressure is a regulated variable that is directly related to blood volume, based on cardiac output during the cardiac cycle.

The Cardiac Cycle: Changes in contractility lead to pressure differences in the heart’s chambers that drive the movement of blood.
Contractile Myofilament
The structure of the smooth muscle actomyosin array is similar to striated muscle with several important differences:
-
there is no troponin complex in smooth muscle
-
contraction is regulated by Ca2+ calmodulin-dependent myosin light chain kinase (MLCK) mediated phosphorylation of the regulatory light chains of myosin, which enables actin-myosin interaction and cross-bridge cycling
-
in the absence of Ca2+ and calmodulin (CaM), caldesmon interacts with actomyosin inhibiting the activity of myosin ATPase
-
the activity of myosin light chain phosphatase (MLCP) directly causes the dephosphorylation of myosin LC20 leading to the relaxation
-
the actin: myosin ratio is higher in smooth muscle averaging 15:1 in vascular smooth muscle in comparison to 6:1 in skeletal or cardiac muscle. There are no intercalated disks or z-disks, however, dense bodies in smooth muscle are thought to be analogous to z-disks
Cardiac Output
Cardiac output (Q or CO) is the volume of blood pumped by the heart, in particular by the left or right ventricle, in one minute.
Key Points
Cardiac output, a measure of how much blood the heart pumps over the course of a minute, is calculated by multiplying heart rate by stroke volume.
The heart rate is increased by sympathetic nervous stimulation and decreased by parasympathetic nervous stimulation.
Stroke volume is end-diastolic volume (venous return) minus end-systolic volume, the amount of blood left over in the heart after systole.
The ejection fraction is stroke volume divided by end-diastolic volume.
Mean arterial blood pressure is cardiac output multiplied by total peripheral resistance. A twofold change in vascular size will cause a 16-fold change in resistance in the opposite direction.
Starling’s mechanism states that changes in venous return (preload) to the heart will change cardiac output, which will also change mean arterial blood pressure in the same direction. This means that blood volume and blood pressure are directly related to one another.
Key Terms
- mean arterial blood pressure: A measure of blood pressure based on cardiac output and vascular resistance.
- cardiac output: The volume of blood pumped by the heart, in particular by the left or right ventricle, in the time interval of one minute.
Cardiac output (CO) is a measure of the heart’s performance. While there are many clinical techniques to measure CO, it is best described as a physiological and mathematical relationship between different variables. When one of the variables changes, CO as a whole will change as a result. This can also be used to predict other regulated variables, such as blood pressure and blood volume. The mathematical description of CO is that CO=Heart Rate (HR)×Stroke Volume (SV). Changes in HR, SV, or their components, will change CO.
Heart Rate
The heart rate is determined by spontaneous action potential generation in the sinoatrial (SA) node and conduction in the atrioventricular (AV) node. It refers to the number of heartbeats over the course of a minute. Sympathetic nervous system activation will stimulate the SA and AV nodes to increase the heart rate, which will increase cardiac output. Parasympathetic nervous system activation will conversely act on the SA and AV nodes to decrease the heart rate, which will decrease cardiac output. For the SA node, the rate of depolarization is altered, while the AV node’s rate of conduction is altered by autonomic nerve stimulation.
Stroke Volume
Stroke volume refers to the amount of blood ejected from the heart during a single beat. It is a measure of the contractility of the heart based on end-diastolic volume (EDV), mathematically described as SV=EDV−ESV (end-systolic volume. EDV is the volume of blood in the ventricles at the end of diastole, while ESV is the volume of blood left inside the ventricles at the end of systole, making SV the difference between EDV and ESV. Contractility of the heart refers to the variability in how much blood the heart ejects based on changes in stroke volume rather than changes in heart rate.
Additionally, another indicator known as the ejection fraction (EF) is used to evaluate stroke volume and contractility. It is described as EF=(SVEDV)×100% and is a measure of the proportion of blood ejected during systole compared to the amount of blood that was present in the heart. A higher EF suggests more efficient heart activity.
Mean Arterial Pressure
Cardiac output is an indicator of mean arterial blood pressure (MAP), the average measure of blood pressure within the body. It is described as MAP=CO×TPR (total peripheral resistance). TPR is a measure of resistance in the blood vessels, which acts as the force by which blood must overcome to flow through the arteries determined by the diameter of the blood vessels. The exact relationship is such that a twofold increase in blood vessel diameter (doubling the diameter) would decrease resistance by 16-fold, and the opposite is true as well. When CO increases, MAP will increase, but if CO decreases, MAP will decrease.
Starling’s Law of the Heart

Frank Starling’s Law: This chart indicates stroke volume compared to ventricular preload, with labels for preload dependent zone, responsive patient SVV > 10%, and nonresponsive patient SVV < 10 %.
