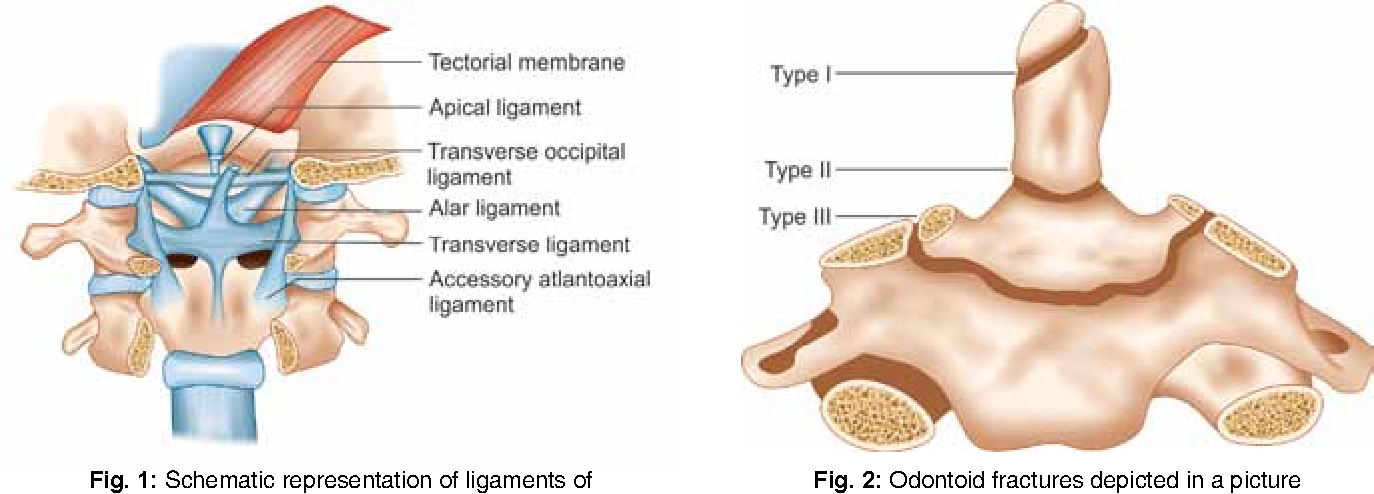
Treatment of Odontoid Fracture/Odontoid Fracture, the odontoid process, or dens, is a superior projecting bony element from the second cervical vertebrae (C2, or the axis). The first cervical vertebrae (atlas) rotates around the odontoid process to provide the largest single component of lateral rotation of the cervical spine. Fracture of the odontoid process is classified into one of three types, which are type I, type II, or type III fractures, depending on the location and morphology of the fracture.[rx]
The odontoid fracture can also occur with hyperflexion of the cervical spine. The transverse ligament runs dorsal to (behind) the odontoid process and attaches to the lateral mass of C1 on either side. If the cervical spine is excessively flexed, then the transverse ligament can transmit the excessive anterior forces to the odontoid process and cause an odontoid fracture.[rx]
A hangman’s fracture is better described as bilateral fracture traversing the pars inter articularis of C2 with an associated traumatic subluxation of C2 on C3. It is the second most common fracture of the C2 vertebrae following a fracture of the odontoid process and is almost always stable without the need for surgical intervention. Steele’s rule of thirds states that the cross-sectional area at the level of the atlas may be divided into three equally represented parts: the dens, space, and the spinal cord. This increased area for the spinal cord at this level is what allows for the relative lack of neurologic injury associated with a hangman’s fracture. [rx]

Mechanisms of Odontoid Fracture
Apart from hangings, the mechanism of injury—a sudden forceful hyperextension centered just under the chin—occurs mainly with deceleration injuries in which the victim’s face or chin strike an unyielding object with the neck in extension. The most common scenario is a frontal motor vehicle accident with an unrestrained passenger or driver, with the person striking the dashboard or windshield with their face or chin. Other scenarios include falls, diving injuries, and collisions between players in contact sports.
