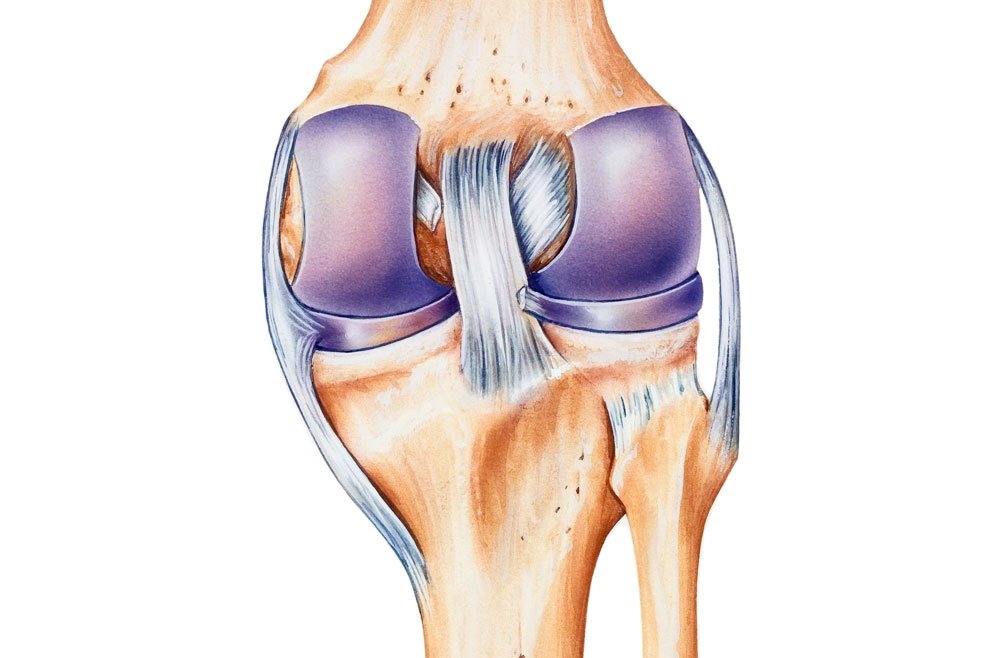
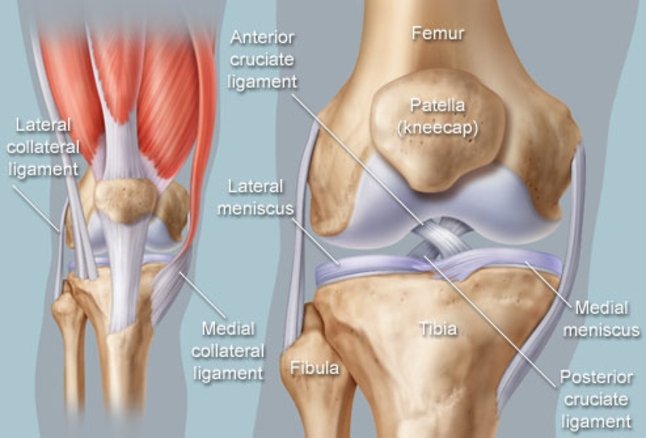
Knee Medial Collateral Ligament Injury (MCL) is a flat band of connective tissue that runs from the medial epicondyle of the femur to the medial condyle of the tibia. Its role is to provide valgus stability to the knee joint. MCL injuries often occur in sports, especially in skiing; in fact, 60% of skiing knee injuries involve the MCL. [rx][rx][rx]
Medial collateral ligament (MCL) injury is one of the most common knee injuries, especially in young athletic patients. Most MCL injuries can be managed conservatively with good results. However, a complete understanding of knee anatomy and the involved structures is necessary to make intelligent treatment decisions. We will review the anatomy and biomechanics of the MCL, classification systems for MCL injuries, and operative and nonoperative treatment for acute and chronic MCL injuries.
The tibial collateral ligament, also known as the medial collateral ligament (MCL), is a ligament extending from the medial epicondyle of the femur to the posteromedial crest of the tibia. The ligament is a broad and strong band that mainly functions to stabilize the knee joint in the coronal plane on the medial side.