CO can also predict blood pressure based on blood volume. Starling’s law of the heart states that the SV of the heart increases in response to an increase in EDV when all other factors remain constant. Essentially, this means that higher venous blood return to the heart (also called the preload) will increase SV, which will in turn increase CO. This is because sarcomeres are stretched further when EDV increases, allowing the heart to eject more blood and keep the same ESV if no other factors change.
The main implication of this law is that increases in blood volume or blood return to the heart will increase cardiac output, which will lead to an increase in MAP. The opposite scenario is true as well. For example, a dehydrated person will have a low blood volume and lower venous return to the heart, which will decrease cardiac output and blood pressure. Those that stand up quickly after lying down may feel light-headed because their venous return to the heart is momentarily impaired by gravity, temporarily decreasing blood pressure and supply to the brain. The adjustment for blood pressure is a quick process, while blood volume is slowly altered. Blood volume itself is another regulated variable, regulated slowly through complex processes in the renal system that alter blood pressure based on the Starling mechanism.
What is cardiac muscle?
Cardiac muscle tissue is one of the three types of muscle tissue in your body. The other two types are skeletal muscle tissue and smooth muscle tissue. Cardiac muscle tissue is only found in your heart, where it performs coordinated contractions that allow your heart to pump blood through your circulatory system.
Keep reading to learn more about the function and structure of cardiac muscle tissue, as well as conditions that affect this type of muscle tissue.
How does it function?
Cardiac muscle tissue works to keep your heart pumping through involuntary movements. This is one feature that differentiates it from skeletal muscle tissue, which you can control.
It does this through specialized cells called pacemaker cells. These control the contractions of your heart. Your nervous system sends signals to pacemaker cells that prompt them to either speed up or slow down your heart rate.
Your pacemaker cells are connected to other cardiac muscle cells, allowing them to pass along signals. This results in a wave of contractions of your cardiac muscle, which creates your heartbeat.
What does cardiac muscle tissue look like when it moves?
Use this interactive 3-D diagram to explore the movement of cardiac muscle tissue
What are heart muscles made of?
Intercalated discs
Intercalated discs are small connections that join cardiac muscle cells (cardiomyocytes) to each other.
Gap junctions
Gap junctions are part of the intercalated discs. When one cardiac muscle cell is stimulated to contract, a gap junction transfers the stimulation to the next cardiac cell. This allows the muscle to contract in a coordinated way.
Desmosomes
Like gap junctions, desmosomes are also found within intercalated discs. They help hold the cardiac muscle fibers together during a contraction.
Nucleus
The nucleus is the “control center” of a cell. It contains all of the cell’s genetic material. While skeletal muscle cells can have multiple nuclei, cardiac muscle cells typically only have one nucleus.
What is cardiomyopathy?
Cardiomyopathy is one of the main conditions that can affect your cardiac muscle tissue. It’s a disease that makes it harder for your heart to pump blood.
There are several different types of cardiomyopathy:
- Hypertrophic cardiomyopathy. The cardiac muscles enlarge and thicken for no apparent reason. It’s usually found in the lower chambers of the heart, called the ventricles.
- Dilated cardiomyopathy. The ventricles become larger and weaker. This makes it hard for them to pump, which makes the rest of your heart work harder to pump blood.
- Restrictive cardiomyopathy. The ventricles become stiff, which prevents them from filling to their full volume.
- Arrhythmogenic right ventricular dysplasia. The cardiac muscle tissue of your right ventricle is replaced with fatty or fiber-rich tissue. This can lead to arrhythmia, which refers to an abnormal heart rate or rhythm.
Not all cases of cardiomyopathy produce symptoms. However, it can sometimes cause:
- trouble breathing, especially when exercising
- fatigue
- swollen ankles, feet, legs, abdomen, or neck veins
It’s usually hard to pinpoint the cause of cardiomyopathy. But several things can increase your risk of developing it, including:
- a family history of cardiomyopathy or heart failure
- high blood pressure
- obesity
- heavy alcohol consumption
- use of certain recreational drugs
- past heart attacks or heart infections
How does exercise impact cardiac muscle tissue?
As with many other muscles in your body, exercise can strengthen your cardiac muscle. Exercise can also help reduce your risk of developing cardiomyopathy and make your heart work more efficiently.
The American Heart Association recommends at least 150 minutes of moderate exercise per week. To reach this goal, try to get about 30 minutes of exercise five days a week.
As for the type of exercise, cardio workouts are named for their cardiac muscle benefits. Regular cardio exercise can help lower your blood pressure, reduce your heart rate, and make your heart pump more effectively. Common types of cardio exercises include walking, running, biking, and swimming.
If you already have a heart condition, make sure to talk to your doctor before starting any kind of exercise program. You might need to take some precautions to avoid putting too much stress on your heart.
Cardiac muscle tissue is one of the three types of muscle in your body. It’s only found in your heart, where it’s involved in coordinated contractions that keep your heart beating. To keep your cardiac muscle working efficiently and to reduce your risk of cardiac conditions — including cardiomyopathy — try to get in some sort of exercise more days of the week than not.
