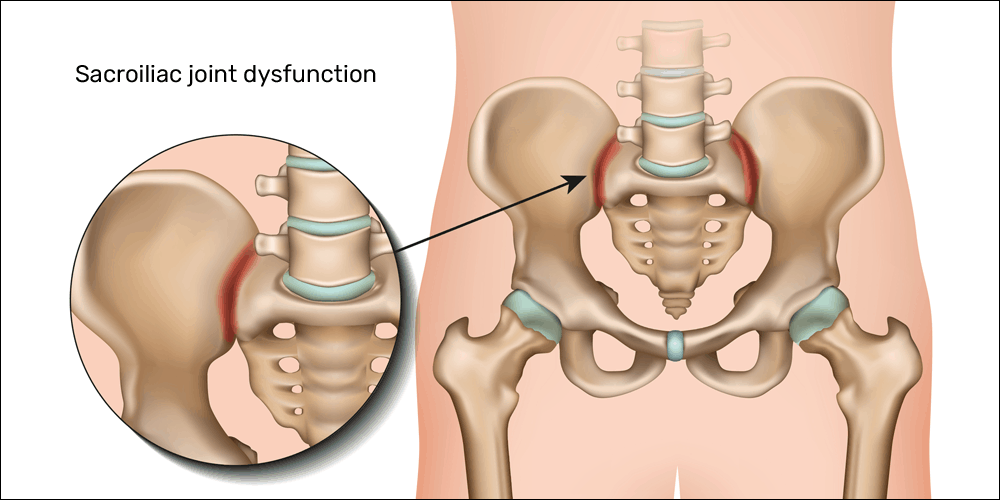
Sacroiliac Joint Dislocation/Sacroiliac Joint Dysfunction or sacroiliitis are common terms used to describe the pain of the sacroiliac joint. It is usually caused by abnormal motion (i.e. hyper- or hypo-mobile) or malalignment of the sacroiliac joint. The joint can be hyper or hypo-mobile which can cause pain. Pain is usually localized over the buttock. Patients usually describe the pain as sharp, dull, achy, stabbing, or shooting pain directly over the affected joint.
Sacroiliac joint (SIJ) pain refers to the pain arising from the SIJ joint structures. SIJ dysfunction generally refers to an aberrant position or movement of SIJ structures that may or may not result in pain. This paper aims to clarify the difference between these clinical concepts and present currently available evidence regarding the diagnosis and treatment of SIJ disorders.
Sacroiliitis is inflammation within the sacroiliac joint. It is a feature of spondyloarthropathies, such as axial spondyloarthritis (including ankylosing spondylitis), psoriatic arthritis, reactive arthritis or arthritis related to inflammatory bowel diseases, including ulcerative colitis or Crohn’s disease. It is also the most common presentation of arthritis from brucellosis.
Anatomy of Sacroiliac Joint Dislocation
Six variants of the sacroiliac joints have been observed: accessory joints, iliosacral complex, bipartite iliac bony plate, crescent-like iliac bony plate, semicircular defects at the sacral or iliac side and ossification centers.
- Accessory sacroiliac joint – Accessory sacroiliac joint is found medial to the posterior superior iliac spine and lateral to the second sacral foramen amongst a rudimentary transverse tuberosity. On CT imaging, accessory joints have articular surfaces that resemble osseous projects from the ilium to the sacrum. An accessory joint can be present at birth; however, they more commonly result from the stress of weight-bearing. Accessory joints are more commonly present in the obese population and the older population, as well as a higher prevalence in women with 3 or more childbirths, compared to 2 or less.
- Iliosacral complex – Iliosacral complex forms from a projection from the ilium articulating with a complementary sacral recess. These complexes can be unilateral or bilateral, and like accessory joints, these complexes exist at the posterior sacroiliac joint from the level of first to the second sacral foramen. This variant has been seen more in older patients greater than 60 years, as well as obese women more so than normal-weight women.
- Bipartite iliac bony plate – Bipartite iliac bony plate is located at the posterior portion of the sacroiliac joint and appears as described, consisting of two parts and appears unilaterally.