Although a hangman’s fracture is unstable, survival from this fracture is relatively common, as the fracture itself tends to expand the spinal canal at the C2 level. It is not unusual for patients to walk in for treatment and have such a fracture discovered on X-rays. Only if the force of the injury is severe enough that the vertebral body of C2 is severely subluxated from C3 does the spinal cord become crushed, usually between the vertebral body of C3 and the posterior elements of C1 and C2.

Types of Odontoid Fracture
Type I Odontoid Fracture
A type I odontoid fracture occurs when the rostral tip of the odontoid process is avulsed (broken or torn off). This injury commonly occurs due to pulling forces from the apical ligament attachment to the odontoid process. The apical ligament attaches the tip of the odontoid process to the foramen magnum (skull base).
Type II Odontoid Fracture
A type II odontoid fracture is a fracture through the base of the odontoid process. This injury occurs most typically when there is an excessive extension of the cervical spine, and the anterior arch of C1 pushes dorsally (backward) with sufficient force on the odontoid process (dens) to fracture the odontoid process at its base. Type II odontoid fractures can also occur with hyperflexion of the neck and the transverse ligament, pushing the odontoid process forward to the point of fracture.
Type III Odontoid Fracture
A type III odontoid fracture is a fracture through the body of the C2 vertebrae and may involve a variable portion of the C1 and C2 facets. Type III odontoid fractures occur secondary to hyperextension or hyperflexion of the cervical spine in a similar manner to type II odontoid fractures. The difference is where the fracture line occurs.
C2 fractures can be divided into 2 kinds: Odontoid and Hangmen
Odontoid Fractures
Location
-
Fracture through the dens, flexion or extension injury
Nomenclature
Anderson and D’Alonzo classification is the most ubiquitous.
-
Type-1 fractures: Upper portion of the odontoid peg, above the transverse portion of the cruciform ligament, these are generally stable
-
Type-2 fractures: These are the most common, the fracture through the based of the odontoid below the transverse portion of the cruciform ligament, they have a high risk of non-union
-
Type-3 fractures: These fracture through the odontoid peg and into the body of C2, generally well tolerated
The Roy-Camille classification of odontoid fractures is another but less frequently used nomenclature format focusing on the direction of the fracture line.
Hangman’s Fractures
Location
-
Fracture through the bilateral pars, generally from hyperextension and axial loading generally
-
Stable 90% heal with immobilization alone
Nomenclature
Levine and Edwards Classification
-
Type 1: Less than 3 mm subluxation of C2 on C3, due to axial loading, stable, rigid cervical collar treatment
-
Type 2: disruption of the C2 to C3 disc, posterior longitudinal ligament, greater than 4 mm subluxation, greater than 11 degrees angulation, less than 5 mm requires a reduction in axial traction and halo fixation for 6 to 12 weeks while those greater than 5 mms can require surgery
-
Type 2a: Less displacement more angular deformity, flexion injury, unstable, not suitable for axial traction, treatment in halo
-
Type 3: C2 to C3 facet capsule disrupted, anterior longitudinal ligament disruption, unstable, may have deficit, surgical candidates.
Levine and Edwards Classification[rx]
Specifics
- Angulation in this system is measured as the angle between the inferior endplate of C2 and C3. Anterior subluxation of C2 on C3 greater than 3 mm serves as a marker for C2 to C3 intervertebral disc disruption. It is important to recognize that this grading system is not applicaple in the pediatric population.