How Your Heart Works
Your heart
The human heart is one of the hardest-working organs in the body.
On average, it beats around 75 times a minute. As the heartbeats, it provides pressure so blood can flow to deliver oxygen and important nutrients to tissue all over your body through an extensive network of arteries, and it has return blood flow through a network of veins.
In fact, the heart steadily pumps an average of 2,000 gallons of blood through the body each day.
Your heart is located underneath your sternum and ribcage, and between your two lungs.
The heart’s chambers
The heart’s four chambers function as a double-sided pump, with an upper and continuous lower chamber on each side of the heart.
The heart’s four chambers are:
- Right atrium. This chamber receives venous oxygen-depleted blood that has already circulated around through the body, not including the lungs, and pumps it into the right ventricle.
- Right ventricle. The right ventricle pumps blood from the right atrium to the pulmonary artery. The pulmonary artery sends the deoxygenated blood to the lungs, where it picks up oxygen in exchange for carbon dioxide.
- Left atrium. This chamber receives oxygenated blood from the pulmonary veins of the lungs and pumps it to the left ventricle.
- Left ventricle. With the thickest muscle mass of all the chambers, the left ventricle is the hardest pumping part of the heart, as it pumps blood that flows to the heart and the rest of the body other than the lungs.
The heart’s two atria are both located on the top of the heart. They are responsible for receiving blood from your veins.
The heart’s two ventricles are located at the bottom of the heart. They are responsible for pumping blood into your arteries.
Your atria and ventricles contract to make your heartbeat and to pump the blood through each chamber. Your heart chambers fill up with blood before each beat, and the contraction pushes the blood out into the next chamber. The contractions are triggered by electrical pulses that start from the sinus node, also called the sinoatrial node (SA node), located in the tissue of your right atrium.
The pulses then travel through your heart to the atrioventricular node, also called the AV node, located near the center of the heart between the atria and the ventricles. These electrical impulses keep your blood flowing in proper rhythm.
The heart’s valves
The heart has four valves, one each at the downstream end of each chamber, so that, under normal conditions, blood can’t flow backward, and the chambers can fill with blood and pump blood forward properly. These valves can sometimes be repaired or replaced if they become damaged.
The heart’s valves are:
- Tricuspid (right AV) valve. This valve opens to allow blood to flow from the right atrium to the right ventricle.
- Pulmonary valve. This valve opens to allow blood to flow from the left ventricle into the pulmonary artery to the lungs so that the heart and rest of the body can receive more oxygen.
- Mitral (left AV) valve. This valve opens to let blood flow from the left atrium to the left ventricle.
- Aortic valve. This valve opens to let blood leave the left ventricle so that the blood can flow to the heart and the rest of the body, save the lungs.
Blood flow through the heart
When working properly, deoxygenated blood coming back from organs, other than the lungs, enters the heart through two major veins known as the vena cavae, and the heart returns its venous blood back to itself through the coronary sinus.
From these venous structures, the blood enters the right atrium and passes through the tricuspid valve into the right ventricle. The blood then flows through the pulmonary valve into the pulmonary artery trunk, and next travels through the right and left pulmonary arteries to the lungs, where the blood receives oxygen during air exchange.
On its way back from the lungs, the oxygenated blood travels through the right and left pulmonary veins into the left atrium of the heart. The blood then flows through the mitral valve into the left ventricle, the heart’s powerhouse chamber.
The blood travels out the left ventricle through the aortic valve, and into the aorta, extending upward from the heart. From there, the blood moves through a maze of arteries to get to every cell in the body other than the lungs.
The heart’s crown
The structure of the heart’s blood supply is called the coronary circulatory system. The word “coronary” comes from the Latin word meaning “of a crown.” The arteries that fuel the heart’s muscle encircle the heart like a crown.
Coronary heart disease, also called coronary artery disease, typically develops when calcium-containing cholesterol and fat plaques collect in and hurt the arteries that feed the heart muscle. If a portion of one of these plaques ruptures, it can suddenly block one of the vessels and cause the heart muscle to begin to die (myocardial infarction) because it’s starved for oxygen and nutrients. This can also occur if a blood clot forms in one of the arteries of the heart, which can happen right after a plaque rupture.
Fun Facts About the Heart You Didn’t Know
How the heart works
The heart is part of your body’s circulatory system. It’s made up of the atria, ventricles, valves, and various arteries and veins. The main function of your heart is to keep blood that’s full of oxygen circulating throughout your body. Because your heart is crucial to your survival, it’s important to keep it healthy with a well-balanced diet and exercise, and avoid things that can damage it, like smoking.
While you’re probably familiar with a few heart-healthy tips, there are some fun facts about the heart that you may not know.
24 fun facts about the heart
- The average heart is the size of a fist in an adult.
- Your heart will beat about 115,000 times each day.
- Your heart pumps about 2,000 gallons of blood every day.
- An electrical system controls the rhythm of your heart. It’s called the cardiac conduction system.
- The heart can continue beating even when it’s disconnected from the body.
