Spirometry is a simple test used to help diagnose and monitor certain lung conditions by measuring how much air you can breathe out in one forced breath. It’s carried out using a device called a spirometer, which is a small machine attached by a cable to a mouthpiece.
Spirometry is one of the most commonly used approaches to test pulmonary function. It measures the volume of exhaled air vs. time. This activity highlights its role in the evaluation of pulmonary disease by the interprofessional team.
Spirometry is one of the most readily available and useful tests for pulmonary function. It measures the volume of air exhaled at specific time points during complete exhalation by force, which is preceded by a maximal inhalation.
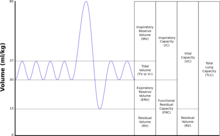
The most important variables reported include total exhaled volume, known as the forced vital capacity (FVC), the volume exhaled in the first second, known as the forced expiratory volume in one second (FEV1), and their ratio (FEV1/FVC).[rx] These results are represented on a graph as volumes and combinations of these volumes termed capacities and can be used as a diagnostic tool, as a means to monitor patients with pulmonary diseases and to improve the rate of smoking cessation according to some reports.[rx]
Anatomy and Physiology
Lungs provide life-sustaining gas exchange by way of introducing oxygen for metabolism and eliminating the by-product carbon dioxide. Air-inspired will pass through the oropharynx to the trachea, which is a membranous tube covered by cartilage bifurcating at the carina as two bronchi at the level of C6. After passing the trachea, the air enters the right and left bronchi, which divide to give several million terminal bronchioles that end in alveoli. The alveoli and surrounding vessels provide a surface where the gas exchange takes place.[rx]
Indications
Apart from being a key diagnostic test for asthma and chronic obstructive pulmonary disease, spirometry in indicated in several other places, as listed below:
Diagnostic Indications
-
Evaluation of the signs and symptoms of a patient or their abnormal investigations and lab tests
-
Evaluation of the effect a certain disease has on pulmonary function
-
Screening and early detection of individuals who are at risk of pulmonary disease
-
Assessing surgical patients for preoperative risk
-
Assessing the severity and the prognosis of pulmonary disease[rx]
Monitoring Indications
-
Assessment of the efficiency of a therapeutic intervention such as bronchodilator therapy
-
Describing the course and progression of a disease that is affecting pulmonary function such as interstitial lung disease or obstructive lung disease
-
Monitoring pulmonary function in individuals with high-risk jobs
-
Sampling data that can be used for epidemiologic surveys[rx]
Spirometry is indicated for the following reasons
- to diagnose or manage asthma[rx][rx][rx]
- to detect respiratory disease in patients presenting with symptoms of breathlessness, and to distinguish respiratory from cardiac disease as the cause[rx]
- to measure bronchial responsiveness in patients suspected of having asthma[rx]
- to diagnose and differentiate between obstructive lung disease and restrictive lung disease[rx]
- to follow the natural history of disease in respiratory conditions[rx]
- to assess impairment from occupational asthma[rx]
- to identify those at risk from pulmonary barotrauma while scuba diving[rx]
- to conduct a pre-operative risk assessment before anesthesia or cardiothoracic surgery[rx]
- to measure response to treatment of conditions which spirometry detects[5]
- to diagnose the vocal cord dysfunction.
Contraindications
Spirometry has proved itself as an accessible utility to assess lung function. However, it may not be for every patient, and care must be taken in some cases, where it may be absolutely or relatively contraindicated.
Absolute Contraindications
-
Hemodynamic instability
-
Recent myocardial infarction or acute coronary syndrome
-
Respiratory infection, a recent pneumothorax or a pulmonary embolism
-
A growing or large (>6 cm) aneurysm of the thoracic, abdominal aorta
-
Hemoptysis of acute onset
-
Intracranial hypertension
-
Retinal detachment
- Hemoptysis of unknown origin
- Pneumothorax
- Unstable cardiovascular status (angina, recent myocardial infarction, etc.)