Grading
-
Type 1: Less than 3 mm subluxation of C2 on C3, due to axial loading, stable, rigid cervical collar treatment
-
Type 2: Disruption of the C2 to C3 disc, posterior longitudinal ligament, greater than 4 mm subluxation, greater than 11 degrees angulation, less than 5 mm requires a reduction in axial traction and halo fixation for 6 to 12 weeks while those greater than 5 mm can require surgery
-
Type 2a: Less displacement more angular deformity, flexion injury, unstable, not suitable for axial traction, treatment in halo
-
Type 3: C2 to C3 facet capsule disrupted, anterior longitudinal ligament disruption, unstable, may have deficit, surgical candidates
Francis Grading System[rx]
Specifics
- Two factors are taken into consideration for the Francis Grading system: angulation and displacement. Angulation is measured by the degree of anterior angulation off of the posterior vertebral line drawn straight up from the C3 vertebral body. Displacement is measured by the amount of anterolisthesis, either greater than or less than 3.5 mm.
Grading
-
Type 1: Less than 11 degrees of angulation and less than 3.5 mm of displacement
-
Type 2: Greater than 11 degrees of angulation and less than 3.5 mm of displacement
-
Type 3: Less than 11 degrees of angulation and greater than 3.5 mm displacement
-
Type 4: Greater than 11 degrees of angulation and greater than 3.5 mm of displacement
-
Type 5: Complete disc disruption
Typical versus Atypical Fractures
- It is important to recognize that not all C2, hangman’s type fractures can be described using these classification systems. A typical hangman’s fracture allows for separation of the anterior elements from the posterior elements of the C2 vertebrae, therefore increase the available space for the spinal cord.
- However, in the case of an atypical hangman’s fracture the posterior aspect of the C2 vertebral body, not the bilateral pars, is involved. This leads to a higher risk of neurologic injury as the space remaining for the spinal cord does not increase secondary to the fracture.

Causes of Odontoid Fracture
- Odontoid fractures occur as a result of trauma to the cervical spine.
- high-energy trauma, which occurs as a result of a motor vehicle or diving accidents.
- trauma can occur after lower energy impacts such as falls from a standing position.
- hyperextension of the cervical spine, pushing the head and C1 vertebrae backward.
- forceful thrust are high enough (or the patient’s bone density is compromised secondary to osteopenia/osteoporosis),
- The odontoid fracture can also occur with hyperflexion of the cervical spine.
- The transverse ligament runs dorsal to (behind) the odontoid process and attaches to the lateral mass of C1 on either side.
- If the cervical spine is excessively flexed, then the transverse ligament can transmit the excessive anterior forces to the odontoid process and cause an odontoid fracture.[rx]
- Sudden forceful fall down
- Road traffic accident
- Falls – Falling onto an outstretched hand is one of the most common causes of the broken cervical spine.
- Sports injuries – Many cervical spine fractures occur during contact sports or sports in which you might fall onto an outstretched hand — such as in-line skating or snowboarding.
- Motor vehicle crashes – Motor vehicle crashes can cause cervical spine to break, sometimes into many pieces, and often require surgical repair.
- Have osteoporosis – a disease that weakens your bones
- Eave low muscle mass or poor muscle strength – or lack agility and have poor balance (these conditions make you more likely to fall)
- Walk or do other activities in the snow or on the ice – or do activities that require a lot of forwarding momenta, such as in-line skating and skiing.
- Previous pelvic fractures record.
- Wave an inadequate intake of calcium or vitamin D.
- Football or soccer, especially on artificial turf
- Athletic injury with a sports injury.
- Horseback riding
- Hockey
- Skiing
- Snowboarding
- Clumsiness in hands
- Gait imbalance
- Degenerative cervical spondylosis (CSM)
- Compression usually caused by anterior degenerative changes (osteophytes, disc osteophyte complex)
- Degenerative spondylolisthesis and hypertrophy of ligamentum flavum may contribute
- The most common cause of cervical myelopathy.
Symptoms of Odontoid Fracture
Symptoms of cervical spondylosis include:
- Neck stiffness and pain
- Numbness and weakness in the upper limbs
- Difficulty in walking, losing balance, or weakness in limbs
- Difficulty in turning the head fully or bending the neck, which may hinder drive
- Muscle spasms in neck and shoulders
- Headaches
- Grinding and popping feeling in the neck when rotating the head
- Loss of bladder and bowel control.