- The first open-heart surgery occurred in 1893. It was performed by Daniel Hale Williams, who was one of the few black cardiologists in the United States at the time.
- The first implantable pacemaker was used in 1958. Arne Larsson, who received the pacemaker, lived longer than the surgeon who implanted it. Larsson died at 86 of a disease that was unrelated to his heart.
- The youngest person to receive heart surgery was only a minute old. She had a heart defect that many babies don’t survive. Her surgery was successful, but she’ll eventually need a heart transplant.
- The earliest known case of heart disease was identified in the remains of a 3,500-year-old Egyptian mummy.
- The fairy fly, which is a kind of wasp, has the smallest heart of any living creature.
- The American pygmy shrew is the smallest mammal, but it has the fastest heartbeat at 1,200 beats per minute.
- Whales have the largest heart of any mammal.
- The giraffe has a lopsided heart, with their left ventricle being thicker than the right. This is because the left side has to get blood up the giraffe’s long neck to reach their brain.
- Most heart attacks happen on a Monday.
- Christmas day is the most common day of the year for heart attacks to happen.
- The human heart weighs less than 1 pound. However, a man’s heart, on average, is 2 ounces heavier than a woman’s heart.
- A woman’s heart beats slightly faster than a man’s heart.
- The beating sound of your heart is caused by the valves of the heart opening and closing.
- It’s possible to have a broken heart. It’s called broken heart syndrome and can have similar symptoms as a heart attack. The difference is that a heart attack is from heart disease and broken heart syndrome is caused by a rush of stress hormones from an emotional or physical stress event.
- Death from a broken heart, or broken heart syndrome, is possible but extremely rare.
- The iconic heart shape as a symbol of love is traditionally thought to come from the silphium plant, which was used as an ancient form of birth control.
- If you were to stretch out your blood vessel system, it would extend over 60,000 miles.
- Heart cells stop dividing, which means heart cancer is extremely rare.
- Laughing is good for your heart. It reduces stress and gives a boost to your immune system.
Your heart affects every part of your body. That also means that diet, lifestyle, and your emotional well-being can affect your heart. Emotional and physical health are both important for maintaining a healthy heart.
28 Healthy Heart Tips
There are many steps you can take to help protect your health and blood vessels. Avoiding tobacco is one of the best.
In fact, smoking is one of the top controllable risk factors for heart disease. If you smoke or use other tobacco products, the American Heart Association (AHA), National Heart, Lung, and Blood InstituteTrusted Source (NHLBI), and Centers for Disease Control and PreventionTrusted Source (CDC) all encourage you to quit. It can make a huge difference to not just your heart, but your overall health, too.
Focus on the middle
That is, focus on your middle. Research in the Journal of the American College of Cardiology has linked excess belly fat to higher blood pressure and unhealthy blood lipid levels. If you’re carrying extra fat around your middle, it’s time to slim down. Eating fewer calories and exercising more can make a big difference.
Play between the sheets
Or you can play on top of the sheets! That’s right, having sex can be good for your heart. Sexual activity may add more than just pleasure to your life. It may also help lower your blood pressure and risk of heart disease. Research published in the American Journal of CardiologyTrusted Source shows that a lower frequency of sexual activity is associated with higher rates of cardiovascular disease.
Knit a scarf
Put your hands to work to help your mind unwind. Engaging in activities such as knitting, sewing, and crocheting can help relieve stress and do your ticker some good. Other relaxing hobbies, such as woodworking, cooking, or completing jigsaw puzzles, may also help take the edge off stressful days.
Power up your salsa with beans
When paired with low-fat chips or fresh veggies, salsa offers a delicious and antioxidant-rich snack. Consider mixing in a can of black beans for an added boost of heart-healthy fiber. According to the Mayo Clinic, a diet rich in soluble fiber can help lower your level of low-density lipoprotein, or “bad cholesterol.” Other rich sources of soluble fiber include oats, barley, apples, pears, and avocados.
Whether you prefer a rumba beat or two-step tune, dancing makes for a great heart-healthy workout. Like other forms of aerobic exercise, it raises your heart rate and gets your lungs pumping. It also burns up to 200 calories or more per hour, reports the Mayo Clinic.
Go fish
Eating a diet rich in omega-3 fatty acids can also help ward off heart disease. Many fish, such as salmon, tuna, sardines, and herring, are rich sources of omega-3 fatty acids. Try to eat fish at least twice a week, suggests the AHA. If you’re concerned about mercury or other contaminants in fish, you may be happy to learn that its heart-healthy benefits tend to outweigh the risks for most people.
Laugh out loud
Don’t just LOL in emails or Facebook posts. Laugh out loud in your daily life. Whether you like watching funny movies or cracking jokes with your friends, laughter may be good for your heart. According to the AHA, research suggests laughing can lower stress hormones, decrease inflammation in your arteries, and raise your levels of high-density lipoprotein (HLD), also known as “good cholesterol.”