Types of Knee Medial Collateral Ligament Injury
Doctors categorize MCL injuries according to the following criteria
- Grade I tear – This is a slight tear (or stretch) of the MCL. Both ends of the ligament are still attached to the bone, but a portion of the ligament may sag and be less taut. Recovery usually takes 1 to 2 weeks; therapy may not be needed.
- Grade II tear – This is a slightly more severe tear of the MCL, with a portion of the ligament sagging. Pain and swelling is usually more severe than with a grade I tear. Kids usually need 3 to 4 weeks of rest and sometimes therapy.
- Grade III tear – With this type of injury, the MCL breaks in half. Many kids are unable to bend the knee or bear weight on it without pain. They might be unstable while walking, and the knee may sometimes “give out.” Kids with this injury need to wear a knee brace and undergo rehab therapy for 6 weeks or longer.
Causes of Knee Medial Collateral Ligament Injury
MCL injuries are regularly seen in contact and non-contact sports and often occur in the following instances:
- Motor vehicle accidents – A “dashboard injury” occurs when the driver’s or passenger’s bent knee slams against the dashboard, pushing in the shinbone just below the knee and causing a tear.
- Contact sports – Athletes in sports such as football and soccer can tear their ligament when they fall on a bent knee with their foot pointed down. The shinbone hits the ground first and it moves backward. Being tackled when your knee is bent also can cause this injury.
- The knee is hit directly – especially during sports like soccer, rugby, and football
- A person lands on a bent knee – such as during a fall or misstep
- Landing directly on the front of the shinbone – such as when a dancer comes down from a leap and falls
- A person makes cutting or pivoting maneuvers – such as when an athlete plants a foot and shifts directions
- A person lands on one leg – which can happen after a jump in basketball or volleyball
- A direct blow to the bent knee in an automobile injury
- A sports-related injury in which the knee bends
- Pulling on the ligament in a twisting injury or hyperextension
- A misstep on uneven terrain
- When the knee is hit directly on its outer side, such as from a football tackle
- As a result of cutting maneuvers, when an athlete plants a foot and forcefully shifts direction
- Squatting or lifting heavy objects, such as weight lifting
- Landing awkwardly on the knee, such as when jumping in volleyball
- Hyperextending the knee, such as when skiing
- Through repeated stress to the knee, which causes the ligament to lose its elasticity (like a worn-out rubber band)
While sports injuries are the most common cause of MCL tears and sprains, any direct blow, such as during a car accident, can cause the ligament to be damaged.

Symptoms of Knee Medial Collateral Ligament Injury
A person who experiences an MCL injury typically reports a combination of the following symptoms:
- A “popping” sound – when the injury occurs. This sound is usually a sign of a grade II or grade III tear.
- Immediate sharp pain – from the inner section of the knee.
- Immediate swelling – at the inner knee. Swelling may increase and spread to the actual knee joint 1 or 2 days following the injury.
- Tenderness – around the inner knee. This area may be painful to the touch.
- Increased pain – a few hours after the injury.
- Bruising around the knee – especially around the location of the MCL (inner knee).
- Noticeable looseness – in the knee. A person may be able to feel looseness around the inner knee when walking. The knee may feel as if it has a greater range of motion than normal.
- Knee stiffness – may make walking, sitting down, rising from a chair or climbing stairs difficult. A person may have trouble bending or straightening the knee.
- The feeling of knee instability – may be particularly noticeable during activities that strain the knee, such as going downstairs or pivoting on one leg. The knee may feel as if it is about to give out. Instability is usually associated with more severe MCL tears.
- Pain when bearing weight – such as when walking, sitting down, or rising from a chair.
Diagnosis of Knee Medial Collateral Ligament Injury
Stage
The severity and symptoms of a knee ligament sprain depend on the degree of stretching or tearing of the knee ligament. You may notice an audible snap or tearing sound at the time of your ligament injury.
- In a mild, Grade I MCL sprain – the knee ligament has a slight stretch, but they don’t tear. Although the knee joint may not hurt or swell very much, a mild ligament sprain can increase the risk of a repeat injury.