- Semicircular defects on the iliac/sacral side – The fourth variant is semicircular defects on either the sacral or iliac aspects of the articular surface of the sacroiliac joint. These can be unilateral or bilateral and again are present at the posterior portion of the sacroiliac joint from the level of the first to the second sacral foramen. This defect has been observed more in women than men and in patients older than 60 years.
- Crescent-like iliac bony plate – The fifth variant is a crescent-like articular surface which may be present unilaterally or bilaterally. CT imaging demonstrates a crescent-like iliac plate with accompanying a bulged sacral surface. This defect is found usually at the posterior portion of the sacral iliac joint spanning the levels of the first and second sacral foramen. This defect was observed only in women and more commonly in patients greater than 60 years old.
- Ossification centers of the sacral wings – The sixth anatomical variant observed is ossification centers presenting as triangular osseous bodies located within the joint space at the anterior portion of the sacroiliac joint. This defect is found at the level of the first sacral foramen, typically unilaterally.[rx][rx]
Causes of Sacroiliac Joint Dislocation
-
High energy trauma (e.g. MVA, falls) – can lead to pelvic ring injuries with a spectrum of injury to the SI joint ligaments
-
Ligament strain and/or stress or occult fractures
-
- Degenerative arthritis
- Degenerative conditions of the spine (most common causes)
-
Spondylolisthesis: in the degenerative setting, this occurs as a result of a pathologic cascade including intervertebral disc degeneration, ensuing intersegmental instability, and facet joint arthropathy
- Spinal stenosis
- Adult isthmic spondylolisthesis is typically caused by an acquired defect in the par interarticularis
-
Pars defects (i.e. spondylolisis) in adults are most often secondary to repetitive microtrauma
-
-
-
Trauma (e.g. burst fractures with bony fragment retropulsion)
-
Clinicians should recognize spinal fractures can occur in younger, healthy patient populations secondary to high-energy injuries (e.g. MVA, fall from height) or secondary low energy injuries and spontaneous fractures in the elderly populations, including any patient with osteoporosis
-
Associated hemorrhage from the injury can result in a deteriorating clinical and neurologic exam
-
-
Benign or malignant tumors
-
Metastatic tumors (most common)
-
Primary tumors
-
Ependymoma
-
Schwannoma
-
Neurofibroma
-
Lymphoma
-
Lipomas
-
Paraganglioma
-
Ganglioneuroma
-
Osteoblastoma
-
-
Infection
-
Osteodiscitis
-
Osteomyelitis
-
Epidural abscess
-
Fungal infections (e.g. Tuberculosis)
-
Other infections: lyme disease, HIV/AIDS-defining ilnesses, Herpes zoster (HZ)
- rare cause of SI joint pain
-
-
Vascular conditions
-
Hemangioblastoma, aterior-venous malformations (AVM)[rx]
-
-
Inflammatory arthropathy (i.e. sacroiliitis)
-
Spondyloarthropathies such as Ankylosing spondylitis, reactive arthritis, psoriatic arthritis, and inflammatory bowel disease (Crohn disease and Ulcerative colitis) should be considered with sacroiliac joint pain especially those with systemic manifestations
-
- Moderate impact exercise (e.g. lifting, jogging)
- Secondary conditions
-
secondary to previous spinal fusion procedures
-
secondary to scoliosis and/or leg length discrepancy
-
- Any form of spondyloarthropathies – which includes ankylosing spondylitis, psoriatic arthritis, reactive arthritis or arthritis related to inflammatory bowel diseases, including ulcerative colitis or Crohn’s disease.
- Pregnancy – can cause inflammation as a result of the widening and stretching of the sacroiliac joints to prepare for childbirth. Additionally, the added weight carried during childbearing can put an extra amount of stress on the SI joints, leading to abnormal wear.

Symptoms of Sacroiliac Joint Dislocation
- Sciatic-like pain – in the buttocks and/or backs of the thighs that feels hot, sharp, and stabbing and may include numbness and tingling. Sciatic-like pain from sacroiliac joint dysfunction rarely extends below the knee.
- Stiffness – and reduced range-of-motion in the lower back, hips, pelvis, and groin, which may cause difficulty with movements such as walking up stairs or bending at the waist.
- Worsened pain – when putting added pressure on the sacroiliac joint, such as climbing stairs, running or jogging, and lying or putting weight on one side.