Stretch it out
Yoga can help you improve your balance, flexibility, and strength. It can help you relax and relieve stress. As if that’s not enough, yoga also has the potential to improve heart health. According to research published in the Journal of Evidence-Based Complementary & Alternative MedicineTrusted Source, yoga demonstrates the potential to reduce your risk of cardiovascular disease.
Raise a glass
Moderate consumption of alcohol can help raise your levels of HDL or good cholesterol. It can also help prevent blood clot formation and artery damage. According to the Mayo Clinic, red wine, in particular, may offer benefits for your heart. That doesn’t mean you should guzzle it at every meal. The key is to only drink alcohol in moderation.
Sidestep salt
If the entire U.S. population reduced its average salt intake to just half a teaspoon a day, it would significantly cut the number of people who develop coronary heart disease every year, report researchers in the New England Journal of Medicine. The authors suggest that salt is one of the leading drivers of rising healthcare costs in the United States. Processed and restaurant-prepared foods tend to be especially high in salt. So think twice before filling up on your favorite fast-food fix. Consider using a salt substitute, such as Dash, if you have high blood pressure or heart failure.
Move it, move it, move it
No matter how much you weigh, sitting for long periods of time could shorten your lifespan, warn researchers in the Archives of Internal Medicine and the American Heart AssociationTrusted Source. Couch potato and desk jockey lifestyles seem to have an unhealthy effect on blood fats and blood sugar. If you work at a desk, remember to take regular breaks to move around. Go for a stroll on your lunch break, and enjoy regular exercise in your leisure time.
Know your numbers
Keeping your blood pressure, blood sugar, cholesterol, and triglycerides in check is important for good heart health. Learn the optimal levels for your sex and age group. Take steps to reach and maintain those levels. And remember to schedule regular check-ups with your doctor. If you want to make your doctor happy, keep good records of your vitals or lab numbers, and bring them to your appointments.
Eat chocolate
Dark chocolate not only tastes delicious, it also contains heart-healthy flavonoids. These compounds help reduce inflammation and lower your risk of heart disease, suggest scientists in the journal Nutrients. Eaten in moderation, dark chocolate — not oversweetened milk chocolate — can actually be good for you. The next time you want to indulge your sweet tooth, sink it into a square or two of dark chocolate. No guilt required.
Kick your housework up a notch
Vacuuming or mopping the floors may not be as invigorating as a Body Slam or Zumba class. But these activities and other household chores do get you moving. They can give your heart a little workout while burning calories too. Put your favorite music on and add some pep to your step while you complete your weekly chores.
Go nuts
Almonds, walnuts, pecans, and other tree nuts deliver a powerful punch of heart-healthy fats, protein, and fiber. Including them in your diet can help lower your risk of cardiovascular disease. Remember to keep the serving size small, suggests the AHA. While nuts are full of healthy stuff, they’re also high in calories.
Be a kid
Fitness doesn’t have to be boring. Let your inner child take the lead by enjoying an evening of roller skating, bowling, or laser tag. You can have fun while burning calories and giving your heart a workout.
Consider pet therapy
Our pets offer more than good company and unconditional love. They also provide numerous health benefits. Studies reported by the National Institutes of Health (NIH) suggest that owning a pet may help improve your heart and lung function. It may also help lower your chances of dying from heart disease.
Start and stop
Start and stop, then start and stop again. During interval training, you alternate bursts of intense physical activity with bouts of lighter activity. The Mayo Clinic reports that doing so can boost the number of calories you burn while working out.
Cut the fat
Slicing your saturated fat intake to no more than 7 percent of your daily calories can cut your risk of heart disease, advises the USDA. If you don’t normally read nutrition labels, considering starting today. Take stock of what you’re eating and avoid foods that are high in saturated fat.
Take the scenic route home
Put down your cell phone, forget about the driver who cut you off, and enjoy your ride. Eliminating stress while driving can help lower your blood pressure and stress levels. That’s something your cardiovascular system will appreciate.
Make time for breakfast
The first meal of the day is an important one. Eating a nutritious breakfast every day can help you maintain a healthy diet and weight. To build a heart-healthy meal, reach for:
- whole grains, such as oatmeal, whole-grain cereals, or whole-wheat toast
- lean protein sources, such as turkey bacon or a small serving of nuts or peanut butter
- low-fat dairy products, such as low-fat milk, yogurt, or cheese
- fruits and vegetables
Take the stairs
Exercise is essential for good heart health, so why not sneak it in at every opportunity? Take the stairs instead of the elevator. Park on the far side of the parking lot. Walk to a colleague’s desk to talk, instead of emailing them. Play with your dog or kids at the park, instead of just watching them. Every little bit adds up to better fitness.
Brew up a heart-healthy potion
No magic is needed to brew up a cup of green or black tea. Drinking one to three cups of tea per day may help lower your risk of heart problems, reports the AHA. For example, it’s linked to lower rates of angina and heart attacks.