- Thoracic, abdominal, or cerebral aneurysms
- Cataracts or recent eye surgery
- Recent thoracic or abdominal surgery
- Nausea, vomiting, or acute illness
- Recent or current viral infection
- Undiagnosed hypertension
Relative Contraindications
-
Patients who cannot be instructed to use the device properly and are at risk of using the device inappropriately such as children and patients with dementia
-
Conditions that make it difficult to hold the mouthpiece such as facial pain
-
Recent abdominal, thoracic, brain, eye, ear, nose or throat surgeries
Equipment
The first requirement for spirometry is physical space in order for the patient to be positioned comfortably. The minimum space recommended is a 2.5* 3m room with 120 cm side doors.
Spirometers are classified into closed-circuit and open-circuit spirometers. Closed-circuit spirometers are further sub-classified into wet and dry spirometers, which consist of a piston or a bellow acting as an air collecting system and a supported recording system that moves at the desired rate.
Open-circuit spirometers, which are more commonly used at present, do not have an air collecting system and instead measure the airflow, integrate the results, and calculate the volume. The most commonly used open-circuit spirometer is the turbine flow meter, which records the rate at which turbines turn and derives the flow measurement based on proportionality. Pneumotachographs are another example, which measures the airflow by measuring the pressure difference generated as the laminar flow passes through a certain resistance. Hotwire spirometers, in which a hot metal wire is heated, and the air used to cool it is used to calculate the flow, are also an example of open-circuit spirometers. Ultrasound spirometers can be based on any of the aforementioned open-circuit spirometer principles.[rx]
The minimum specifications for a spirometer are the ability to measure a volume of 8L with an accuracy of ±3% or ±50ml with a flow measurement range of ±141 and a sensitivity of 200ml/s. It is recommended that the spirometer can record at 15 s of the expiration time for the forced maneuver.[rx][rx]
Personnel
The personnel performing the procedure must be familiar with respiratory symptoms and signs. They have to undergo training to understand the technical and physiological background of the tests in order to be competent in performing the techniques of the operation of the device, be able to apply the universal precautions, instruct the patients properly to avoid complications, and act accordingly if any of the complications arise. The personnel should be able to identify responses to therapy, the need for initiating therapy or discontinuing an inefficient one. Continuity of training and periodic retraining is a must for staff in charge of spirometry.[rx]
Preparation
All patients must be informed that they must abstain from smoking, physical exercise in the hours before the procedure. Any bronchodilator therapy must also be stopped beforehand.
The procedure must be carefully explained to the patient focusing on the importance of the patient’s cooperation to provide the most accurate results. The patient’s weight and height must be recorded with the patient barefoot and wearing only light clothing. In the case of chest deformities such as kyphoscoliosis, the span should be measured from the tip of one middle finger to the tip of the other middle finger with the hands crossed, and the height can be estimated from the formula: height = span/1.06. The patient’s age must be recorded. The procedure should be performed with the patient sitting upright wearing light clothing and without crossing their legs. Children can perform the test sitting or standing, but the same procedure should be carried out for the same individual every time.
During the procedure, the back must be supported by a backrest and must not lead forward. Dentures have to be removed if they interfere with the procedure. Manual occlusion of the nares with the help of nose clips helps to prevent air leakage through the nasal passages, although it is not mandatory to occlude nasal passages. The calibration of the spirometer has to be confirmed on the day of the test.
Any contraindications or infectious diseases that require special measures will lead to a delay in the procedure.[rx][rx][rx]
Patient positioning
Correct measurement posture is as follows.
- Sit upright: there should be no difference in the amount of air the patient can exhale from a sitting position compared to a standing position as long as they are sitting up straight and there are no restrictions.
- Feet flat on the floor with legs uncrossed: no use of abdominal muscles for leg position.
- Loosen tight-fitting clothing: if clothing is too tight, this can give restrictive pictures on spirometry (give lower volumes than are true).
- Dentures normally left in: it is best to have some structure to the mouth area unless dentures are very loose.
- Use a chair with arms: when exhaling maximally, patients can become light-headed and possibly sway or faint.
Infection control
Hands must be washed between patients. Bacterial–viral filters should be used for all patients and thrown away by the patient at the end of testing. If an infectious patient requires testing, this should be performed at the end of the session and the equipment should be stripped down and sterilized/parts replaced (depending on what is being used) before being used again.