- With a moderate Grade II MCL sprain – the knee ligament tears partially. Knee swelling and bruising are common, and the use of the knee joint is usually painful and challenging. You may have some complaints of instability or a feeling of the knee giving way.
With a severe Grade III MCL sprain – the ligament tears completely, causing swelling and sometimes bleeding under the skin. As a result, the joint is unstable and can be difficult to bear weight. You may have a feeling of the knee giving way. Often there will be no pain or severe pain that subsides quickly following a grade 3 tear as all of the pain fibers are torn at the time of injury. With these more severe tears, other structures are at risk of injury, including the meniscus or ACL.
Physical Exam
Testing of the knee joint should be done using the following techniques and the findings compared to the contralateral, normal knee:[rx][rx]
- Valgus stress at 0° and 20° – This test puts direct stress on the medial knee structures, reproducing the mechanism of injury. Valgus stress testing is done with the patient supine on the exam table. The lower extremity, supported by the examiner, is abducted. The examiner’s fingers monitor the medial joint space for gapping while placing the opposite hand on the ankle. The knee is placed in 20° of flexion. The examiner then uses their own thigh as a fulcrum at the knee and applies a valgus force (pulling the foot and ankle away from the patient’s body). The force is then used to establish the amount of gapping present within the joint. It has been reported that 20° of flexion is best for isolating the MCL, allowing the practitioner to establish the degree of injury (see Classification). Additional testing is done at 0° to determine if a Grade III injury is present.[rx][rx]
- Valgus stress testing – is the best way to test the integrity of the MCL directly. The patient should be positioned supine with the hip abducted on the affected side so that the leg is unsupported off the table. The knee should be brought into 30 degrees of flexion. The examiner should grasp the ankle with one hand and push the ankle laterally while applying a valgus force to the knee with the other hand.
- Anteromedial drawer test – This test is performed with the patient supine with the knee flexed to 80-90°. The foot is externally rotated 10-15° and the examiner supplies an anterior and external rotational force. The joint can then be evaluated for tibial anteromedial rotation, taking care to recognize the possibility of posterolateral corner instability giving similar rotational test results. As always, compare the test in the opposite knee.[rx][rx][rx]
- Dial Test (anteromedial rotation test) – This test should be executed with the patient lying both supine and prone. When the patient is supine, the knees must be flexed 30° off the table. The thigh is then stabilized and the foot externally rotated. The examiner watches for the tibial tubercle of the affected knee to rotate as the foot rotates, comparing it to the contralateral knee. A positive test will show the rotation of greater than 10-15° of rotation compared to the opposite knee. This is most easily assessed with a hand placed over the tibia while testing. When the patient is prone, the knee is flexed to 90° and both feet are externally rotated and compared, noting the difference from the non-injured joint. Similar to the anteromedial drawer test, a false positive test can result from a posterolateral corner injury. Testing at both 30° and 90° helps to distinguish between these injuries: one should monitor where the tibial rotation occurs (anteromedial or posterolateral) in the supine position and also assess for medial or lateral joint line gapping to differentiate between these two injuries.[rx][rx][rx]
Imaging Test
- X-rays – use low levels of radiation and give doctors a view of a person’s bones. Although MCL injuries do not show up on standard X-ray exams, they are a relatively inexpensive, fast way to rule out other possible injuries that might be causing the symptoms. Additionally, a stress X-ray—where a physician applies a valgus force to the knee during the exam—can help to determine the degree of ligamentous injury.
- Magnetic resonance imaging (MRI) – shows a detailed view of the soft tissue surrounding the knee joint. An MRI can also help a doctor determine the location and grade of an MCL tear.
- Ultrasound imaging – uses high-frequency sound waves to build a picture of the knee’s tissues. Ultrasound can be utilized in situations when an MRI is not recommended. Ultrasound may also be used in an urgent care setting to make an immediate assessment, allowing the injury to be treated more quickly.