- neck pain and stiffness
- axial neck pain (oftentimes absent)
- occipital headache common
- extremity paresthesias
- diffuse nondermatomal numbness and tingling
- weakness and clumsiness
- weakness and decreased manual dexterity (dropping object, difficulty manipulating fine objects)
- Gait instability patient feels “unstable” on feet
- weakness walking up and downstairs
- gait changes are the most important clinical predictor
- urinary retention rare and only appear late in disease progression, not very useful in diagnosis due to the high prevalence of urinary conditions in this patient population
- Cervical pain aggravated by movement
- Referred pain (occiput, between the shoulder blades, upper limbs)
- Retro-orbital or temporal pain (from C1 to C2)
- Cervical stiffness—reversible or irreversible
- Vague numbness, tingling, or weakness in upper limbs
- Dizziness or vertigo
- Poor balance
- Rarely, syncope triggers a migraine, “pseudo-angina”
Diagnosis of Odontoid Fracture
Laboratory tests should be ordered as an adjunct in overall medical status.
- Normalized hemoglobin,
- hematocrit,
- coagulation profile with prothrombin time (PT),
- partial thromboplastin time (PTT), and
- platelet counts will be needed for operative intervention.
In hospitals and countries without readily available advanced imaging capabilities, radiographs are critical to evaluate and assist in ruling out potential odontoid fractures. Recommended views include:[rx]
-
AP C-spine
-
Lateral C-spine
-
Open-mouth odontoid view
Although radiographs yield lower sensitivity and specificity rates when compared to computed tomogram (CT) scans, experienced clinicians and practitioners can still appreciate suspected injury without CT utilization. In addition, in the setting of suspected occipito cervical instability (useful in type I odontoid fractures or the setting of os odontoideum), flexion-extension radiographs should be obtained.
X-ray
Evaluation of x-rays will provide limited but important information. Care must be taken to ensure proper radiographic imaging creates a picture from the occiput to the C7 through T1 disc space. This is essential in reviewing cervical spine trauma. Lateral, anteroposterior (AP) and open mouth odontoid views are necessary. Approximately, 93% of cervical spine injuries are apparent with combined, lateral, AP, and odontoid view radiographs. X-rays are an excellent modality for determining alignment during the immediate injury, post-operative period, as well as long-term, follow up.
Computed tomogram (CT) scan
CT scan is the most important modality for determining fracture etiology and ruling out an injury with regards to a C2 fracture. Even if plain films are negative and clinical suspicion is high a CT scan is warranted. CT scan does not directly evaluate the spinal cord, soft tissue, or ligamentous construct. It is important to recognize the importance that complete imaging will require dedicated thin-cut CT reconstructions. Non-contrast CT scan is adequate for evaluation of the bony anatomy for fracture. This can be coupled with a CT angiogram for evaluation of the vascular anatomy.
Magnetic resonance imaging (MRI) scan
Evaluation with MRI is important for the analysis of the ligamentous construct, disc space, spinal cord, nerve roots, and other soft tissue injuries. MRI is also useful for determining the acute nature of the fracture when this is otherwise unknown. This is done via non-contrasted imaging. T2 signal hyperintensities and STIR changes within the dens, ligaments, or soft tissue can illustrate an acute component.
Vascular Imaging
Vascular imaging may be indicated. The vertebral artery’s second segment (V2) runs through the transverse foramen of C2 to C6 while V3 runs extramurally exiting the C2 foramen across the sulcus arteriosus. This can place it at risk for injury. Indeed, in one series 15% of patients with C1 to C2 fractures had a vertebral artery injury. Of which, type-III odontoid fractures posed the greatest risk. It is important to note that an untreated vertebral artery injury has a 24% stroke rate.