- Instability – in the pelvis and/or lower back, which may cause the pelvis to feel like it will buckle or give way when standing, walking, or moving from standing to sitting.
The following are signs and symptoms that may be associated with an SI joint (SIJ) problem
- Mechanical SIJ dysfunction usually causes a dull unilateral low back pain.[rx]
- The pain is often a mild to moderate ache around the dimple or posterior superior iliac spine (PSIS) region.[rx]
- The pain may become worse and sharp while doing activities such as standing up from a seated position or lifting the knee towards the chest during stair climbing.
- Pain is typically on one side or the other (unilateral PSIS pain), but the pain can occasionally be bilateral.
- When the pain of SIJ dysfunction is severe (which is infrequent), there can be referred pain into the hip, groin, and occasionally down the leg, but rarely does the pain radiate below the knee.
- Pain can be referred from the SIJ down into the buttock or back of the thigh, and rarely to the foot.
- Low back pain and stiffness, often unilateral, that often increases with prolonged sitting or prolonged walking.
- Pain may occur during sexual intercourse; however, this is not specific to just sacroiliac joint problems.
Symptoms are typically aggravated by
- Transitioning from sitting to standing
- Walking or standing for extended periods of time
- Running
- Climbing stairs
- Taking long strides
- Rolling over in bed
- Bearing more weight on one leg[rx]
Diagnosis of Sacroiliac Joint Dislocation
In most clinical evaluations, common laboratory findings in the aseptic setting include:
-
WBC count – usually normal (elevated in infection/septic presentation)
-
ESR – elevated
-
CRP – elevated
-
HLA-B27 – About 1-2% of patients with ankylosing spondylitis will be HLA-B27 positive
-
Rheumatoid Factor (RF) – Negative in the setting of true ankylosing spondylitis
Special provocative tests can be very helpful in reproducing the patient’s pain:
-
“Fortin finger sign”- reproduction of pain after applying a deep palpation with the four-hand fingers posteriorly at the patient’s SI joint(s).
-
FABER test– reproduction of pain after flexing the hip while also abducting and externally rotating the hip.
-
Sacral distraction test– reproduction of pain after applying pressure to the anterior superior iliac spine.
-
Iliac compression test– reproduction of pain after applying pressure downward on the superior aspect of the iliac crest.Apply compression to the joint with the patient lying on his or her side. The pressure is applied downward to the uppermost iliac crest.[rx]
-
Gaenslen test– reproduction of pain after having the patient flex the hip on the unaffected side and then dangle the affected leg off the examining table. The pressure is then directed downward on the leg to extend further the hip, which causes stress on the SI joint.
-
Sacral thrust test– reproduction of pain with the patient prone and then applying an anterior pressure through the sacrum.
- Iliac Gapping Test – Distraction can be performed to the anterior sacroiliac ligaments by applying pressure to the anterior superior iliac spine.[rx]
- Patrick test – To identify if the pain may come from the sacroiliac joint during flexion, abduction, and external rotation, the clinician externally rotates the hip while the patient lies supine. Then, downward pressure is applied to the medial knee stressing both the hip and sacroiliac joint.[rx][rx][rx]
- Thigh Thrust – This test applies anteroposterior shear stress on the SI joint. The patient lies supine with one hip flexed to 90 degrees. The examiner stands on the same side as the flexed leg. The examiner provides either a quick thrust or steadily increasing pressure through the line of the femur. The pelvis is stabilized at the sacrum or at the opposite ASIS with the hand of the examiner.
- Palpation tests – in which deep thumb pressure is applied directly over the entire SI joint on each side. A positive test is a tenderness over the affected SI joint, which should then be correlated with other provocative tests. When several types of motion palpation tests are included with clusters of provocative tests such as those described above, the highest level of accuracy was found.
Radiological Imaging
- X-rays – The first test typically performed and one that is very accessible at most clinics and outpatient offices. Three views (AP, lateral, and oblique) views help assess the overall alignment of the spine as well as for the presence of any degenerative or spondylotic changes.