Treatment of Knee Medial Collateral Ligament Injury
Nonsurgical
Most everyone who has an MCL injury will be advised by a health care professional to follow the RICE method:
- Rest – Activities that irritates the knee, such as pivoting and walking for long periods of time, should be avoided until the symptoms get better.
- Ice – A person may be advised to apply ice packs to the knee to help reduce swelling and decrease pain. Apply ice with a compressive wrap for 20 minutes and repeat every 3-4 hours for the first 24-48 hours.
- Compression – Wearing a tight, elastic bandage around the knee can help stop swelling.
- Elevation – Keeping the knee propped up above the waist can help decrease swelling.
- Wear a knee cap – that allows the knee to move forward and backward but restricts side-to-side movement. Apply minimally restrictive lateral hinge brace (grade II or III injuries).
- Use crutches – to avoid weight-bearing. Crutches are not needed in all cases. Dispense crutches; allow weight-bearing as tolerated.
- Bracing – Your knee must be protected from the same sideways force that caused the injury. You may need to change your daily activities to avoid risky movements. Your doctor may recommend a brace to protect the injured ligament from stress. To further protect your knee, you may be given crutches to keep you from putting weight on your
Medication
If the injury is severe and pain is intolerable the following medicine can be considered to prescribe
- Take anti-inflammatory medications – Non-steroidal anti-inflammatory drugs (NSAIDs), like will help with pain and swelling. However, these drugs can have side effects, such as an increased risk of bleeding and ulcers. They should be only used occasionally unless your doctor specifically says otherwise.
- Antibiotic – Cefuroxime or Azithromycin, or Flucloxacillin or any other cephalosporin/quinolone antibiotic must be used to prevent infection or clotted blood remove to prevent furthers swelling and edema.
- NSAIDs – Prescription-strength drugs that reduce both pain and inflammation. Pain medicines and anti-inflammatory drugs help to relieve pain and stiffness, allowing for increased mobility and exercise. There are many common over-the-counter medicines called non-steroidal anti-inflammatory drugs (NSAIDs). They include and Ketorolac, Aceclofenac, Naproxen, Etoricoxib.
- Corticosteroids – Also known as oral steroids, these medications reduce inflammation.
- Muscle Relaxants – These medications provide relief from associated muscle spasms.
- Neuropathic Agents – Drugs(pregabalin & gabapentin) that address neuropathic—or nerve-related—pain. This includes burning, numbness, and tingling.
- Opioids – Also known as narcotics, these medications are intense pain relievers that should only be used under a doctor’s careful supervision.
- Topical Medications – These prescription-strength creams, gels, ointments, patches, and sprays help relieve pain and inflammation through the skin.
- Calcium & vitamin D3 – to improve bone health and healing fracture. As a general rule, men and women age 50 and older should consume 1,200 milligrams of calcium a day, and 600 international units of vitamin D a day.
- Antidepressants – A drug that blocks pain messages from your brain and boosts the effects of endorphins (your body’s natural painkillers).
- Glucosamine & Diacerein, Chondroitin sulfate – can be used to tightening the loose tension, cartilage, ligament, and cartilage, ligament regenerates cartilage or inhabits the further degeneration of cartilage, ligament. They are structural components of articular cartilage, and the thought is that a supplement will aid in the health of articular cartilage.
- Intra-articular corticosteroid injections – may be useful for symptomatic injury especially where there is a considerable inflammatory component. The delivery of the corticosteroid directly into the knee may reduce local inflammation associated with injury and minimize the systemic effects of the steroid.
- Intra-articular hyaluronic acid injections (HA) – injections are another injectable option for a knee injury. HA is a glycosaminoglycan that is found throughout the human body and is an important component of synovial fluid and articular cartilage. HA breaks down during the process of ligament injury and contributes to the loss of articular cartilage as well as stiffness and pain. Local delivery of HA into the joint acts as a lubricant and may help increase the natural production of HA in the joint.
- Platelet-rich plasma (PRP) injection – newer therapy where a blood sample is taken from the patient, spun in a centrifuge, growth factors are isolated and then they are injected back into the affected site to stimulate faster healing.