Advanced Imaging modalities
The imaging modality of choice is a CT of the cervical spine. The CT provides the best resolution of the bony elements allowing for identification and characterization of an odontoid fracture. If there is neurologic injury (paresthesia, weakness), then magnetic resonance imaging (MRI) without the contrast of the cervical spine should be obtained to assess the cervical cord for injuries.
Nuclear bone scan – a diagnostic procedure in which a radioactive substance is injected into the body to measure activity in the bones. (The amount of radiation is small–less than the radiation in half of one CT scan.) This scan helps identify damaged bones.

Treatment of Odontoid Fracture
The treatment of an odontoid fracture depends on the type of fracture and age of the patient.[rx][rx][rx][rx]
Non-Surgical Treatment
Treatment available can be broadly
- Skeletal traction – Available evidence suggests that treatment depends on the part of the pelvic fracture that is fractured. Traction may be useful for odontoid fracture because it counteracts the force of the muscle pulling the two separated parts together, and thus may decrease bleeding and pain.[rx] Traction should not be used in the femoral neck and odontoid fracture or when there is any other trauma to the leg or pelvis.[rx][rx] It is typically only a temporary measure used before surgery. It only considered the definitive treatment for patients with significant comorbidities that contraindicate surgical management.[rx]
- Get medical help immediately – If you fall on an outstretched arm, get into a car accident or are hit while playing a sport and feel intense pain in your hip area, then get medical care immediately. You’ll innately know that something is seriously wrong because you won’t be able to lift your leg up. Other symptoms include immediate swelling and/or bruising near the fracture, grinding sounds with arm movements and potential numbness, and tingling in the leg.
- Apply ice – After you get home from the hospital odontoid fracture (regardless if you had surgery or not), you should apply a bag of crushed ice (or something cold) to your injured in order to reduce the swelling and numb the pain. Ice therapy is effective for acute (recent) injuries that involve swelling because it reduces blood flow by constricting local blood vessels. Apply the crushed ice to your odontoid fracture for 15 minutes three to five times daily until the soreness and inflammation eventually fades away
- Lightly exercise after the pain fades – After a couple of weeks when the swelling has subsided and the pain has faded away, remove your arm sling for short periods and carefully move your hip joints in all different directions. Don’t aggravate the odontoid fracture so that it hurts, but gently reintroduce movements to the involved joints and muscles. Start cautiously, maybe starting with light, and then progress to holding light weights (five-pound weights to start).
- Practice stretching and strengthening exercises – of the fingers, leg if your doctor recommends them.
- A splint – which you might use for a few days to a week while the swelling goes down; if a splint is used initially, a cast is usually put on about a week later.
- A cast – which you might need for six to eight weeks or longer, depending on how bad the break is (you might need a second cast if the first one gets too loose after the swelling goes away.)
- Get a supportive arm sling – Due to their anatomical position, necks of odontoid fracture can’t be cast like a broken spine. Instead, a supportive arm sling or “figure-eight” splint is typically used for support and comfort, either immediately after the injury if it’s just a hairline fracture or following surgery, if it’s a complicated fracture.
- Get a referral to physical therapy – Once you’ve recovered and able to remove your arm sling splint for good, you’ll likely notice that the muscles surrounding your neck and lower chest look smaller and feel weaker. That’s because muscle tissue atrophies without movement. If this occurs, then you’ll need to get a referral for some physical rehabilitation. Rehab can start once you are cleared by your orthopedist, are pain-free, and can perform all the basic arm and necks movements. A physiotherapist or athletic trainer can show you specific rehabilitation exercises and stretches to restore your muscle strength, joint movements, and flexibility
- Rigid fixation – osteosynthesis with locking plate, hook plate fixation, fixation with a locking plate, coracoclavicular screws, Knowles pin fixation.
- Flexible fixation – simple k wire fixation, tension band wiring, suture anchors, vinyl tape, dacron arterial graft for ligament reconstruction.
- A splint – which you might use for a few days to a week while the swelling goes down; if a splint is used initially, a cast is usually put on about a week later.