- CT Scan – This imaging is the most sensitive test to examine the bony structures of the spine. It can also show calcified sacroiliac joint dysfunction or any insidious process that may result in bony loss or destruction. In patients that are unable to or are otherwise ineligible to undergo an MRI, CT myelography can be used as an alternative to visualize a herniated disc.
- MRI – The preferred imaging modality and the most sensitive study to visualize a herniated disc, as it has the most significant ability to demonstrate soft-tissue structures and the nerve as it exits the foramen and sacroiliac joint dysfunction
- Electrodiagnostic testing – (Electromyography and nerve conduction studies) can be an option in patients that demonstrate equivocal symptoms or imaging findings as well as to rule out the presence of a peripheral mononeuropathy. The sensitivity of detecting cervical radiculopathy with electrodiagnostic testing ranges from 50% to 71%.[rx]
- The contralateral (crossed) straight leg raise test – As in the straight leg raise test, the patient is lying supine, and the examiner elevates the asymptomatic leg. The test is positive if the maneuver reproduces the patient’s typical pain and paresthesia. The test has a specificity greater than 90%.
- Myelography – An X-ray of the spinal canal following the injection of contrast material into the surrounding cerebrospinal fluid spaces will reveal the displacement of the contrast material. It can show the presence of structures that can cause pressure on the spinal cord or nerves, such as herniated discs, tumors, or bone spurs.
- Transcranial Magnetic Stimulation (TMS) – The presence and severity of myelopathy can be evaluated by means of transcranial magnetic stimulation (TMS), a neurophysiological method that measures the time required for a neural impulse to cross the pyramidal tracts, starting from the cerebral cortex and ending at the anterior horn cells of the cervical, thoracic, or lumbar spinal cord and sacroiliac joint dysfunction. This measurement is called the central conduction time (CCT).
- Electromyography and nerve conduction studies (EMG/NCS) – measure the electrical impulses along with nerve roots, peripheral nerves, and muscle tissue. Tests can indicate if there is ongoing nerve damage, if the nerves are in a state of healing from a past injury, or if there is another site of nerve compression. EMG/NCS studies are typically used to pinpoint the sources of nerve dysfunction distal to the spine.
Evaluating clinicians must first rule out associated “red flag” symptoms including
-
Thoracic pain
-
Fever/unexplained weight loss
-
Night sweats
- Bowel or bladder dysfunction
- Malignancy (document/record any previous surgeries, chemo/radiation, recent scans and bloodwork, and history of metastatic disease)
-
Can be seen in association with pain at night, pain at rest, unexplained weight loss, or night sweats
-
-
Significant medical comorbidities
-
Neurologic deficit or serial exam deterioration
-
Gait ataxia
-
Saddle anesthesia
-
Age of onset (bimodal — Age < 20 years or Age > 55 years)

Treatment of Sacroiliac Joint Dislocation
-
Massages – Various massage techniques are used to relax muscles and ease tension.
-
Heating and cooling – This includes the use of hot packs and plasters, a hot bath, going to the sauna, or using an infrared lamp. Heat can also help relax tense muscles. Cold packs, like cold wraps or gel packs, are also used to help with irritated nerves.
-
Ultrasound therapy – Here the lower back is treated with sound waves. The small vibrations that are produced generate heat to relax body tissue.
-
Lumbar Manipulation – There is limited evidence suggesting that cervical manipulation may provide short-term benefits for neck pain. Complications from manipulation are rare and can include worsening radiculopathy, myelopathy, spinal cord injury, and vertebral artery injury. These complications occur ranging from 5 to 10 per 10 million manipulations.
-
Lumbar Corset or Collar for Immobilization – In patients with acute neck pain, a short course (approximately one week) of collar immobilization may be beneficial during the acute inflammatory period.
- Traction – May be beneficial in reducing the radicular symptoms associated with disc herniations. Theoretically, traction would widen the neuroforamen and relieve the stress placed on the affected nerve, which, in turn, would result in the improvement of symptoms. This therapy involves placing approximately 8 to 12 lbs of traction at an angle of approximately 24 degrees of neck flexion over a period of 15 to 20 minutes.
- Supports or braces – When the SI joint is too loose (hypermobile), a pelvic brace can be wrapped around the waist and pulled snugly to stabilize the area. A pelvic brace is about the size of a wide belt and can be helpful when the joint is inflamed and painful.