Surgery
- Knee arthroscopy – minimally invasive surgical procedure to diagnose and repair an MCL injury; small incisions are made in the knee and a camera is inserted to visualize the injury and determine treatment.
Physiotherapy
Depending on the grade of injury, you can start to feel better within days to just a few weeks of the damage. Your physiotherapy treatment will aim to:
- Reduce pain and inflammation.
- Normalize joint range of motion.
- Strengthen your knee: esp quadriceps (esp VMO) and hamstrings.
- Strengthen your lower limb: calves, hip and pelvis muscles.
- Improve patellofemoral (knee cap) alignment
- Normalize your muscle lengths
- Improve your proprioception, agility and balance
- Improve your technique and function, e.g. walking, running, squatting, hopping and landing.
- Guide return to sports activities and exercises
- Minimize your chance of re-injury.
Exercises
A physical therapist will be able to advise on strengthening exercises to aid recovery after an MCL tear. Some possible exercises may include:
Exercise to restore range of motion and increase strength. These exercises typically include gentle stretches and strengthening exercises. People may also do upper body workouts and swim in order to keep up general conditioning. Some people may work with a physical therapist for guided treatment.
1. Hamstring curl
- Stand up straight, engaging the stomach muscles.
- Stand on one leg and slowly bend the opposite knee by bringing the heel up toward the buttocks.
- Hold for 30 seconds before repeating on the other side of the body.
- A person can hold on to a chair or table for support if needed.
2. Wall slide
- Standing up straight, with both feet flat on the ground, place the back firmly against a wall.
- Slowly slide down, keeping the back against the wall until reaching a squatting position.
- Hold for 30 seconds.
- Push up from the feet to stand up, keeping the back flat against the wall.
- Repeat 10 to 15 times.
3. Chair squat
- Standing on one leg, slowly squat toward sitting down onto a chair.
- Return to a standing position, again standing on one leg.
- Bend at the waist and keep the body in a straight line when standing.
- A person may need to build up to sitting fully on the chair
Subsequent treatment
- Begin active range-of-motion exercises in cold whirlpool at least twice daily.
- Begin straight-leg raises and electrical muscle stimulation (if available).
- Maintain general conditioning with upper body ergometer or swimming.
Goal one: Walking unassisted without a limp
- Discard crutches.
- Continue range of motion, isometric strengthening, and conditioning exercises.
Goal two: 90 degrees of knee flexion
- Begin stair climber and bicycle ergometer with seat high; gradually lower seat.
- Begin isotonic progressive restrictive exercise for quadriceps and hamstrings; supplement with isokinetic exercise if available.
- Continue range of motion and conditioning exercises.
Goal Three: Full knee motion
- Begin running and functional exercise program.
- For example:
-
Jog 1 mile.
-
Five successive 100-yard sprints at half speed.
-
Five successive 100-yard sprints at three-quarters speed.
-
Five successive 100-yard sprints at full speed.
-
Five zigzag sprints at half speed.
-
Five zigzag sprints at full speed.
-
- Other agility drills (e.g. Cariocas).
- Continue conditioning.
Goal four: Complete entire running program in one session
- May return to competition if the athlete has minimal pain, full range of motion, and 90 percent of normal strength.
- Continue to use a brace for all sports participation for the remainder of the season.[rx]
Rehabilitation
The rehabilitation for a non-operative treatment can be split into four phases:
- Phase one is from one to two weeks. Phase one consists of controlling the swelling of the knee by applying ice for 15 minutes every two hours (first two days). The rest of the week the frequency can be reduced to three times a day. Use ice as tolerated and as needed based on symptoms. In the begin, the patient needs to use crutches. Early weight bearing is encouraged because patients who increasing their weight-bearing, they can progressively reduce their dependence on crutches. Afterward, progress to one crutch and let the patient stop using the crutches only when normal gait is possible. Another aim of this phase is to try to maintain the ability to straighten and bend the knee from 0° to 90° knee flexion. For achieving the range of motion of the knee it is important to emphasize full extension and progress flexion as tolerated. Pain-free stretches for the hamstrings, quads, groin and calf muscles (in particular) are suggested. At last, there are therapeutic exercises. The patient may begin with static strengthening exercises (as soon as pain allows it). They consist for example of Quadricpes sets, straight leg raises, range-of-motion exercises, sitting hip flexion, side-lying hip abduction, standing hip extension, standing, and hamstring curls. As soon as patients can tolerate it, they are encouraged to ride a stationary bike to improve the range of motion of the knee. This would ensure accelerated healing. The amount of time and effort on the stationary bike is increased as tolerated. Obviously, every patient is different and these are not the standard exercises that have to be given to patients. There are no limits on upper extremity workouts that do not affect the injured knee[rx]. It’s important that the patient rests from all painful activities (use crutches if necessary), and that the MCL is well protected (by wearing a stabilized knee brace).