- A cast – which you might need for six to eight weeks or longer, depending on how bad the break is (you might need a second cast if the first one gets too loose after the swelling goes away.)
Rest Your Leg – Once you’re discharged from the hospital in an arm sling, your top priority is to rest your and not further inflame the injury. Of course, the arm sling not only provides support, but it also restricts movement, which is why you should keep it on even during sleep. Avoiding the temptation to move your shoulder and arm will help the bone mend quicker and the pain fades away sooner.
- Depending on what you do for a living and if the injury is to your dominant side, you may need to take a couple of weeks off work to recuperate.
- Healing takes between four to six weeks in younger people and up to 12 weeks in the elderly, but it depends on the severity of the radial head fractures.
- Athletes in good health are typically able to resume their sporting activities within two months of breaking they’re ulnar styloid depending on the severity of the break and the specific sport.
- Sleeping on your back (with the sling on) is necessary to keep the pressure off your shoulder and prevent stressing the hip injury.
Eat Nutritiously During Your Recovery – All bones and tissues in the body need certain nutrients in order to heal properly and in a timely manner. Eating a nutritious and balanced diet that includes lots of minerals and vitamins are proven to help heal broken bones of all types. Therefore focus on eating lots of fresh produce (fruits and veggies), whole grains, lean meats, and fish to give your body the building blocks needed to properly repair your. In addition, drink plenty of purified water, milk, and other dairy-based beverages to augment what you eat.
- Broken bones need ample minerals (calcium, phosphorus, magnesium, boron) and protein to become strong and healthy again.
- Excellent sources of minerals/protein include dairy products, tofu, beans, broccoli, nuts and seeds, sardines, and salmon.
- Important vitamins that are needed for bone healing include vitamin C (needed to make collagen), vitamin D (crucial for mineral absorption), and vitamin K (binds calcium to bones and triggers collagen formation).
- Conversely, don’t consume food or drink that is known to impair bone/tissue healing, such as alcoholic beverages, sodas, most fast food items and foods made with lots of refined sugars and preservatives.
Physical Therapy
- Although there will be some pain, it is important to maintain arm motion to prevent stiffness. Often, patients will begin doing exercises for elbow motion immediately after the injury. It is common to lose some leg strength. Once the bone begins to heal, your pain will decrease and your doctor may start gentle hip, knee exercises. These exercises will help prevent stiffness and weakness. More strenuous exercises will be started gradually once the fracture is completely healed.
Follow-Up Care
- You will need to see your doctor regularly until your fracture heals. During these visits, he or they will take x-rays to make sure the bone is healing in a good position. After the bone has healed, you will be able to gradually return to your normal activities.
Breathing Exercise
- To elevate breathing problems or remove lung congestion if needed.
Type I Odontoid Fracture
- Most consider a type I odontoid fracture a stable fracture and treatment for six to 12 weeks in a rigid cervical orthosis (hard cervical collar). Some have suggested that rarely a type I odontoid fracture may be unstable secondary to more extensive and unrecognized ligamentous injury, and flexion/extension x-rays should be obtained at the time of removal of the cervical collar after six to 12 weeks to ensure cervical stability.
Type II Odontoid Fracture[rx]
- Type II odontoid fractures are inherently unstable and have a lower union rate than type III odontoid fractures due to the lower surface area of a fractured bone in type II versus type III odontoid fractures.
- The configuration of type II odontoid fracture and age of patient also play important roles in treatment decisions. The current treatment options for a type II odontoid fracture include rigid cervical orthosis, halo vest immobilization, odontoid screw, transoral adenoidectomy, and posterior instrumentation.
Rigid Cervical Orthosis
- A type II odontoid fracture is inherently unstable, and a rigid cervical orthosis is not the ideal treatment for such an injury. In the elderly population, many are not surgical candidates (due to comorbidities or poor bone quality), and the elderly typically poorly tolerate a halo vest immobilization. In such situations, a practitioner may attempt a rigid cervical orthosis, although union rates are low.