Physical Therapy
- Exercising in water – can be a great way to stay physically active when other forms of exercise are painful. Exercises that involve lots of twisting and bending may or may not benefit you. Your physical therapist will design an individualized exercise program to meet your specific needs.
- Weight-training exercises – though very important, need to be done with proper form to avoid stress to the back.
- Reduce pain and other symptoms – Your physical therapist will help you understand how to avoid or modify the activities that caused the injury, so healing can begin. Your physical therapist may use different types of treatments and technologies to control and reduce your pain and symptoms.
- Improve posture –If your physical therapist finds that poor posture has contributed to your SI joint, the therapist will teach you how to improve your posture so that pressure is reduced in the injured area, and healing can begin and progress as rapidly as possible.
- Improve motion – Your physical therapist will choose specific activities and treatments to help restore normal movement in any stiff joints/ sacroiliitis. These might begin with “passive” motions that the physical therapist performs for you to move your spine, and progress to “active” exercises and stretches that you do yourself. You can perform these motions at home and in your workplace to help hasten healing and pain relief.
- Improve flexibility – Your physical therapist will determine if any of the involved muscles are tight, start helping you to stretch them, and teach you how to stretch them at home.
- Improve strength – If your physical therapist finds any weak or injured muscles, your physical therapist will choose, and teach you, the correct exercises to steadily restore your strength and agility. For neck and back disc herniations, “core strengthening” is commonly used to restore the strength and coordination of muscles around your back, hips, abdomen, and pelvis.
- Improve endurance – Restoring muscular endurance is important after an injury. Your physical therapist will develop a program of activities to help you regain the endurance you had before the injury, and improve it.
- Learn a home program – Your physical therapist will teach you strengthening, stretching, and pain-reduction exercises to perform at home. These exercises will be specific for your needs; if you do them as prescribed by your physical therapist, you can speed your recovery.
Eat Nutritiously During Your Recovery
- All bones and tissues in the body need certain nutrients in order to heal properly and in a timely manner. Eating a nutritious and balanced diet that includes lots of minerals and vitamins are proven to help heal broken bones of all types. Therefore focus on eating lots of fresh produce (fruits and veggies), whole grains, lean meats, and fish to give your body the building blocks needed to properly repair your. In addition, drink plenty of purified water, milk, and other dairy-based beverages to augment what you eat.
- Broken bones need ample minerals (calcium, phosphorus, magnesium, boron) and protein to become strong and healthy again.
- Excellent sources of minerals/protein include dairy products, tofu, beans, broccoli, nuts and seeds, sardines, and salmon.
- Important vitamins that are needed for bone healing include vitamin C (needed to make collagen), vitamin D (crucial for mineral absorption), and vitamin K (binds calcium to bones and triggers collagen formation).
- Conversely, don’t consume food or drink that is known to impair bone/tissue healing, such as alcoholic beverages, sodas, most fast food items, and foods made with lots of refined sugars and preservatives.
Medication
Pharmacotherapy – There is no evidence to demonstrate the efficacy of non-steroidal anti-inflammatories (NSAIDs) in the treatment of SI radiculopathy. However, they are commonly used and can be beneficial for some patients. The use of COX-1 versus COX-2 inhibitors does not alter the analgesic effect, but there may be decreased gastrointestinal toxicity with the use of COX-2 inhibitors. Clinicians can consider steroidal anti-inflammatories (typically in the form of prednisone) in severe acute pain for a short period. A typical regimen is prednisone 60 to 80 mg/day for five days, which can then be slowly tapered off over the following 5 m to 14 days. Another regimen involves a prepackaged tapered dose of Methylprednisolone that tapers from 24 mg to 0 mg over 7 days.
- Non-steroidal anti-inflammatory drugs (NSAIDs) – These painkillers belong to the same group of drugs as acetylsalicylic acid (ASA, the drug in medicines like “Aspirin”). NSAIDs that may be an option for the treatment of sciatica include diclofenac, ibuprofen, and naproxen. Anti-inflammatory drugs are drugs that reduce inflammation. This includes substances produced by the body itself like cortisone. It also includes artificial substances like ASA – acetylsalicylic acid (or “aspirin”) or ibuprofen –, which relieve pain and reduce fever as well as reducing inflammation.