- Starting at week three-phase two begins – The aims for the range of motion are the same as in phase one. Progress to 20 minutes of biking. Increase also the resistance as tolerated by the patient. Biking will ensure healing, rebuild strength, and maintain aerobic conditioning. The physiotherapist can give other exercises like Hamstring curls, leg presses (double-leg), and step-ups. As a precaution, the patient has the chance to be examined by a physician every three weeks to verify the healing of the ligament[rx].
- Phase three starts from week five – A major goal for this phase: full weight-bearing on the injured knee. Discontinue the use of a brace when ambulating with full weight-bearing is possible and there is no gait deviation. The range of motion has to be fully achieved and had to be symmetrical with the not injured knee. The therapeutic exercises are the same as in phase two. They may benefit progression. We continue with cold therapy and compression to eliminate swelling. In this phase, you can commence with balance and proprioceptive activities. To maintain aerobic fitness the patient can use the stepper or (if possible) may begin to swim. As a precaution, the patient has the chance to be examined by a physician every five to six weeks. When needed, you can be allowed to make stress radiography as a precaution.[rx]
- Six weeks after injuring the knee, phase four can begin – Discontinue wearing the brace during the gait. Athletics can wear the brace for competition through the competitive season for at least three months. Cold therapy still needs to be applied. The aim of the therapeutic exercises is more focused on sport-specific or daily movements. The intensity of the strengthening exercises needs to be increased and instead of double leg exercises, we change to single-leg exercises. The patient may start running again at a comfortable pace (make sure the patient doesn’t make sudden changes of direction). As a precaution, it is best to return the competition once full motion and strength is returned and when the patient passes a sport functional test[rx].
How to do the exercises
Knee flexion with heel slide

slide 1 of 10, Knee flexion with heel slide,
- Lie on your back with your knees bent.
- Slide your heel back by bending your affected knee as far as you can. Then hook your other foot around your ankle to help pull your heel even farther back.
- Hold for about 6 seconds, then rest for up to 10 seconds.
- Repeat 8 to 12 times.
Heel slides on a wall

slide 2 of 10, Heel slides on a wall,
- Lie on the floor close enough to a wall so that you can place both legs up on the wall. Your hips should be as close to the wall as is comfortable for you.
- Start with both feet resting on the wall. Slowly let the foot of your affected leg slide down the wall until you feel a stretch in your knee.
- Hold for 15 to 30 seconds.
- Then slowly slide your foot up to where you started.
- Repeat 2 to 4 times.
Quad sets

slide 3 of 10, Quad sets,
- Sit with your affected leg straight and supported on the floor or a firm bed. Place a small, rolled-up towel under your knee. Your other leg should be bent, with that foot flat on the floor.
- Tighten the thigh muscles of your affected leg by pressing the back of your knee down into the towel.
- Hold for about 6 seconds, then rest for up to 10 seconds.
- Repeat 8 to 12 times.
Short-arc quad

slide 4 of 10, Short-arc quad,
- Lie on your back with your knees bent over a foam roll or a large rolled-up towel.
- Lift the lower part of your affected leg and straighten your knee by tightening your thigh muscle. Keep the bottom of your knee on the foam roll or rolled-up towel.
- Hold your knee straight for about 6 seconds, then slowly bend your knee and lower your leg back to the floor. Rest for up to 10 seconds between repetitions.