Brush your teeth regularly
Good oral hygiene does more than keep your teeth white and glistening. According to the Cleveland Clinic, some research suggests that the bacteria that cause gum disease can also raise your risk of heart disease. While the research findings have been mixed, there’s no downside to taking good care of your teeth and gums.
Walk it off
The next time you feel overwhelmed, exasperated, or angry, take a stroll. Even a five-minute walk can help clear your head and lower your stress levels, which is good for your health. Taking a half-hour walk every day is even better for your physical and mental health.
Pump some iron
Aerobic fitness is key to keeping your heart healthy, but it’s not the only type of exercise you should do. It’s also important to include regular strength training sessions in your schedule. The more muscle mass you build, the more calories you burn. That can help you maintain a heart-healthy weight and fitness level.
Find your happy place
A sunny outlook may be good for your heart, as well as your mood. According to the Harvard T. H. Chan School of Public Health, chronic stress, anxiety, and anger can raise your risk of heart disease and stroke. Maintaining a positive outlook on life may help you stay healthier for longer.
Cardiomyopathy
What is cardiomyopathy?
Cardiomyopathy is a progressive disease of the myocardium or heart muscle. In most cases, the heart muscle weakens and is unable to pump blood to the rest of the body as well as it should. There are many different types of cardiomyopathy caused by a range of factors, from coronary heart disease to certain drugs. These can all lead to an irregular heartbeat, heart failure, a heart valve problem, or other complications.
Medical treatment and follow-up care are important. They can help prevent heart failure or other complications.
What are the types of cardiomyopathy?
Cardiomyopathy generally has four types.
Dilated cardiomyopathy
The most common form, dilated cardiomyopathy (DCM), occurs when your heart muscle is too weak to pump blood efficiently. The muscles stretch and become thinner. This allows the chambers of your heart to expand.
This is also known as an enlarged heart. You can inherit it, or it can be due to coronary artery disease.
Hypertrophic cardiomyopathy
Hypertrophic cardiomyopathy is believed to be genetic. It occurs when your heart walls thicken and prevent blood from flowing through your heart. It’s a fairly common type of cardiomyopathy. It can also be caused by long-term high blood pressure or aging. Diabetes or thyroid disease can also cause hypertrophic cardiomyopathy. There are other instances that the cause is unknown.
Arrhythmogenic right ventricular dysplasia (ARVD)
Arrhythmogenic right ventricular dysplasia (ARVD) is a very rare form of cardiomyopathy, but it’s the leading cause of sudden death in young athletes. In this type of genetic cardiomyopathy, fat and extra fibrous tissue replace the muscle of the right ventricle. This causes abnormal heart rhythms.
Restrictive cardiomyopathy
Restrictive cardiomyopathy is the least common form. It occurs when the ventricles stiffen and can’t relax enough to fill up with blood. Scarring of the heart, which frequently occurs after a heart transplant, may be a cause. It can also occur as a result of heart disease.
Other types
Most of the following types of cardiomyopathy belong to one of the previous four classifications, but each has unique causes or complications.
Peripartum cardiomyopathy occurs during or after pregnancy. This rare type occurs when the heart weakens within five months of delivery or within the final month of pregnancy. When it occurs after delivery, it’s sometimes called postpartum cardiomyopathy. This is a form of dilated cardiomyopathy, and it’s a life-threatening condition. There’s no cause.
Alcoholic cardiomyopathy is due to drinking too much alcohol over a long period of time, which can weaken your heart so it can no longer pump blood efficiently. Your heart then becomes enlarged. This is a form of dilated cardiomyopathy.
Ischemic cardiomyopathy occurs when your heart can no longer pump blood to the rest of your body due to coronary artery disease. Blood vessels to the heart muscle narrow and become blocked. This deprives the heart muscle of oxygen. Ischemic cardiomyopathy is a common cause of heart failure. Alternatively, nonischemic cardiomyopathy is any form that isn’t related to coronary artery disease.
Noncompaction cardiomyopathy also called spongiform cardiomyopathy, is a rare disease present at birth. It results from abnormal development of the heart muscle in the womb. Diagnosis may occur at any stage of life.
Who is at risk for cardiomyopathy?
Cardiomyopathy can affect people of all ages. Major risk factors include the following:
- a family history of cardiomyopathy, sudden cardiac arrest, or heart failure
- coronary heart disease
- diabetes
- severe obesity
- sarcoidosis
- hemochromatosis
- amyloidosis
- heart attack
- long-term high blood pressure
- alcoholism
According to research, HIV, HIV treatments, and dietary and lifestyle factors can also increase your risk of cardiomyopathy. HIV can increase your risk of heart failure and dilated cardiomyopathy, in particular. If you have HIV, talk to your doctor about regular tests to check the health of your heart. You should also follow a heart-healthy diet and exercise program.
What are the symptoms of cardiomyopathy?