Technique
The patient must place the mouthpiece in their mouth, and the technician must ensure that there are no leaks, and the patient is not obstructing the mouthpiece. The procedure is carried out as follows:
- The patient must breathe in as much air as they can with a pause lasting for less than 1s at the total lung capacity.
-
The mouthpiece is placed just inside the mouth between the teeth, soon after the deep inhalation. The lips should be sealed tightly around the mouthpiece to prevent air leakage. Exhalation should last at least 6 seconds, or as long as advised by the instructor. If only the forced expiratory volume is to be measured, the patient must insert the mouthpiece after performing step 1 and must not breathe from the tube.
-
If any of the maneuvers are incorrectly performed, the technician must stop the patient in order to avoid fatigue and re-explain the procedure to the patient.
Complications
The complications of spirometry are fairly limited and will render the procedure as inaccurate or ineffective once they occur. They include:[rx][rx][rx]
-
Respiratory alkalosis as a result of hyperventilation
-
Hypoxemia in a patient whose oxygen therapy has been interrupted
-
Chest pain
-
Fatigue
-
Paroxysmal coughing
-
Bronchospasm
-
Dizziness
-
Urinary incontinence
-
Increased intracranial pressure
-
Syncopal symptoms
|
Flow-Volume loop showing successful FVC maneuver. Positive values represent expiration, negative values represent inspiration. At the start of the test both flow and volume are equal to zero (representing the volume in the spirometer rather than the lung). The trace moves clockwise for expiration followed by inspiration. After the starting point the curve rapidly mounts to a peak (the peak expiratory flow). (Note the FEV1 value is arbitrary in this graph and just shown for illustrative purposes; these values must be calculated as part of the procedure).
|
|
| MeSH | D013147 |
|---|---|
| OPS-301 code | 1-712 |
 |
|
| TLC | Total lung capacity: the volume in the lungs at maximal inflation, the sum of VC and RV. |
|---|---|
| TV | Tidal volume: that volume of air moved into or out of the lungs during quiet breathing (TV indicates a subdivision of the lung; when tidal volume is precisely measured, as in gas exchange calculation, the symbol TV or VT is used.) |
| RV | Residual volume: the volume of air remaining in the lungs after a maximal exhalation |
| ERV | Expiratory reserve volume: the maximal volume of air that can be exhaled from the end-expiratory position |
| IRV | Inspiratory reserve volume: the maximal volume that can be inhaled from the end-inspiratory level |
| IC | Inspiratory capacity: the sum of IRV and TV |
| IVC | Inspiratory vital capacity: the maximum volume of air inhaled from the point of maximum expiration |
| VC | Vital capacity: the volume of air breathed out after the deepest inhalation. |
| VT | Tidal volume: that volume of air moved into or out of the lungs during quiet breathing (VT indicates a subdivision of the lung; when tidal volume is precisely measured, as in gas exchange calculation, the symbol TV or VT is used.) |
| FRC | Functional residual capacity: the volume in the lungs at the end-expiratory position |
| RV/TLC% | Residual volume expressed as a percent of TLC |
| VA | Alveolar gas volume |
| VL | The actual volume of the lung including the volume of the conducting airway. |
| FVC | Forced vital capacity: the determination of the vital capacity from a maximally forced expiratory effort |
| FEVt | Forced expiratory volume (time): a generic term indicating the volume of air exhaled under forced conditions in the first t seconds |
| FEV1 | The volume that has been exhaled at the end of the first second of forced expiration |
| FIFA | Forced expiratory flow related to some portion of the FVC curve; modifiers refer to the amount of FVC already exhaled |
| FEFmax | The maximum instantaneous flow achieved during an FVC maneuver |
| FIF | Forced inspiratory flow: (Specific measurement of the forced inspiratory curve is denoted by nomenclature analogous to that for the forced expiratory curve. For example, maximum inspiratory flow is denoted FIFmax. Unless otherwise specified, volume qualifiers indicate the volume inspired from RV at the point of measurement.) |
| PEF | Peak expiratory flow: The highest forced expiratory flow measured with a peak flow meter |
| MVV | Maximal voluntary ventilation: volume of air expired in a specified period during repetitive maximal effort |
![]()

About the author