- Repeat 8 to 12 times.
Straight-leg raises to the front

slide 5 of 10, Straight-leg raises to the front,
- Lie on your back with your good knee bent so that your foot rests flat on the floor. Your affected leg should be straight. Make sure that your low back has a normal curve. You should be able to slip your hand in between the floor and the small of your back, with your palm touching the floor and your back touching the back of your hand.
- Tighten the thigh muscles in your affected leg by pressing the back of your knee flat down to the floor. Hold your knee straight.
- Keeping the thigh muscles tight and your leg straight, lift your affected leg up so that your heel is about 30 centimeters off the floor. Hold for about 6 seconds, then lower slowly.
- Relax for up to 10 seconds between repetitions.
- Repeat 8 to 12 times.
Hamstring set (heel dig)
slide 6 of 10, Hamstring set (heel dig),
- Sit with your affected leg bent. Your good leg should be straight and supported on the floor.
- Tighten the muscles on the back of your bent leg (hamstring) by pressing your heel into the floor.
- Hold for about 6 seconds, then rest for up to 10 seconds.
- Repeat 8 to 12 times.
Hip adduction

slide 7 of 10, Hip adduction,
- Sit on the floor with your knees bent.
- Place a pillow between your knees.
- Put your hands slightly behind your hips for support.
- Squeeze the pillow by tightening the muscles on the inside of your thighs.
- Hold for 6 seconds, then rest for up to 10 seconds.
- Repeat 8 to 12 times.
Hip abduction

slide 8 of 10, Hip abduction,
- Sit on the floor with your affected knee close to a wall.
- Bend your affected knee but keep the other leg straight in front of you.
- Place a pillow between the outside of your knee and the wall.
- Put your hands slightly behind your hips for support.
- Push the outside of your knee against the pillow and the wall.
- Hold for 6 seconds, then rest for up to 10 seconds.
- Repeat 8 to 12 times.
Lateral step-up

slide 9 of 10, Lateral step-up,
- Stand sideways on the bottom step of a staircase with your injured leg on the step and your other foot on the floor. Hold on to the banister or wall.
- Use your injured leg to raise yourself up, bringing your other foot level with the stair step. Make sure to keep your hips level as you do this. And try to keep your knee moving in a straight line with your middle toe. Do not put the foot you are raising on the stair step.
- Slowly lower your foot back down.
- Repeat 8 to 12 times.
Wall squats with ball

slide 10 of 10, Wall squats with ball,
- Stand with your back facing a wall. Place your feet about a shoulder-width apart.
- Place the therapy ball between your back and the wall, and move your feet out in front of you so they are about 30 centimetres in front of your hips.
- Keep your arms at your sides, or put your hands on your hips.
- Slowly squat down as if you are going to sit in a chair, rolling your back over the ball as you squat. The ball should move with you but stay pressed into the wall.
- Be sure that your knees do not go in front of your toes as you squat.
- Hold for 6 seconds.
- Slowly rise to your standing position.
- Repeat 8 to 12 times.
How do I get ready for a knee ligament repair?
- Your healthcare provider will explain the procedure to you and offer you the chance to ask any questions that you might have about the procedure.
- You will be asked to sign a consent form that gives your permission to do the procedure. Read the form carefully and ask questions if something is not clear.
- In addition to a complete medical history, your healthcare provider may perform a complete physical exam to ensure you are in good health before undergoing the procedure. You may undergo blood tests or other diagnostic tests.
- Tell your healthcare provider if you are sensitive to or are allergic to any medicines, latex, tape, and anesthetic agents (local and general).
- Tell your healthcare provider of all medicines (prescribed and over-the-counter) and herbal supplements that you are taking.
- Tell your healthcare provider if you have a history of bleeding disorders or if you are taking any anticoagulant (blood-thinning) medicines, aspirin, or other medicines that affect blood clotting. It may be necessary for you to stop these medicines before the procedure.
- If you are pregnant or suspect that you are pregnant, you should notify your healthcare provider.