The symptoms of all types of cardiomyopathy tend to be similar. In all cases, the heart can’t adequately pump blood to the tissues and organs of the body. It can result in symptoms such as:
- general weakness and fatigue
- shortness of breath, particularly during exertion or exercise
- lightheadedness and dizziness
- chest pain
- heart palpitations
- fainting attacks
- high blood pressure
- edema, or swelling, of your feet, ankles, and legs
What is the treatment for cardiomyopathy?
Treatment varies depending on how damaged your heart is due to cardiomyopathy and the resulting symptoms.
Some people may not require treatment until symptoms appear. Others who are beginning to struggle with breathlessness or chest pain may need to make some lifestyle adjustments or take medications.
You can’t reverse or cure cardiomyopathy, but you can control it with some of the following options:
- heart-healthy lifestyle changes
- medications, including those used to treat high blood pressure, prevent water retention, keep the heart beating with a normal rhythm, prevent blood clots, and reduce inflammation
- surgically implanted devices, like pacemakers and defibrillators
- surgery
- heart transplant, which is considered a last resort
The goal of treatment is to help your heart be as efficient as possible and to prevent further damage and loss of function.
What is the long-term outlook?
Cardiomyopathy can be life-threatening and can shorten your life expectancy if severe damage occurs early on. The disease is also progressive, which means it tends to get worse over time. Treatments can prolong your life. They can do this by slowing the decline of your heart’s condition or by providing technologies to help your heart do its job.
Those with cardiomyopathy should make several lifestyle adjustments to improve heart health. These may include:
- maintaining a healthy weight
- eating a modified diet
- limiting caffeine intake
- getting enough sleep
- managing stress
- quitting smoking
- limiting alcohol intake
- getting support from their family, friends, and doctor
One of the biggest challenges is sticking with a regular exercise program. Exercise can be very tiring for someone with a damaged heart. However, exercise is extremely important for maintaining a healthy weight and prolonging heart function. It’s important to check with your doctor and engage in a regular exercise program that’s not too taxing but that gets you moving every day.
The type of exercise that’s best for you will depend on the type of cardiomyopathy you have. Your doctor will help you determine an appropriate exercise routine, and they’ll tell you the warning signs to watch out for while exercising.
Warning Signs of a Heart Attack
Did you know that you can have a heart attack without feeling any chest pain? Heart failure and heart disease don’t show the same signs for everyone, especially women.
The heart is a muscle that contracts to pump blood throughout the body. A heart attack (often called a myocardial infarction) occurs when the heart muscle doesn’t get enough blood. Blood carries oxygen and nutrients to the heart muscle. When there isn’t enough blood flowing to your heart muscle, the affected part can get damaged or die. This is dangerous and sometimes deadly.
Heart attacks happen suddenly, but they normally result from long-standing heart disease. Typically, a waxy plaque builds up on the walls inside your blood vessels that feed the heart muscle. Sometimes a chunk of the plaque, called a blood clot, breaks off and prevents blood from passing through the vessel to your heart muscle, resulting in a heart attack.
Less commonly, something like stress, physical exertion, or cold weather causes the blood vessel to contract or spasm, which decreases the amount of blood that can get to your heart muscle.
There are many risk factors that contribute to having a heart attack, including:
- age
- heredity
- high blood pressure
- high cholesterol
- obesity
- poor diet
- excessive alcohol consumption (on a regular basis: more than one drink per day for women and more than two drinks per day for men)
- stress
- physical inactivity
A heart attack is a medical emergency. It’s really important to listen to what your body is telling you if you think you might be having one. It’s better to seek emergency medical treatment and be wrong than to not get help when you’re having a heart attack.
Chest pain, pressure, and discomfort
Most people with heart attacks experience some sort of chest pain or discomfort. But it’s important to understand that chest pains don’t occur in every heart attack.
Chest pain is a common sign of a heart attack. People have described this sensation as feeling like an elephant is standing on their chest.
Some people don’t describe chest pain as pain at all. Instead, they may say they felt chest tightness or squeezing. Sometimes this discomfort can seem bad for a few minutes and then go away. Sometimes the discomfort comes back hours or even a day later. These could all be signs your heart muscle isn’t getting enough oxygen.
If you experience chest pains or tightness, you or someone around you should call 911 immediately.
Not just chest pain
Pain and tightness can also radiate in other areas of the body. Most people associate a heart attack with pain working its way down the left arm. That can happen, but pain can also appear in other locations, including:
- upper abdomen
- shoulder
- back
- neck/throat
- teeth or jaw
According to the American Heart Association, women tend to report heart attacks that cause pain specifically in the lower abdomen and lower portion of the chest.
The pain may not be concentrated in the chest at all. It could feel like pressure in the chest and pain in other parts of the body. Upper back pain is another symptom women more commonly cite than men.
Sweating day and night
Sweating more than usual — especially if you aren’t exercising or being active — could be an early warning sign of heart problems. Pumping blood through clogged arteries takes more effort from your heart, so your body sweats more to try to keep your body temperature down during the extra exertion. If you experience cold sweats or clammy skin, then you should consult your doctor.