Halo Vest Immobilization
- If a patient is relatively young and healthy, and there is low risk for nonunion, then halo vest immobilization may be the best treatment for a type II odontoid fracture. Risk factors for nonunion include a fractured space greater than a few millimeters between the odontoid process and vertebral body, poor alignment of the odontoid process with respect to the vertebral body, and poor bone quality and/or health status of the patient.
Medication
- Antibiotic – Cefuroxime or Azithromycin, or Flucloxacillin or any others cephalosporin/quinolone antibiotic must be used to prevent infection or clotted blood remove to prevent furthers swelling and edema
- NSAIDs – Prescription-strength drugs that reduce both pain and inflammation. Pain medicines and anti-inflammatory drugs help to relieve pain and stiffness, allowing for increased mobility and exercise. There are many common over-the-counter medicines called non-steroidal anti-inflammatory drugs (NSAIDs). They include and Ketorolac, Aceclofenac, Naproxen, Etoricoxib.
- Corticosteroids – Also known as oral steroids, these medications reduce inflammation.
- Muscle Relaxants – These medications provide relief from associated muscle spasms.
- Neuropathic Agents – Drugs(pregabalin & gabapentin) that address neuropathic—or nerve-related—pain. This includes burning, numbness, and tingling.
- Opioids – Also known as narcotics, these medications are intense pain relievers that should only be used under a doctor’s careful supervision.
- Topical Medications – These prescription-strength creams, gels, ointments, patches, and sprays help relieve pain and inflammation through the skin.
- Calcium & vitamin D3 – to improve bone health and healing fracture. As a general rule, men and women age 50 and older should consume 1,200 milligrams of calcium a day, and 600 international units of vitamin D a day.
- Glucosamine & Diacerein, Chondroitin sulfate – can be used to tightening the loose tension, cartilage, ligament, and cartilage, ligament regenerate cartilage or inhabit the further degeneration of cartilage, ligament
- Dietary supplement-to remove general weakness & improved health.
- Antidepressants – A drug that blocks pain messages from your brain and boosts the effects of endorphins (your body’s natural painkillers).
Odontoid Screw
- An anterior odontoid osteosynthesis (odontoid screw) is a screw placed from the inferior anterior aspect of the C2 vertebral body, in a superior trajectory, and capturing the odontoid process and affixing it in place to allow bony fusion to occur. The odontoid screw has an advantage of relative preservation of motion of the upper cervical spine while treating a type II odontoid fracture.
- A surgeon can only place the odontoid screw if there are acceptable alignment and minimal displacement of the odontoid process, the fracture line is oblique or perpendicular to the screw trajectory, the injury is relatively recent, and the patient has acceptable body habitus to place the odontoid screw.
Transoral Odontoidectomy
- In some situations, the odontoid process (dens) may be severely posteriorly displaced and compressing the spinal cord causing neurologic deficits. It is difficult and dangerous to reduce the odontoid process in a closed manner, so surgical removal of the odontoid process is required to relieve the compression of the spinal cord.
- This relief is commonly achieved through a transoral adenoidectomy, as the odontoid process commonly is located posterior to the oropharynx. If the odontoid process is removed, the cervical spine remains unstable, and the patient requires instrumented fusion, commonly from a posterior or combined anterior-posterior approach.
Posterior Instrumentation
If the patient has certain risk factors for nonunion, then posterior instrumentation may provide the best treatment option for a type II odontoid fracture. The risk factors include:
-
More than a few millimeters gap between the odontoid process and the vertebral body
-
Poor odontoid process alignment
-
Poor bone quality, older fractures
-
Older patients
-
Failure of other treatment modalities
-
Smoking
Posterior instrumented fusion techniques vary widely and include fusion limited to C1 and C2 as well as more extensive fusions. The fusion of only C1 and C2 will lead to approximately 50% reduction of the lateral rotation of the cervical spine.