- You will be asked to fast for 8 hours before the procedure, generally after midnight.
- You may receive a sedative prior to the procedure to help you relax. Because the sedative may make you drowsy, you will need to arrange for someone to drive you home.
- You may meet with a physical therapist prior to your surgery to discuss rehabilitation.
- Arrange for someone to help around the house for a week or two after you are discharged from the hospital.
- Based on your health condition, your healthcare provider may request other specific preparations.
What happens during a knee ligament repair?
Knee ligament repair may be done on an outpatient basis or rarely as part of your stay in a hospital. Procedures may vary depending on your condition and your healthcare provider’s practices.
Knee ligament repair may be performed while you are asleep under general anesthesia, or while you are awake under spinal anesthesia. If spinal anesthesia is used, you will have no feeling from your waist down. Your healthcare provider will discuss this with you in advance.
Generally, knee ligament repair surgery follows this process:
- You will be asked to remove clothing and will be given a gown to wear.
- An intravenous (IV) line may be started in your arm or hand.
- You will be positioned on the operating table.
- The anesthesiologist will continuously monitor your heart rate, blood pressure, breathing, and blood oxygen level during the surgery.
- The skin over the surgical site will be cleansed with an antiseptic solution.
- The healthcare provider will make several small incisions in the knee area.
- The healthcare provider will do the surgery using an arthroscope (a small tube-shaped instrument that is inserted into a joint). The healthcare provider may reattach the torn ligament or reconstruct the torn ligament by using a portion (graft) of the patellar tendon (that connects the kneecap to the tibia), the hamstring tendon (from the back of the thigh), or other autografts. The tendon graft may come from the person (autograft) or from an organ donor (allograft).
- The healthcare provider will drill small holes in the tibia and femur where the torn ligament was attached.
- The healthcare provider will thread the graft through the holes and attach it with surgical staples, screws, or other
means. Bone eventually grows around the graft. - The incision will be closed with stitches or surgical staples.
- A sterile bandage or dressing will be applied.
What happens after a knee ligament repair?
After the surgery, you will be taken to the recovery room for observation. Your recovery process will vary depending on the type of anesthesia that is given. Once your blood pressure, pulse, and breathing are stable and you are alert, you will be taken to your hospital room or discharged to your home. Knee ligament repair is usually done on an outpatient basis.
You may be given crutches and a knee immobilizer before you go home.
Once you are home, it is important to keep the surgical area clean and dry. Your healthcare provider will give you specific bathing instructions. The stitches or surgical staples will be removed during a follow-up office visit.
Take a pain reliever for soreness as recommended by your healthcare provider. Aspirin or certain other pain medicines may increase the chance of bleeding. Be sure to take only recommended medicines.
To help reduce swelling, you may be asked to elevate your leg and apply an ice bag to the knee several times per day for the first few days. Your healthcare provider will arrange for an exercise program to help you regain muscle strength, stability, and range of motion. Physical therapy is a key part of recovery.
Tell your healthcare provider if you have any of the following:
- Fever or chills
- Redness, swelling, bleeding, or another drainage from the incision site
- Increased pain around the incision site
- Numbness or tingling in the leg
- Calf swelling or tenderness
You may resume your normal diet unless your healthcare provider advises you differently.
Because of the limited mobility, it may be hard for a few weeks to resume your normal daily activities. You may need someone at home to assist you. You should not drive until your healthcare provider tells you to. Other activity restrictions may apply. Full recovery from the surgery and rehab may take several months.
Your healthcare provider may give you additional or alternate instructions after the procedure, depending on your particular situation.
Next steps
Before you agree to the test or the procedure make sure you know:
- The name of the test or procedure
- The reason you are having the test or procedure
- What results to expect and what they mean
- The risks and benefits of the test or procedure
- What the possible side effects or complications are
- When and where you are to have the test or procedure
- Who will do the test or procedure and what that person’s qualifications are
- What would happen if you did not have the test or procedure
- Any alternative tests or procedures to think about
- When and how you will get the results
- Who to call after the test or procedure if you have questions or problems
- How much you will have to pay for the test or procedure
References
![]()