-
Acetaminophen (paracetamol) – Acetaminophen (paracetamol) is also a painkiller, but it is not an NSAID. It is well tolerated and can be used as an alternative to NSAIDs – especially for people who do not tolerate NSAID painkillers because of things like stomach problems or asthma. But higher doses of acetaminophen can cause liver and kidney damage. The package insert advises adults not to take more than 4 grams (4000 mg) per day. This is the amount in, for example, 8 tablets containing 500 milligrams each. It is not only important to take the right dose, but also to wait long enough between doses.
-
Opioids – Strong painkillers that may only be used under medical supervision. Opioids are available in many different strengths, and some are available in the form of a patch. Morphine, for example, is a very strong drug, while tramadol is a weaker opioid. These drugs may have a number of different side effects, some of which are serious.
- Skeletal Muscle relaxant – If muscle spasms are prominent, the addition of a muscle relaxant may merit consideration for a short period. For example, cyclobenzaprine is an option at a dose of 5 mg taken orally three times daily. Antidepressants (amitriptyline) and anticonvulsants (gabapentin and pregabalin) have been used to treat neuropathic pain, and they can provide a moderate analgesic effect.
-
Steroids – Anti-inflammatory drugs that can be used to treat various diseases systemically. That means that they are taken as tablets or injected. The drug spreads throughout the entire body to soothe inflammation and relieve pain. Steroids may increase the risk of gastric ulcers, osteoporosis, infections, skin problems, glaucoma, and glucose metabolism disorders.
-
Muscle relaxants – Sedatives which also relax the muscles. Like other psychotropic medications, they can cause fatigue and drowsiness, and affect your ability to drive. Muscle relaxants can also affect liver functions and cause gastro-intestinal complications. Drugs from the benzodiazepine group, such as tetrazepam, can lead to dependency if they are taken for longer than two weeks.
- Nerve Relaxant and Neuropathic Agents – Drugs(pregabalin & gabapentin) or Vitamin B1 B6, B12 and mecobalamin that address neuropathic—or nerve-related pain remover. This includes burning, numbness, and tingling.
-
Anticonvulsants – These medications are typically used to treat epilepsy, but some are approved for treating nerve pain (neuralgia). Their side effects include drowsiness and fatigue. This can affect your ability to drive.
- Antidepressants – These drugs are usually used for treating depression. Some of them are also approved for the treatment of pain. Possible side effects include nausea, dry mouth, low blood pressure, irregular heartbeat, and fatigue.
- Topical Medications – These prescription-strength creams, gels, ointments, patches, and sprays help relieve pain and inflammation through the skin.
- Calcium & vitamin D3 – to improve bone health and healing fracture. As a general rule, men and women age 50 and older should consume 1,200 milligrams of calcium a day, and 600 international units of vitamin D a day.
- Glucosamine & Diacerein, Chondroitin sulfate – can be used to tightening the loose tension, cartilage, ligament, and cartilage, ligament regenerate cartilage or inhabit the further degeneration of cartilage, ligament
- Injections – Injection therapy uses mostly local anesthetics and/or anti-inflammatory medications like corticosteroids (for example cortisone). These drugs are injected into the area immediately surrounding the affected nerve root.
Surgical and other procedures
If other methods haven’t relieved your pain, you doctor might suggest:
- Joint injections – Corticosteroids can be injected into the joint to reduce inflammation and pain. You can get only a few joint injections a year because the steroids can weaken your joint’s bones and tendons.
- Radiofrequency denervation – Radiofrequency energy can damage or destroy the nerve tissue causing your pain.
- Electrical stimulation – Implanting an electrical stimulator into the sacrum might help reduce pain caused by sacroiliitis.
- Joint fusion – Although surgery is rarely used to treat sacroiliitis, fusing the two bones together with metal hardware can sometimes relieve sacroiliitis pain.
Prevention
- A positive attitude, regular activity, and a prompt return to work are all very important elements of recovery. If regular job duties cannot be performed initially, modified (light or restricted) duty may be prescribed for a limited time.
Prevention is key to avoiding recurrence
References

![]()










About the author