Surgical Treatment
Treatment options include conservative management, cervical orthosis, halo-vest orthosis, and surgical procedures.[rx][rx][rx][rx]
External Fixation
- Rigid cervical collar represents the immediate first treatment. For type-I and type-III odontoid fractures this is generally adequate. This is also true for 90% of Hangman’s fractures. Halo-vest orthosis can be used as well for external fixation in certain cases of type-II odontoid fractures or angulated/displaced Hangman’s fractures but is not very well tolerated in the elderly population.
Internal Fixation
- Internal fixation can be achieved via anterior fixation or by a variety of posterior constructs.
Anterior
- An odontoid screw can be placed for type-II odontoid fractures in good alignment with an intact transverse ligament in the acute setting. There is concern about the placement of the odontoid screw in the elderly population and instances of delayed non-union.
Posterior
-
C1 to C2 transarticular screws
-
C1 lateral mass and C2 pedicle screws
-
C1 lateral mass and C2 pars interarticularis screws
-
C1 to C2 wiring (also as an adjunct technique)
Posterior fixation technique selection requires significant review by neurosurgeon or orthopedic spine surgeon. It takes into consideration a variety of factors including surgeon experience, fracture location, vertebral artery location, biomechanical suitability, and anatomical variations. Vascular imaging is mandatory to illustrate the location of the vertebral artery in the V2 and V3 segments.
Collars and Halo Fixators
- The use of collars and halo fixators remains controversial. Soft collars have no stabilizing function, thus we do not recommend them in the early phase. However, they may be used for nonoperative treatment in stable fractures after an initial phase with a hard collar.
- Hard collars (Philadelphia, for example) may be used in the first phase for unstable fractures until a decision for further treatment is made. It may be used for 6 to 8 weeks in cases where nonoperative treatment is indicated. [rx–rx]
Anterior Odontoid Screw Fixation
- Initially described by Böhler,rx] osteosyntheses with 1 or 2 screws by an anterior approach is a standard operative treatment in younger patients with good bone quality if adverse modifiers are absent.
- Patients are operated on in the supine position. With a minimal open incision, the preparation follows the anatomical structures for the standard anterior approach to the cervical spine.
Anterior Transarticular C1/2 Stabilization
- This technique may be used in elderly patients to secure reduction by transarticular stabilization of C1/2 if the posterior approach is impossible and is regularly combined with odontoid screw(s).[rx]
- A crucial part of this operative technique is the entry point and positioning of the screws from C2 onto C1 via the classical anterior approach. As in the posterior technique, the vertebral artery anatomy has to be analyzed in advance.
Posterior Transarticular C1/2 Stabilization and Fusion
- The posterior fusion technique with bone graft is performed by an open approach. This technique may be modified into a percutaneous cannulated posterior C1/2 stabilization.
- The crucial step is the reduction of the fracture and the positioning of the patient to maintain correct reduction. Care must be taken not to harm the vertebral artery as there is a large variety and the anatomical space for the screws is absolutely limited.[rx,rx]
Posterior Instrumentation (Harms/Goel)
- C1/2 internal fixation by placing C1 lateral mass screws and C2 pedicle screws according to Harms/Goel is a valuable alternative to the Magerl technique. This technique was first described by Goel and allows good fracture reduction.
- It is the preferred method in cases where the Magerl technique is not possible and if one aims for a temporary stabilization. However, it is demanding, with the need for an open approach in an anatomically complex region. The technique has been modified by Harms and Melcher[rx] using polyaxial screw/rod systems.
Posterior Occipito-Cervical Stabilization and Fusion (C0-C3/4)
- The presence of ankylosing spondylitis, diffuse idiopathic skeletal hyperostosis (DISH), or complex injuries may alter the treatment algorithm and a C1/2 stabilization alone may be insufficient. In these cases, an occipital-cervical stabilization and fusion should be performed.
References

![]()





About the author