Night sweats are also a common symptom for women experiencing heart troubles. Women may mistake this symptom for an effect of menopause. However, if you wake up and your sheets are soaked or you cannot sleep due to your sweating, this could be a sign of a heart attack, especially in women.
Fatigue
Fatigue can be a less commonly recognized heart attack sign in women. According to the American Heart Association, some women may even think their heart attack symptoms are flu-like symptoms.
A heart attack can cause exhaustion due to the extra stress on your heart to try to pump while an area of blood flow is blocked. If you often feel tired or exhausted for no reason, it could be a sign that something is wrong.
Fatigue and shortness of breath are more common in women than men and may begin months before a heart attack. That’s why it’s important to see a doctor as early as possible when you experience early signs of fatigue.
Shortness of breath
Your breathing and your heart pumping blood effectively are very closely related. Your heart pumps blood so it can circulate to your tissues as well as get oxygen from your lungs. If your heart can’t pump blood well (as is the case with a heart attack), you can feel short of breath.
Shortness of breath can sometimes be an accompanying symptom of unusual fatigue in women. For example, some women report they would get unusually short of breath and tired from the activity they were performing. Going to the mailbox could leave them exhausted and unable to catch their breath. This can be a common sign of heart attack in women.
Lightheadedness
Lightheadedness and dizziness can occur with a heart attack and are often symptoms women describe. Some women report they feel like they might pass out if they try to stand up or overexert themselves. This sensation is certainly not a normal feeling and shouldn’t be ignored if you experience it.
Heart palpitations
Heart palpitations can range from feeling like your heart is skipping a beat to having changes in heart rhythm that can feel like your heart is pounding or throbbing. Your heart and body rely on a consistent, steady beat to best move blood throughout your body. If the beat gets out of rhythm, this could be a sign you’re having a heart attack.
Heart palpitations due to a heart attack can create a sense of unease or anxiety, especially in women. Some people may describe heart palpitations as a sensation their heart is pounding in their neck, not just their chest.
Changes in your heart’s rhythm shouldn’t be ignored, because once the heart is consistently out of rhythm, it requires medical intervention to get back into rhythm. If your palpitations are accompanied by dizziness, chest pressure, chest pain, or fainting, they could be confirmation that a heart attack is occurring.
Indigestion, nausea, and vomiting
Often people begin experiencing mild indigestion and other gastrointestinal problems before a heart attack. Because heart attacks usually occur in older people who typically have more indigestion problems, these symptoms can get dismissed as heartburn or another food-related complication.
If you normally have an iron stomach, indigestion or heartburn could be a signal that something else is going on.
What you should do during a heart attack
If you think you are having a heart attack, you or someone nearby should call emergency services immediately. It’s unsafe to drive yourself to the hospital during a heart attack, so call an ambulance. While you may feel awake and alert enough to drive, the chest pain could get so severe that you may have trouble breathing or difficulty thinking clearly.
After you call emergency services
When you call emergency services, the dispatcher may ask you about the medicines you take and your allergies. If you don’t currently take a blood thinner and you aren’t allergic to aspirin, the dispatcher may advise you to chew an aspirin while you’re waiting on medical attention. If you have nitroglycerin tablets, you may also wish to use these as directed by your doctor to reduce chest pain.
If you have a list of medications you currently take or any information about your medical history, you may wish to take this information with you. It can speed your medical care.
At the hospital
When you arrive at the hospital, you can expect the emergency medical personnel to take an electrocardiogram (EKG). This is a pain-free way to measure your heart’s electrical activity.
If you’re having a heart attack, an EKG is performed to look for unusual electrical patterns in your heart. The EKG can help your doctor determine if the heart muscle is damaged and what part of your heart was damaged. A doctor will also likely order a blood draw. If you’re having a heart attack, your body usually releases certain proteins and enzymes as a result of the stress to your heart.
If you’re having a heart attack, your doctor will discuss treatment options with you. Your risk of severe heart damage is lowered if you start treatment within several hours of developing symptoms.
How to prevent future heart problems
According to the Centers for Disease Control and PreventionTrusted Source, an estimated 200,000 deaths from heart disease and stroke are preventable. Even if you have risk factors for heart disease or have already had a heart attack, there are things you can do to reduce your risk of having a heart attack in the future.
People who have already had a heart attack should make sure to take all medications prescribed to them by their doctor. If your doctor placed cardiac stents to keep your heart vessels open or you had to have bypass surgery for your heart, taking the medications your doctor prescribed to you is vital to preventing a future heart attack.
Sometimes if you require surgery for another condition, your doctor may recommend stopping some medications you take for your heart. An example might be an antiplatelet (anticlot) medication like clopidogrel (Plavix), prasugrel (Effient), or ticagrelor (Brilinta). Always check with the doctor you see for your heart before you stop taking any of your medications. It’s unsafe to abruptly stop many medications, and stopping abruptly could increase your risk of a heart attack.
References
Comments are closed.